“Diabetic patients, despite current therapies, have significant residual risk of cardiovascular events such that we need to think about new agents,” said Professor Mark Kearney (University of Leeds) in a review of the increased pernicious nature of ischaemic heart disease (IHD) in the setting of type 2 diabetes.
He said that it was heartening to see that there has been a significant improvement in cancer survival rates over the past three decades in the UK. Using the cancer analogy, he said that “stable angina in patients with diabetes might be described as a “pre-malignant condition”; once angina becomes unstable, “it becomes malignant”.
Diabetes starts very early in life, with insulin resistance. As this progresses, there is an initial compensatory increase in plasma insulin, re-setting glucose at normal levels, but “ultimately the pancreas fails” with a resulting increase in blood glucose. All the time during this process, the blood vessel is exposed “to a portfolio of risk factors” that changes the artery. By the time the diabetic patient presents with an MI, the atherosclerotic phenotype and the prognosis are very different in comparison to those of a non-diabetic patient presenting with an MI.
Coronary artery disease is characterised by a series of changes within the arterial wall that culminates in plaque rupture. An early step in this process is endothelial dysfunction, which is characterised by a reduction in nitric oxide (NO), a change which occurs before there are any physical changes within the artery, Professor Kearney explained. This can be measured in a number of ways, including blood flow in the forearm after occlusion and release of a blood pressure cuff, ie. flow-mediated dilatation (FMD), detected by ultrasound. This can be equated to the amount of NO that an individual produces. These techniques have been used to study vascular function and to form a model of insulin resistance in young Asian men, confirming the presence of early atherosclerosis– “biochemical atherosclerosis, which we think is linked to insulin resistance”.
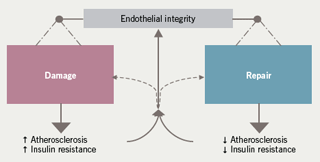
Asian males in the UK are three times more likely to die from an acute MI than European males and their post-MI mortality is worse, although we really do not understand why. Conventional risk factors, while important, do not account for all of this risk and there is a residual risk that is poorly understood. Progressive insulin resistance and glucose intolerance may play an important pathophysiological role in this process. Professor Kearney described a study he and co-workers have undertaken, ( Murphy C et al. Arterioscler Thromb Vasc Biol 2007;27:936–42) that examined differences in risk factors, vascular function and circulating endothelial progenitor cells among 24 young South Asian men and 25 age-matched, healthy, non-smoking Caucasian men. They looked at the balance between damage to the artery, caused by atherosclerosis and insulin resistance, and other cardiovascular risk factors, and endothelial repair, in the form of endothelial circulating progenitor cells (EPCs) which home in to sites of damage and can repair such damaged arteries (figure 1).
Risk factors between the two groups of men were very similar. The Asian men had normal fasting glucose levels but their fasting insulin and HOMA (a measure of insulin resistance) were significantly greater than in the Caucasian men, “showing that they have compensated insulin resistance”. Looking at endothelial function with FMD and forearm blood flow, these young Asian men also “had good evidence of a reduction in nitric oxide production, even at the age of 25. I put it to you that this is early atherosclerosis,” said Professor Kearney. Both the numbers and colonies of EPCs and their function were also reduced, indicating “impaired repair systems”.
Further along this paradigm, Professor Kearney’s group have also investigated determinants of endothelial function in 100 asymptomatic subjects with and without the metabolic syndrome, “the central core of which is insulin resistance and glucose intolerance” (Melikian N et al. Atherosclerosis 2008;197:375–82). Those with the metabolic syndrome still had normoglycaemia but they had an increase in fasting glucose, increased fasting insulin and a doubling of the HOMA index: that is, “they had worsening glucose control”. Similarly, endothelial function in this group was worse that that seen in the study of young Asian men, and they are starting to exhibit systemic inflammation and other markers of vascular/metabolic dysfunction, and a worsening of atherosclerosis.
