People with peripheral arterial disease (PAD) have a high prevalence of modifiable risk factors for coronary artery disease (CAD). Whether these risk factors are adequately treated remains unknown. We investigated people admitted to hospital with PAD and CAD. We compared use of antiplatelet agents, statins and angiotensin-converting enzyme (ACE) inhibitors before and during admission. Multivariate analysis showed that before admission, compared to patients with CAD, patients with PAD had decreased use of antiplatelet agents (odds ratio [OR] 2.7, 95% confidence interval [CI] 1.2–6.1), statins (OR 3.8, 95% CI 1.5–9.3) and ACE inhibitors (OR = 5.8, 95% CI 2.3–14.3). During admission, treatment was significantly less likely to be initiated in patients with PAD. This shows how secondary prevention can be neglected in patients with PAD. This is an important missed treatment opportunity, with substantial public health implications.
Introduction
Patients with peripheral arterial disease (PAD) have a high prevalence of modifiable risk factors for coronary artery disease (CAD).1 Consequently, they represent a suitable target for secondary prevention and there is strong evidence that this is beneficial.2–4 We aimed to establish whether people with PAD who are admitted to hospital receive equal pharmacological secondary prevention to those with CAD.
Methods
We prospectively recruited patients from 1st March 2003 until 1st June 2003 admitted to a vascular surgery ward (PAD) or cardiology ward (CAD) until discharge. All patients had symptomatic established disease and underwent diagnostic peripheral or coronary angiography. We defined the presence of PAD as: ankle-brachial pressure index < 0.9 or patients who required limb arterial revascularisation, together with typical symptoms.
We defined the presence of CAD as at least one of the following: a history of angina (stable or unstable), percutaneous transluminal coronary angioplasty, angiographic evidence of at least 70% stenosis of a major coronary artery, myocardial infarction (based on World Health Organization criteria) or coronary artery bypass graft surgery.
We interviewed patients on admission to determine prior dyslipidaemia investigation and prescribing of HMG-CoA-reductase inhibitors (statins), angiotensin-converting enzyme (ACE) inhibitors and antiplatelet agents (aspirin, clopidogrel). The primary investigators were not involved in the participants’ care. We reviewed case notes daily to establish which secondary prevention measures were implemented during admission. We recorded whether serum cholesterol was assessed during admission; patients not investigated for dyslipidaemia had venous blood taken on the day of discharge to establish cholesterol levels. We excluded patients with contraindications to treatment and assigned Townsend scores using patients’ postcodes, based on census data. The study was approved by the local research and ethics committee.
Results
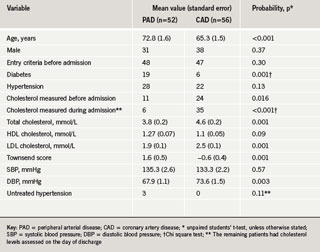
During the study, 52 patients with PAD and 56 patients with CAD met the inclusion criteria. We found patients with PAD were older (72.8 vs. 65.3 years, p<0.001) and there were fewer men (59.6% vs. 67.9%). PAD patients more often had diabetes, and lived in more deprived areas than CAD patients, (p=0.001 and p=0.001, respectively). A similar number of patients in both groups met the entry criteria before admission (48 patients with PAD, 47 patients with CAD, p=0.30). The remaining patients in both groups were diagnosed during admission. Dyslipidaemia was more often investigated in patients with CAD than in those with PAD both before (42.9% vs. 21.1%, p=0.016) and during admission (62.5% vs. 11.5%, p<0.001). Table 1 summarises the baseline characteristics of the study population.
Results are summarised in table 2. Multivariate logistic regression analysis controlling for age, gender, Townsend score and diabetes showed that patients with PAD, when compared with CAD patients, had decreased use of antiplatelet agents (48.1% vs. 71.4%, odds ratio [OR] 2.7, 95% confidence interval [CI]1.2–6.1), statins (32.7% vs. 64.3%, OR 3.8, 95% CI 1.5–9.3) and ACE inhibitors (23.1% vs. 55.4%, OR 5.8, 95% CI 2.3–14.3). Seventeen patients with PAD had coexisting CAD. When excluded from our analyses, the findings were similar: antiplatelet agents OR 3.1 (95% CI 1.1-9.2), statins OR 4.7 (95% CI 1.5–14.3), and ACE inhibitors OR 18.9 (95% CI 3.5–100).
