A busy three-day programme comprised this year’s meeting at the ExCel Centre, London, from 1st–3rd June 2009. We report on a few of the meeting’s highlights.
Report shows access to cardiac care is patchy in the UK
A new UK-wide study, mapping disparities in access to cardiac care, has “major implications for provision of services throughout the UK” says Professor Keith Fox (University of Edinburgh) President, British Cardiovascular Society (BCS).
The report, commissioned by the BCS, the British Heart Foundation and the Cardio & Vascular Coalition, shows that despite finding a marked increase in provision of the main cardiac treatments in the country, there were many parts of the UK where access was significantly below the levels expected. It also shows the UK being in the lower quartile for the main cardiac interventions, with the exception of total cardiac resynchronisation therapy (CRT) when compared to other similar developed countries.
The study analysed population access, variations and inequalities in England, Northern Ireland, Scotland and Wales from 2000 to 2006. “It is the first time we have had such comprehensive data in the UK,” said Dr David Hackett, current Vice-President of the BCS. The study is the first to systematically explore the seven main cardiovascular procedures using a consistent set of assumptions across all four nations of the UK.
The future projections model the numbers of interventions that will be required in order to match provision to estimated need and reduce variations in access. By 2020, there will need to be a significant increase in the numbers of cardiac procedures provided across the UK. Some parts of the country will also need to plan for higher increases than others because of their local population characteristics, and because some of their current intervention rates are lower than expected.
The cardiac interventions in need of the most focus are electrophysiology and arrhythmia intervention. Areas with a high population of elderly patients are particularly under-resourced, with areas such as Wales and the West Midlands needing a growth of 201% and 224%, respectively, in new pacemakers. “We are still lagging behind other countries in Europe for pacemaker implants” said Dr Hackett.
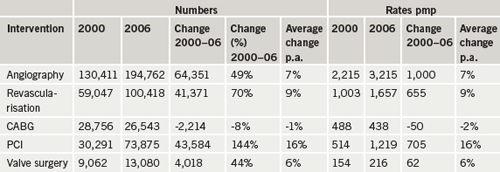
The good news, however, is that, “the outlook for people with heart conditions is better than ever before in all parts of the UK. In the six years from 2000 to 2006, patients in every region have benefitted from significantly improved access to the main critical cardiac care interventions,” Professor Fox concluded (see table 1).
Allopurinol prolongs exercise time in stable angina
Results from a study presented at the meeting by Dr A Norman, (University of Dundee) support the use of allopurinol as a novel anti-ischaemic agent in patients with angina pectoris.
Experimental work has shown that allopurinol, a xanthine oxidase inhibitor used for treatment of gout, improves “mechano-energetic uncoupling” of the myocardium in heart failure, he said. This means that allopurinol reduces myocardial oxygen demand for a given stroke volume, an effect which might be of value in angina pectoris. In addition, allopurinol has been shown to improve endothelial function and reduce oxidative stress in patients with coronary artery disease.
In a double-blind, placebo-controlled, crossover trial, 60 eligible patients with chronic stable angina and angiographically confirmed coronary artery disease were randomly assigned to receive either placebo or allopurinol (600 mg/day) for six weeks and were then crossed over to the alternative therapy for a further six weeks. The main outcome measurements were changes in total exercise time (TET), time to onset of angina symptoms (Tsym) and time to ST depression (TST) on the exercise treadmill test using the Bruce protocol. These measures were assessed at baseline and after each treatment period.
The median baseline TET was 301 s, Tsym was 233.5 s and TST was 232 s. Allopurinol increased TET by 53.7 s versus -7.1 s for placebo (p<0.001), Tsym by 49.5 s versus 9.5 s for placebo (p = 0.01) and TST by 48.5 s versus 14.5 s for placebo (p<0.001).
In patients with chronic stable angina, allopurinol (600 mg/day) improves TET and Tysm and to ischaemia during exercise. The results also point towards a potential role for the enzyme xanthine oxidoreductase in the pathophysiology of angina.
Serial haemoglobins predict long-term CV outcomes
Both the presence of anaemia at baseline and at follow-up independently predict long-term adverse clinical outcomes in patients after an acute coronary syndrome (ACS), according to Dr DSC Ang, and colleagues (University of Dundee).
