Reviewing whether chronic stable angina is a benign condition or whether it requires aggressive management, Professor Robert Wilcox (University Hospital, Nottingham) outlined how the subject of angina is fraught with problems of terms and definitions. What, for example, is ‘stable angina’? Does this relate to the frequency, predictability, duration, severity or the tolerability of the symptoms in an individual? Similarly, when does chronic stable angina become ‘refractory’? A patient who has previously had a myocardial infarction (MI) or an intervention such as a percutaneous coronary intervention (PCI) and now has chronic stable angina, must presumably be different from someone with angina who has not had an intervention, who presents to his general practitioner with exertional chest pain. It is reasonable to suppose that these two individuals will have different prognoses, he said.
Professor Wilcox proposed his own definition: “chronic stable angina is angina occurring at a frequency and severity, acceptable and tolerable to the patient whilst on optimal medical therapy and having made appropriate lifestyle changes, irrespective of prior interventional therapy”. This depends on how much treatment an individual is prepared to take and how many lifestyle changes they are prepared to make.
A recent systematic review and meta-analysis of 74 reports across 31 countries, including more than 400,000 men and women, using the Rose Angina Questionnaire, identified more than 13,000 cases of angina among women and more than 11,000 cases in men (Hemingway H et al. Circulation 2008;117:1526–36). There was considerable heterogeneity in the prevalence of angina but the population-weighted mean for women was just over 6% and for men just under 6%, respectively, so “there’s an awful lot of angina about”, said Professor Wilcox.
The Renfrew-Paisley Study, in the early 1970s, enrolled 15,000 individuals, and found that 2% of the population were Rose Angina Questionnaire-positive (RAQ+ve) and had a resting ECG abnormality (ECG+ve), while another 7% were RAQ+ve but with normal ECGs (ECG-ve). More worrying, however, were the 7% of the population who were RAQ-ve and ECG +ve, representing a “big invisible part of the ischaemia iceberg”. We do not yet have a clear strategy for dealing with these patients, but the 20-year follow-up showed that survival among this group was much worse than among patients with the clinical features of angina but without ischaemic changes, or of course those with neither ischaemia or angina (about 83% of the population), who fare best. Similar gradations are seen for hospital admissions and cardiovascular death.
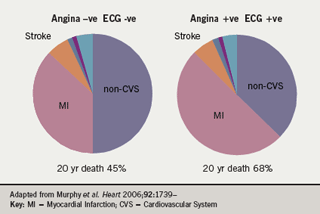
Men without angina or ischaemia had a 45% death rate over 20 years compared to men who had both ischaemia and angina, who had a 68% death rate. The results for women were similar but at slightly lower rates. Over half the deaths were cardiovascular, of which between one and two thirds were due to myocardial infarction (figure 1). There is therefore a gradation of risk within the community according to symptoms and ECG changes. A similar gradation was seen in the British Regional Heart Survey (Lampe RC et al; Eur Heart J 2000;21:1052–63). From the European Heart Survey, Daly and colleagues produced a risk score for prognosis in angina and constructed a risk curve which shows the greatly amplified risk according to the presence of co-morbidities, left ventricular dysfunction and so forth across the spectrum of patients with stable angina (Daly C et al. BMJ 2006;332:262)
The risk of having ischaemia does not abate with time. In the Whitehall Civil Servants study, for example, “the risk of this disease carries on throughout life and has a major impact on life expectancy,” said Professor Wilcox (Clarke R et al. Eur J Cardiovasc Prev Rehabil 2007;14:280–6).
The mass of available evidence suggests that the prevalence of angina is probably about 5% in those aged >40 years; the death rate from that group is about 1 to 3% per annum, depending on co-morbidity and other factors, and the risk of MI is about 2%, but it is highly variable.
What then has been done to improve the outcome in angina? Professor Wilcox looked at some of the older data on coronary artery bypass surgery (CABG) versus medical treatment, including a meta-analysis of seven trials but enrolling only 2,649 patients (Yusuf S et al. Lancet 1994;344:563). The data showed an advantage for surgery with a “deferring of death” of about two years, but the survival curves converge at around 12 years, as “no treatment will impart immortality”. He reminded the audience that both the surgery and the drugs deployed were rather “old fashioned” and rudimentary compared to what is currently available; however, these are the only data we have comparing the two treatments of angina.
