Heart failure (HF) is an important cause of morbidity and mortality in the general hospital setting worldwide. The paucity of data on psychiatric co-morbidity in Nigeria necessitated this study. This study was carried out among adults in stable state of HF at the cardiology clinic of Lagos University Teaching Hospital (LUTH) with sex- and age-matched controls.
Fifty-eight subjects were studied, made up of 27 (46.6%) males and 31 (53.4%) females. The mean age was 51.2±13.8 years. There were 44 age- and sex-matched controls with mean age of 50.1±13.6 years. Thirty-four of the subjects (58.6%) had General Health Questionnaire (GHQ) scores of ≥2 (cut-off score); out of which 14 (24.4%) were confirmed to have psychiatric disorders. One subject with GHQ score <2 also had a psychiatric diagnosis giving a sensitivity of 0.93 and specificity of 0.54 for GHQ-12 in this study. Thus, a total of 15 (25.9%) had psychiatric diagnoses which included: depression 7 (12.0%); generalised anxiety 6 (10.3%); paranoid schizophrenia 1 (1.7%), and somatisation disorder 1 (1.7%).
It is concluded that clinically significant psychiatric co-morbidities exist among subjects with HF. The need for ‘liaison’ psychiatric services in the cardiology clinic is emphasised.
Introduction
A large number of studies have documented a high rate of co-occurrence of psychiatric morbidity and chronic medical conditions, such as bronchial asthma, diabetes, hypertension and heart disease.1,2Specifically, in heart failure (HF), psychiatric complications such as depression and anxiety are very common.3,4 In Africa, most especially Nigeria, HF is quite common with attendant high morbidity and mortality rates.5,6 Studies have shown that co-morbid psychiatric disorders delay recovery from HF, increasing length of hospital stay, with associated poorer prognosis and increased mortality.7,8 Despite the importance of co-morbid psychiatric complications and HF, the paucity of studies in the country (Nigeria) necessitated this work.
Materials and methods
Study setting
The study was carried out at the cardiology clinic of Lagos University Teaching Hospital (LUTH), Idi-Araba, Lagos, the commercial capital of Nigeria. The clinic takes place on Tuesday with average patients’ patronage of 70 per clinic session (both new and follow-up cases), most especially patients with hypertension and/or HF.
Subjects
Subjects aged 18 years and above, in stable state of HF and on clinic follow-up were studied over a six-month period. HF was defined by a left ventricular ejection fraction of <40% with or without accompanying clinical symptoms.9 Necessary explanation was given on the study and consent obtained from the subjects in addition to the permission granted by the research and ethical committee of the hospital to carry out the study. Out of 62 patients who met the eligibility criteria and gave verbal consent to be included in the study, 58 (93.5%) eventually took part in the study.
Instruments
General Health Questionnaire (GHQ)
GHQ was developed by Goldberg (1972) as a screening instrument aimed at detecting psychiatric disorders in the community, in primary and post primary care settings.10 The GHQ-12 with preserved psychometric properties of the original 60-item version was used in this study, and the cut-off score set at 2; the optimum cut-off score from previous studies.11
International Classification of Diseases–10th Edition (ICD–10)12
The diagnostic description and clinical guidelines of the ICD-10 was used to make definitive diagnoses from clinical interviews conducted by one of the authors, a consultant psychiatrist.
Rating scales
The following rating scales were used to assess the severity of psychopathologies diagnosed on the subjects:
- Brief Psychiatric Rating Scale (BPRS) was developed by Overall and Gorham (1962),13 designed as an outcome measure in treatment studies of schizophrenia and also used to rate patients with very severe impairment from psychotic symptoms.
- Hamilton Depressive Rating Scale (HDRS) was designed by Hamilton (1960)14 to assess severity of depression and to track changes in depressive symptoms over time in treatment.
- Hamilton Anxiety Scale (HAM-A) is a rating scale developed by Hamilton (1959)15 to quantify the severity of anxiety symptomatology.
Procedure
Each of the subjects and controls was given a socio-demographic questionnaire and the GHQ-12 to complete by a research assistant (a senior registrar in cardiology). The completed questionnaires were made blind to the consultant psychiatrist (OFA) who thereafter carried out a comprehensive clinical interview and mental state examination on each of the subjects. For each of those with presence of psychiatric symptoms, the appropriate Axis-I diagnosis was made in line with the diagnostic description and clinical guidelines of ICD–10.12
The severity of the diagnosed psychiatric illness was rated with the appropriate rating scales.
Statistical analysis
This was performed on SPSS® for Windows® version 10.0. Frequencies and percentages were calculated for discrete categorical variables and means with standard deviation for the continuous variables. Correlation analysis was also carried out between the subjects’ socio-demographic variables and scores obtained on the psychometric instruments. The data obtained from the subjects and controls were compared using chi-squared test with statistical significance set at 0.05.