Baseline anaemia in patients with acute coronary syndrome is an independent predictor of adverse clinical outcomes. However, little is known about serial haemoglobin measures after an ACS event and its impact on prognosis in this patient population. Haemoglobin levels were measured in 448 consecutive patients presenting with ACS and at seven weeks outpatient follow-up. The main outcome measure was either the occurrence of death or acute myocardial infarction (AMI) over a median duration of 2.5 years (range 1-50 months).
Of the 448 patients, 120 patients presented with ST elevation myocardial infarction (27%). During follow-up there were 117 deaths or cases of AMI. The prevalence of anaemia on admission was 20% and this figure increased to 50% at seven weeks’ follow-up. Adjusting for a variety of baseline, clinical, laboratory and echocardiographic variables (e.g. left ventricular systolic dysfunction), the presence of anaemia was strongly associated with subsequent deaths or AMI when measured on admission and also at seven weeks post-ACS. Patients with persistent anaemia at seven weeks were at an increased risk of death or AMI compared with those with persistently normal haemoglobin.
The study also showed that, in ACS, the prevalence of anaemia increases substantially at seven weeks follow-up (40%) when compared with admission haemoglobin levels; and that both the presence of anaemia at baseline and at follow-up independently predicts long-term adverse clinical outcomes.
Study findings also suggest that the trend of haemoglobin post-ACS is a more important predictor of adverse prognosis compared with a one-off low haemoglobin level at baseline.
What’s new with fish oils?
An interesting symposium sponsored by Solvay Healthcare on omega-3 fatty acids (fish oils) chaired by chaired by Professor Julian Halcox (University of Wales) discussed the relevance of omega-3 biology in cardiovascular disease (CVD) and whether fish oil preparations have a role in preventing sudden cardiac death.
Earliest interest came from observations among the Inuit population of Greenland who despite consuming a diet high in fat suffer low rates of CVD. Meta-analyses suggest that a high intake of fish actually reduces the relative risk of cardiac mortality. This appears to be related to high levels of essential omega-3 fatty acids. It is known that these fatty acids may have a number of effects, including anti-arrhythmic, and anti-inflammatory effects, as well as triglyceride reduction and reductions in platelet aggregation.
Dr Adrian Brady (Glasgow Royal Infirmary) turned attention to how best to treat patients with left ventricular dysfunction (LVD), which is observed commonly in coronary artery disease and post-MI patients. Patients with LVD are at increased risk of death and many trials over the past 30-40 years have shown that adding therapies can reduce mortality. But what should best practice look like? We know that standard therapy includes aspirin, beta blockers and ACE inhibitors but what about the benefits of angiotensin II receptor blockers, clopidogrel and omega-3s, he asked? They all seem to have a part to play in modern management of LVD and recent findings from the GISSI-HF study suggest that a 1 g fish oil preparation daily on standard background medical therapy is safe and effective in reducing all-cause mortality and CV hospital admissions in chronic heart failure patients.
Dr Henry Purcell (Royal Brompton Hospital, London) looked into the putative anti-arrhythmic effects of omega-3s referring back to the Italian GISSI-Prevenzione trial published in 1999. This 11,000 patient study suggested that fish oils may reduce sudden cardiac death early after a myocardial infarction (MI). Even in a population of high ‘fish-eaters’ in Japan, the JELIS study also showed a reduction in major coronary events with high dose eicosapentanoic acid (EPA). These positive data for omega-3s in CVD have led to their inclusion in a number of guidelines including National Institute for Health and Clinical Excellence, Joint British Societies (JBS2), European Society of Cardiology, American Heart Association and the Scottish Medicines Consortium.
More recent data from patients with implantable cardioverter defibrillators (ICDs) did not support a protective effect of omega-3s on cardiac arrhythmia, and that benefits may be dependent on the nature of the underlying disease substrate. Fish oils may be more protective, for example, in patients with a recent MI or acute myocardial ischaemia based on triggered activity and prolonged action potentials rather than on life-threatening re-entrant arrhythmias
Alison Mead (a specialist dietitian from Imperial College London) looked at just how easy is it to get the recommended amount of omega-3s from diet alone. Education, however, is the key for the patient to know where, how much and how often they need to eat certain foods. And, of course, the real question is will they actually consume any fish at all? Early identification and education of patients in coronary care will give us as healthcare providers the advantage we need to help our patients. If they can’t be persuaded to eat enough oily fish then using a licensed omega-3 ethyl ester is another option.
