Colin Doig and Henry Purcell report highlights from the recent Cardiology at the Limits meeting held in Cape Town, South Africa
One of today’s great dilemmas is how we adequately deliver highly developed healthcare to still developing nations. Ironically, about 80% of cardiovascular diseases are now occurring in developing countries. Africa is a case in point. In the South African townships of Soweto, for example, 87% of the population have one or more coronary heart disease (CHD) risk factors. Populations already wracked by HIV/AIDS, which has a prevalence of about 11% in South Africa, now have to cope with emerging epidemics of coronary and other heart-related disorders such as HIV-associated cardiomyopathy, tuberculous pericarditis and the cardiac complications of antiretroviral therapy. There are an estimated three million people (some 30% of the amount required) receiving antiretrovirals.
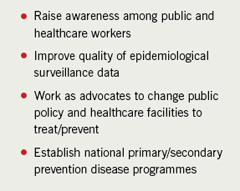
Even more pertinent are the ‘forgotten cardiac diseases’ of Africa. These include rheumatic heart disease (RHD), which remains a major cause of morbidity and premature death, with surveys showing current prevalence rates of approximately one to five cases per 1,000 among school-aged children in developing countries, with the highest rates in sub-Saharan Africa. The Pan African Society of Cardiology (PASCAR) believes that Africa has 10% of the world population, but as many as half of the 2.4 million children affected by RHD globally. Mindful of the fact that the major determinants of rheumatic fever (RF) and RHD are poverty, overcrowding, poor housing and shortage of healthcare resources, PASCAR convened the First All-Africa workshop on RF and RHD in October 2005 producing the Drakensberg Declaration,1 which called on African governments and the world community to accelerate investment and initiatives designed to eradicate these problems permanently. They identified four particular areas of activity to achieve this (table 1).
A further ‘forgotten disease’ is endomyocardial fibrosis. A tropical disease, it is the most common cause of restrictive cardiomyopathy, resulting in impaired filling of one or both ventricles, and right or left heart failure (or both), which is estimated to affect 10 million people worldwide. In its severest form it carries a two-year prognosis after diagnosis and it is highly prevalent in parts of Africa, notably, Mozambique, Uganda and Nigeria, as well as other countries, such as south India and Brazil.
While both conditions can be detected clinically, cardiac ultrasonography is much more sensitive than auscultation at picking up pathological valve disease. The World Health Organization (WHO) recommends that clinically silent rheumatic valve involvement should be managed as RHD until proved otherwise.
Early detection
The potential for using small hand-held, battery-operated systems for the early detection of these diseases in their asymptomatic stages is both exciting and immense, and this was the basis of a presentation by Dr Ana Mocumbi a cardiologist with a particular interest in paediatric cardiology, which is a consistent major theme of the Cardiology at the Limits Scientific Meetings Programme. Based in the Heart Institute, in Maputo, Mozambique, she has spearheaded national programmes for the control of major endemic diseases. Dr Mocumbi has collaborated scientifically with major cardiology centres including the Heart Science Centre at Harefield Hospital, UK.
She presented details of two major projects on endomyocardial fibrosis2 and RHD,3 both of which were published in the New England Journal of Medicine. The first study,2 involved systematic sampling of a rural community in Mozambique, with detailed transthoracic echocardiography in 211 of 1,000 randomly selected subjects. The overall prevalence of endomyocardial fibrosis was 19.8%, being highest in males and in the 10 to 19 years age range. Most affected subjects had mild-to-moderate structural and functional echo abnormalities, but only 48 (22.7%) were symptomatic. The large population affected offers unique opportunities for studying the basic molecular mechanisms of the disease, which may be due to genetic (there was a familial occurrence) or environmental factors, or both, and for developing treatment and prevention strategies. Currently, there is no effective treatment. It may also help in understanding other forms of cardiomyopathy and diseases involving fibrosis.
The second study,3 conducted in both Mozambique and Cambodia, involved almost 6,000 children and identified 145 cases of echo-confirmed RHD, corresponding to prevalence rates of 21.5 and 30.4 cases per 1,000, respectively; rates 10-times greater with echocardiographic screening compared with traditional clinical screening. Ninety per cent of cases in this study were clinically silent, occurring in asymptomatic children without audible murmurs.
The findings may encourage a drive to make more funding available for RHD screening programmes, and have potentially important implications for case finding and prevention of this devastating disease in developing nations.