Results
Socio-demographic characteristics
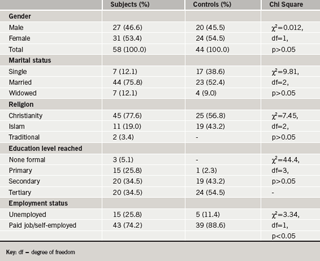
A total of 58 subjects in stable state of HF were studied (table 1); made up of 27 (46.6%) males and 31 (53.4%) females. The mean age was 51.2±13.8 years with a range of 18–83 years. The majority, 44 (75.9%), were married, seven (12.1%) widowed and six (10.3%) single. Three (5.2%) had no formal education, 15 (25.9%) had only primary school education, 20 (34.5%) had secondary school certificate, and 20 (34.5%) had received tertiary education. In terms of employment, 15 (25.8%) were not actively engaged in any job (students, unemployed and retirees). The rest, 43 (74.2%), were in paid employment or self-employment.
There were 44 apparently healthy controls matched for age and sex, made up of 20 (45.5%) males and 24 (54.5%) females. The mean age was 50.1±13.6 years with a range of 15–76 years. Significant statistical differences between subjects and controls was only apparent in employment status with χ2=3.34, degree of freedom (df) =1 at p≤0.05.
Causes and severity of HF
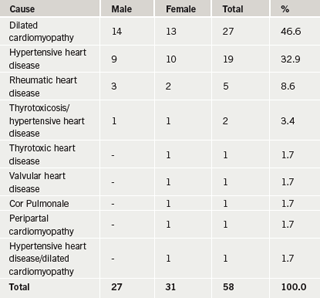
In nearly half (46.6%) of the patients HF was caused by dilated cardiomyopathy, followed by hypertensive heart disease (32.9%) and rheumatic heart disease (8.6%). Other causes are shown in table 2.
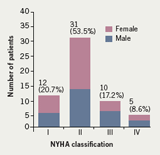
The severity of HF using the New York Heart Association (NYHA) classification shows over half (53.5%) of the subjects had class II level of severity, followed by class I (20.7%), class III (17.2%) and lastly class IV (8.6%) (figure 1).
Psychiatric morbidities
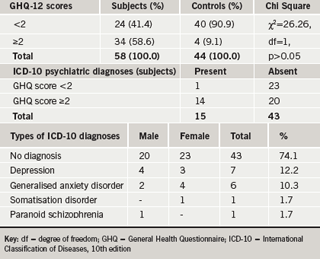
Thirty-four (58.6%) of the 58 subjects had a GHQ score ≥2 (the cut-off score); while four (9.1%) of the 44 controls had GHQ scores ≥2. The difference was not statistically significant (χ2=26.26, df=1 and p>0.05).
Out of the 34 subjects with GHQ scores ≥2, 14 were confirmed (from the psychiatric interview and diagnosis with ICD-10) to have a form of psychiatric illness. Among the 24 subjects with GHQ score <2, only one was found to have psychiatric illness during further evaluation. This gives a sensitivity of 0.93 and specificity of 0.54 for the instrument (GHQ–12) in this study. Thus, overall, 15 (25.9%) out of the total 58 subjects had psychiatric illness (from both GHQ screening and ICD–10 diagnostic evaluation). The diagnoses included: depression 7 (12.2%) with mean HDRS score of 25.8; generalised anxiety disorder (GAD) 6 (10.3%) with mean ham-a score of 17.2; somatisation disorder 1 (1.7%); and paranoid schizophrenia 1 (1.7%) with BPRS score of 22 (table 3). No psychopathology was detected among the other 43 (74.1%) patients.
No significant correlation was found between GHQ scores and the socio-demographic variables of sex, marital status, education and occupation.
Discussion
The 25.9% prevalence of psychiatric morbidity in our study of subjects in stable state of HF is clinically significant. This figure is only slightly higher than that of Wells et al. (1998)1 who found 24.7% of their subjects with chronic medical conditions had psychiatric complications. Our figure also fell within the range of 25–30% obtained by Barrett et al. (1988) and Derogatis et al. (1989).16,17 When compared with local Nigerian studies, our figure is similar to that of psychiatric morbidity (15–25%) among attendees of general hospital settings with chronic medical illness,18 and even closer to the figure (27.8%) obtained by Gureje et al. (1992).19
As a popular screening instrument, the cut-off score of 2 for the GHQ-12 used in this study is in line with Goldberg’s (1972) original validity study in the UK;10,20 and also previous studies in Nigeria.21The specificity and sensitivity figures obtained in this study for the GHQ are similar to previous Nigerian studies;21,22 although the sensitivity figure in our study seemed to be moderately higher.