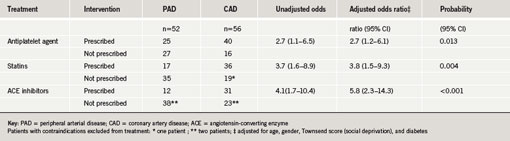
During admission, secondary prevention was more likely to be initiated in patients with CAD: antiplatelet agents OR 16.9 (95% CI 2.4–119.9), p<0.0001; statins OR 18.4 (95% CI 2.6–133.2), p<0.0001; ACE inhibitors OR 9.9 (95% CI 1.3–77.2), p=0.002.
Discussion
Our results show that prior to hospital admission, people with PAD receive markedly less investigation of dyslipidaemia and substantially less treatment with antiplatelet agents, statins and ACE inhibitors than patients with CAD. This represents an important missed opportunity for secondary prevention. In addition, during admission, secondary preventive measures were less likely to be initiated in patients with PAD and dyslipidaemia was less often investigated. When we excluded 17 patients from the PAD group who had coexisting CAD, the likelihood of PAD patients not receiving treatment increased. Multivariate analysis suggests this effect is independent of age, gender, social deprivation (Townsend score) or a history of diabetes. Patients with PAD received less treatment despite the fact that they were more often symptomatic before admission.
It was disappointing that dyslipidaemia was infrequently investigated prior to admission in both groups; however, this is subject to recall bias. Of greater concern was that so few patients with PAD underwent investigation for dyslipidaemia during admission. The reasons for this warrant further investigation. Although investigation of dyslipidaemia during admission in patients with CAD was suboptimal (61.5%), this may be because more patients with CAD had dyslipidaemia investigated before admission.
Our findings are similar to a previous study that identified patients with CAD or PAD from discharge data, who were then telephoned two weeks after discharge and asked to recall advice regarding diet and exercise whilst an in-patient. PAD patients were found to receive less intensive secondary prevention.5 The conclusions from this study are limited by its design (42–46% of patients were lost to follow-up), and the possibility of recall bias.
Subgroup analysis from landmark trials for antiplatelet agents (CAPRIE2), ACE inhibitors (HOPE3) and statins (SSSS4) indicate patients with PAD gain larger relative risk reduction of cardiovascular end points than patients with CAD. Our results suggest these treatment opportunities for patients with PAD are being missed, particularly in secondary care. Future studies should address the public health impact of these findings.
Conflict of interest
None declared.
Key messages
- Patients with peripheral arterial disease (PAD) have a high prevalence of modifiable risk factors for atherosclerosis
- Initiating secondary prevention in patients with PAD significantly reduces death from myocardial infarction and stroke
- When admitted to hospital, patients with PAD are less likely to be taking antiplatelet agents, statins, and angiotensin-converting enzyme (ACE) inhibitors than patients with CAD
- During admission, treatment with antiplatelet agents, statins and ACE inhibitors is less likely to be initiated in patients with PAD than patients with CAD
References
- Mukherjee D, Lingham P, Chetcuti S et al. Missed opportunities to treat atherosclerosis in patients undergoing peripheral vascular interventions: insights from the University of Michigan Peripheral Vascular Disease Quality Improvement Initiative (PVD-QI2). Circulation 2002;106:1909-12.
- CAPRIE steering committee. A randomised, blinded trial of clopidogrel vs aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996;348: 1329-39.
- The Heart Outcomes Prevention Evaluation Study Investigators. Effects of an angiotensin converting enzyme inhibitor, ramipril, on cardiovascular events in high risk patients. N Engl J Med 2000;342:145-53.
- Pedersen TR, Kjekshus J, Pyorala K et al. Effect of simvastatin on ischaemic signs and symptoms in the Scandinavian Simvastatin Survival Study (4S). Am J Cardiol 1998;81:333-5.
- Mc Grae Mc Dermott M, Mehta S, Ahn H, Greenland P. Atherosclerotic risk factors are less intensively treated in patients with peripheral arterial disease than in patients with coronary artery disease. J Gen Intern Med1997;12:209-15.