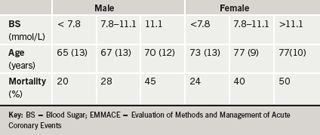
Professor Kearney described the effect of diabetes on outcomes after coronary events, looking at patients with impaired glucose tolerance (IGT) compared to patients with overt diabetes after MI. He presented data looking at new-onset hyperglycaemia following MI, as part of the EMMACE (Evaluation of Methods and Management of Acute Coronary Events) Study Group (Cubbon RM et al. Eur J Cardiovasc Preven Rehab 2007;14:666–71). Post-MI patients in 12 Yorkshire hospitals were followed up in EMMACE 1 (three months in 1995; n=1,770) and EMMACE 2 (six months during 2003; n=1,542) for 18 months overall to determine treatment effects. In women admitted to hospitals in 2003, the mortality associated with blood sugar > 11.1 mmol/L was 50% (table 1). When compared with stage III carcinoma of the breast, a woman with diabetes post-MI has a survival rate which is three years shorter. “I do not intend to trivialise carcinoma of the breast but this puts into perspective the need for new therapies in patients with diabetes and coronary artery disease,” said Professor Kearney.
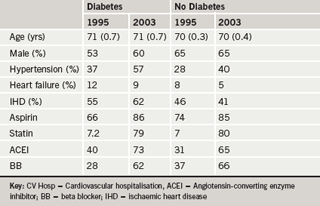
How have new therapies, introduced over the past 10 years, impacted on outcomes following MI? The two EMMACE 1 and EMMACE 2 databases have been examined to try and answer this (Cubbon RM et al. Eur Heart J 2007;128:540–45). The characteristics and treatments of the patients with and without diabetes in 1995 and 2003 are shown in table 2. “These secondary prevention therapies after myocardial infarction are very good,” with 86% of diabetic patients receiving aspirin in 2003 versus 66% in 1995, for example. How did this translate into outcomes? Two-year mortality among non-diabetic patients in 1995 was about 30%; in 2003, this was reduced by about an absolute percentage of 6% and a relative reduction of about 20%. Despite contemporary therapies and increased use of statins, aspirin, ACE inhibitors and beta blockers, mortality in diabetic patients remains “totally unchanged over the last ten years”.
To explore this further, Professor Kearney and colleagues have looked at responses to therapies (Cubbon RM et al. Diabetes Care 2008;31:363–5).They quantified the effects of different agents in diabetic and non-diabetic patients. Conventional agents such as beta blockers, ACE inhibitors and statins have very similar effects in diabetics and non-diabetics: “they all have a beneficial effect on mortality in the two groups, but aspirin seems not to have as good an effect”.
Outcomes remain poor in diabetes
Summarising the presentation, Professor Kearney said that “the pathology of diabetic coronary artery disease is different, despite the use of contemporary therapies. There is no doubt that even now, in 2008, outcomes for patients with diabetes after myocardial infarction are very poor. Contemporary therapies help these patients but they do not address all of the risk that these patients have. And we really need to assess new agents to address this residual risk that is not addressed by current therapies”.
Asked whether the glitazones may have a role in acute coronary syndromes (ACS), Professor Kearney said that there are controversies about these agents. There is no evidence for the two marketed agents in ACS, but in stable coronary disease there is evidence that pioglitazone has a favourable effect on mortality. In the context of stable coronary disease, diabetes and poor glycaemic control, pioglitazone does have a place, but whether it actually affects the pathophysiology of the arterial wall is a debate which is still ongoing, in his view. He commented also on the controversial findings from the Diabetes Mellitus Insulin-Glucose Infusion in Acute Myocardial Infarction-2 trial (DIGAMI-2), which suggests that long-term glucose-insulin infusion improves survival in diabetic patients compared to ‘usual care’. He said that in-hospital mortality improves with tight glycaemic control but that “something happens to these patients when they leave hospital as the mortality suddenly shoots up.” It may be because patients become tired of taking so many medications, but he supports the DIGAMI criteria for treatment.
MK has received an honorarium from CV Therapeutics.