The situation for PCI is probably less good than for surgery. Whereas PCI is extremely good at reducing angina symptoms, “it does not reduce the incidence of death or non-fatal MI” and the likelihood of a repeat procedure is much greater compared to CABG. Some of the best information on PCI comes from the Second Randomised Intervention Treatment of Angina Trial (RITA-2), which evaluated the long-term effects of PCI versus medical management as initial treatment strategies in angina patients with angiographically proven coronary artery disease (CAD). Current symptoms were not mandatory and patients with multivessel disease and ventricular impairment were included. (Patients with significant left main stem disease or previous revascularisation were excluded.) Seven-year follow up data from the trial showed “no difference whatsoever” in overall death between medical treatment and PCI (Henderson R et al. J Am Coll Cardiol 2003;42:1161).
In contrast, medical treatment was associated with lower rates of death/MI, due mainly to the early risk of intervention, and 60% or more of medically treated patients “were saved an intervention by continuing medical therapy”. The RITA-2 authors therefore concluded that, as an initial strategy, intervention will not significantly influence outcomes but it will improve angina symptoms and exercise tolerance. Also, patients considered equally suitable for intervention or medical therapy can be safely managed with continued medical therapy, but PCI is appropriate if symptoms are not controlled.
The trial was criticised by US workers, who are regarded as more prone to intervention bias, but this criticism has in turn been challenged by findings from the COURAGE trial (Boden WE et al. N Engl J Med 2007;356:1503–16). This landmark study investigated whether PCI plus optimal medical therapy result in superior outcomes when compared with optimal medical therapy alone. Conducted in 2,287 stable angina patients, the trial was arguably over-represented by white males (86%), but they were high-risk patients: one third had diabetes, two thirds hypertension and nearly 40% had a previous MI. The medical therapy was “really quite intensive”, comprising antiplatelet agents, long-acting metoprolol, amlodipine, isosorbide mononitrate, lisinopril or losartan, simvastatin +/- ezetimibe (target low-density lipoprotein cholesterol [LDL-C] < 2 mmol/L), exercise, niacin and fibrate (target high-density lipoprotein cholesterol [HDL-C] >1.03 mmol/L and triglycerides [TG] <1.69 mmol/L).
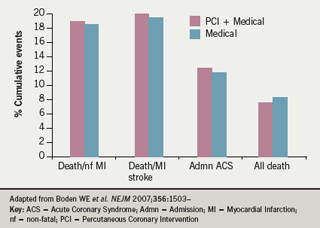
After a mean of 4.6 years, “no difference whatsoever” was found between the two treatment arms in the rates of death or non-fatal MI, stroke, admission for acute coronary syndrome or all-cause mortality (figure 2). COURAGE was criticised for being unrepresentative, for not including high enough risk patients and because one third or more of the medical group went on to have an intervention. This was good news“as that means two thirds didn’t need it!”, said Professor Wilcox. About 20% of patients who had PCI needed a repeat procedure. Such findings are important and they “should influence our attitude to dealing with patients with chronic stable angina,” in his view.
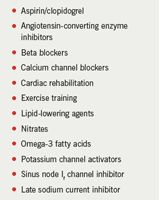
There are many non-interventional strategies for stable angina (Table 1): not all of which have been shown to improve survival and supportive data for many of these agents are limited in the stable angina setting. “There is a lot now medically that can be offered to patients which was not available in the past, and certainly was not available when the early trials of medicine versus surgery were conducted,” said Professor Wilcox.
In summary, chronic stable angina is not a benign condition in Professor Wilcox’s view. He said that “chronic stable angina has variable risk depending on co-morbidity, gender and prior cardiovascular events….Modern aggressive medical therapy performs well against PCI, but has not been compared with CABG. And, as newer anti-anginal drugs become available, their place in risk reduction rather than just symptom control will need to be assessed. Because we are adding on treatments, we are looking for small incremental benefits of these new drugs.”
The best approach to screening for and dealing with silent ischaemia is not established. Once ischaemia is proven as the likely cause of chest pain, should an angiogram be performed to look for “interventionally-preferred treatment?” This is one of the dilemmas in managing patients who present with new-onset angina. Alternatively, we might say to the patient that we can safely treat him medically, Professor Wilcox concluded.
RW acknowledges research income from CV Therapeutics Europe Ltd to the University of Nottingham.