Atrial fibrillation – another epidemic
Echocardiography is, of course, also invaluable in investigating the ‘spectrum of conditions’ we have come to know in atrial fibrillation (AF). This was described by another speaker, Professor Jonathan Kalman, Director of Electrophysiology at the Royal Melbourne Hospital, Australia.
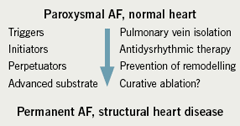
For many years, the prevailing understanding of the genesis and maintenance of AF has been the re-entrant wavelet hypothesis. In this model, waves are constantly abutting regions of refractoriness resulting in persistently shifting patterns of ineffectual stimulation. Haissaguerre challenged this concept in 1998 when he described the single focus concept with myocardial sleeves of tissue extending onto the pulmonary veins. This raised a new target for ablative therapy and much of the advance of this technology in the last decade has come from this insight. Professor Kalman reminded the audience that it was perhaps more constructive for cardiologists to break down the process of AF into component parts, all of which have a role in the genesis or maintenance of AF (figure 1). These comprised triggers (pulmonary vein ectopics), initiators (anatomical and functional obstacles) and perpetrators (persistent triggers, remodelling). In an individual patient, each of these may be more or less important, making them attractive for medical attention in a patient-specific tailored fashion.
However AF begins, the maxim that AF begets AF holds true for most patients because of recent understandings in the mechanism of preservation of the dysrhythmia. AF promotes atrial cellular calcium loading, which threatens cell viability. This results in the down-regulation of calcium channels. This alters action potential duration and increases the disparity of refractoriness within atrial tissue, hence maintaining AF. In chronic AF, the interstitial fibrosis and glycogen accumulation in cells further enhance this disrupted architecture and functionality (anisotropy). Further insight into the possible aetiology of AF has come from Italian studies, which have shown that 66% of atrial septal biopsy samples from AF patients have evidence of previous atrial myocarditis.
Treatment
With regards to disease specific treatment, angiotensin-converting enzyme (ACE) inhibitors have been shown in meta-analyses of heart failure studies to be associated with a marked reduction of AF occurrence. More work is needed as there is a mixed story in the use of these agents in hypertension and for treatment of AF alone. Another angle for medical intervention might come from the respiratory world where AF is associated with obstructive sleep apnoea, and continuous positive airway pressure (CPAP) after DC cardioversion is helpful in maintaining sinus rhythm.
Given that Cardiology at the Limits invites its speakers to take the audience to the limit of known understanding, Professor Kalman described the current position of electrophysiology and radiofrequency ablation in the management of AF. In paroxysmal AF, the aim is to circumferentially isolate the pulmonary veins in a double lasso procedure. Studies, predominately in a younger population, have shown greater benefit of ablation over traditional antidysrhythmic medical therapy. Since the long-term prognosis for lone AF is good, ablative therapy is used in symptomatic patients with a complication rate of 4%. Cryo-ablative balloon intervention may offer additional advantages over current procedures.
Persistent AF is a harder nut to crack. Where intervention is needed, multiple procedures are often required. The precise target or technique for intervention has not been agreed. There are no agreed definitions or standards by which the success of ablative procedures can be defined. Like the Maze surgical procedure, outside observers may deem ablation for persistent AF to have inherently failed, as most patients remain on long-term anticoagulation. Thus, it could be argued, for now, we are at the limits of our interventional treatment for AF. If so, Professor Kalman suggested we return to the basic paradigm and treat aggressively those areas where we know intervention or lifestyle changes can have a positive impact.
Acknowledgements
Cardiology at the Limits is organised by Professor Derek Yellon and Professor Lionel Opie as part of a joint initiative between the Hatter Institutes of University College London and the University of Cape Town. The annual meeting has been created to establish greater collaboration and development between the two institutions, both of which have international reputations in the field of cardiovascular research. This year’s meeting was supported by an unrestricted educational grant from Pfizer. The authors were sponsored delegates at the meeting.
References
- Mayosi B, Robertson K, Volmink J et al. The Drakensberg declaration on the control of rheumatic fever and rheumatic heart disease in Africa. S Afr Med J 2006;96:246.
- Mocumbi AO, Ferreira MB, Sidi D, Yacoub MH. A population study of endomyocardial fibrosis in a rural area of Mozambique. New Engl J Med 2008;359:43–9.
- Marijon E, Ou P, Celermajer DS et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N Engl J Med 2007;357:470–6.
Colin Doig
Consultant Cardiologist
Northumbria Healthcare NHS Foundation Trust
Henry Purcell
Senior Fellow in Cardiology
Royal Brompton Hospital, London