In our study, depression and GAD were the most common psychiatric co-morbidities among our subjects. This is in line with findings from previous studies.1,2 In Nigeria, studies have shown a high level of hesitancy to consult psychiatrists in chronically ill patients with mental health complications;23,24 hence, to ensure adequate care it is recommended that a ‘modified’ or ‘mini’ liaison psychiatric practice is set up in conjunction with cardiologists and even other medical specialists in the country. This would involve a psychiatrist visiting the cardiology clinic and cases requiring psychiatric evaluation could then be seen in the clinic by the psychiatrist. The arrangement would be such as to guarantee follow-up treatment of the psychiatric complication alongside that of the cardiac pathology. This integrative form of practice (though not labelled as recommended above) is already conducted in some centres in Europe and North America to overcome the stigma associated with psychiatric referrals.2
In conclusion, significant levels of psychiatric complications have been demonstrated among patients with chronic HF in Nigeria; and the need for special consultation-liaison psychiatry in cardiology clinics is emphasised. However, the small number of subjects is a limitation of this study. Further studies in a larger number of patients with chronic HF are required in other centres in Nigeria in order to generalise these findings in the population.
Conflict of interest
None declared.
Key messages
- Heart failure is an important cause of morbidity and mortality
- Co-morbid psychiatric conditions can delay recovery resulting in a poorer prognosis and increased mortality
- Psychiatric co-morbidity was found in a quarter of heart failure patients attending a cardiology clinic in Nigeria
- A cut-off point of ≥2 on the General Health Questionnaire was sensitive for the detection of psychiatric illness
- Liaison psychiatric services should be available in cardiology clinics to encourage appropriate recognition and management of psychiatric conditions
References
- Wells KB, Golding JM, Burnam MA. psychiatric disorders in a sample of the general population with and without chronic medical conditions. Am J Psych 1988;145:976–81.
- Maruish ME. Prevalence of behavioural health disorders. In: Handbook of psychological assessment in primary care settings. Mahwa, New Jersey: Lawrence Erlbaum Associates Publishers, 2000: pp 6–8.
- Mayou RA, Gill D, Thompson DR et al. Depression and anxiety as predictors of outcome after myocardial infarction. Psychosom Med 2000;62:212–19.
- Balestroni GL. Psychological intervention and heart failure: from theory to clinical practice. Monaldi Arch Chest Dis 2002;58:166–73.
- Akinkugbe OO, Nicholson GD, Cruickshank JK. Heart disease in black of Africa and the Caribbean. Cardiovasc Clin 1991;21:377–91.
- Sliwa K, Damasceno A, Mayosi BM. Epidemiology and etiology of cardiomyopathy in Africa. Circulation 2005;112:3577–83.
- Vaccarino V, Kasl SV, Abraahson J, Krumholz HM. Depressive symptoms and risk of functional decline and death in patients with heart failure. J Am Coll Cardiol 2001;38:199–205.
- MacMahon KM, Lip GY. Psychological factors in heart failure; a review of the literature. Arch Intern Med 2002;162:509–16.
- Task Force for the Diagnosis and Treatment of Heart Failure. Eur Heart J 2001;22:1527–60.
- Goldberg D. The detection of psychiatric illness by questionnaire: A technique for the identification of non-psychotic psychiatric illness. London: Oxford University Press, 1972.
- Goldberg DP, Gater R, Sartorius N et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med 1997;27:191–7.
- World Health Organization. International Classification of Diseases and related health problems. 10th edition. Geneva: WHO, 1992.
- Overall JE, Gorham DR. The Brief psychiatric Rating Scale. Psychol Rep 1962;10:799–812.
- Hamilton M. A rating scale for depression. J Neurol Neurosurg psych 1960;23:56–62.
- Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol 1959;32:50–5.
- Barrett JE, Barratt JA, Oxman TE, Gerber PD. The prevalence of psychiatric disorders in primary care practice. Arch Gen Psychiatry 1998;45: 1100-06.
- Derogatis LR, Wise TN. Anxiety and depressive disorders in the medical patient. Washington DC: American Psychiatric Press, 1989.
- Udofia O, Oseikhuemen AE. psychiatric morbidity in patients with sickle cell anaemia. West Afr J Med 1996;15:196–200.
- Gureje O, Obikoya B, Ikuesan BA. Prevalence of specific psychiatric disorders in an urban primary care setting. East Afr J Med 1992;69:282–7.
- Lewis G, Araya RI. Is the General Health Questionnaire (12-item) a culturally biased measure of psychiatric disorder? Soc psychiatry Psychiatr Epidemiol 1995;30:20–5.
- Gureje O, Obikoya B. The GHQ–12 as a screening tool in primary care setting. Soc Psychiatry Psychiatr Epidemiol 1990;5:276–80.
- Morakinyo O. The sensitivity and validity of Cornell Medical Index and the General Health Questionnaire in an African Population. Afr J psychiatry 1979;2:1–8.
- Adeyemi JD, Ohaeri JU, Olatawura MO, Odejide AO, Famuyiwa OO. Who wants to see a psychiatrist? Proceedings of the 9th Pan-African psychiatric Conference, Lagos, Nigeria, November 20–26, 1994:145–58.
- Aina OF, Adeyemi JD. An overview of consultation-liaison psychiatry and current trend in West African sub-region. Nig Qt J Hosp Med 2005;15(4):168–71.
