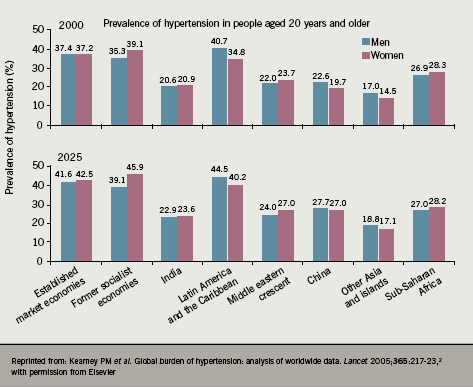
High blood pressure (BP) is one of the leading health risk factors for global mortality, being a higher risk factor than tobacco use, high cholesterol and under-nutrition in both developed and developing regions.1 The estimated total number of adults around the world with hypertension in the year 2000 was 972 million but this figure is predicted to rise by approximately 60% by 2025 to a total of 1.56 billion, due to an ageing population2 and the adverse impact of several aspects of development (figure 1).
Impact of hypertension
Epidemiological data have established a strong direct relationship between increased BP and raised cardiovascular (CV) disease risk. For individuals aged 40–69 years, each increment in systolic BP of 20 mmHg or diastolic BP of 10 mmHg doubles the risk of CV disease (i.e. stroke, ischaemic heart disease, and other vascular diseases) across the entire BP range.3
The World Health Organization has identified high BP as one of the most important preventable causes of premature morbidity and mortality. Antihypertensive drugs have convincingly been shown to be effective treatments for reducing this CV risk. By the mid-1990s an overview of 17 completed randomised trials of antihypertensive treatment by MacMahon et al. demonstrated that a 5–6 mmHg reduction in diastolic BP reduced stroke risk by 38% and coronary heart disease (CHD) risk by 16%.4 There are also other benefits conferred to a variable extent by different antihypertensive therapies, including regression of left ventricular hypertrophy, prevention of dementia, regression of vascular remodelling and atherosclerosis, as well as prevention or delay of the onset of diabetes.
The treatment of hypertension
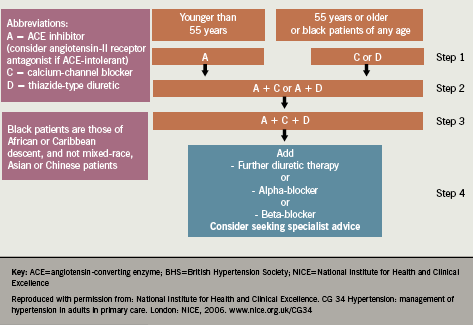
Management of hypertension in the UK has improved greatly in the last decade due to increased awareness of the significant health risks associated with the condition, improved hypertension management offered by primary care practitioners, and the availability of effective treatment options. Furthermore, the British Hypertension Society (BHS)5 and National Institute for Health and Clinical Excellence (NICE)/ BHS guidelines6 have become widely and increasingly adopted by healthcare professionals. These guidelines provide a clear simple treatment algorithm for patients diagnosed with hypertension. For hypertensive patients aged 55 years and over, or black patients of any age, the initial therapy should be either a calcium channel blocker (CCB) or a diuretic (thiazide or thiazide-type diuretic e.g. indapamide or chlorthalidone). In hypertensive patients younger than 55 years, first-choice therapy should be an angiotensin-converting enzyme inhibitor (ACE inhibitor) or an angiotensin receptor blocker (ARB) if an ACE inhibitor is not tolerated (figure 2).
However, CV events are most effectively prevented not by simply reducing high BP in isolation but by improving more than one risk factor at once, since CV events often have a multifactorial aetiology. The various classes of antihypertensive drugs exert differential effects on established non-BP risk factors, including high-density lipoprotein (HDL)-cholesterol, triglycerides, pulse rate, potassium levels and glucose levels. In addition, antihypertensive drugs vary in their duration of action, effect on central BP and their effect on BP variability. Therefore, it cannot be assumed that all antihypertensives exert equal CV protection, even with comparable clinic BP-lowering effects, although such BP-lowering effects are important.
ARBs for the treatment of hypertension
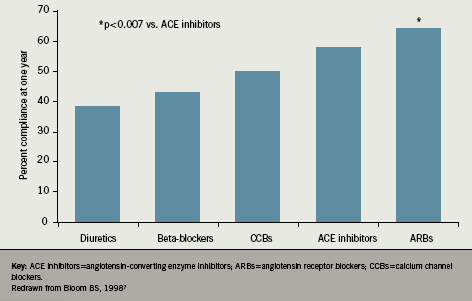
While diuretics are often used as first-line therapy in patients with hypertension, their use is associated with the lowest patient compliance, and compliance with beta-blocker therapy is not notably better. Incremental increases in patient compliance are seen for CCBs and ACE inhibitors, but the highest rate of patient compliance with antihypertensive therapy is seen with the ARBs (figure 3). However, it is uncertain whether these findings are explained by drug tolerability, financial incentives, newness of the product, selection bias or other factors.7
Initially, there were conflicting data regarding use of ARBs for the treatment of hypertension and even a claim that these drugs may increase CV events such as myocardial infarction (MI).8 However, subsequent systematic reviews and meta-analyses have refuted these findings. McDonald et al. evaluated the effect of ARBs on the risk of MI in patients at risk for CV events through a systematic review of controlled trials of ARBs. They identified 19 studies which included 31,569 patients: the use of ARBs was not associated with an increased risk of MI compared with placebo (odds ratio 0.94, 95% confidence interval [CI] 0.75 to 1.16), or with an increased risk of MI when compared with ACE inhibitors (odds ratio 1.01, 95% CI 0.87 to 1.16).9 Similarly, a meta-analysis by Volpe et al. evaluated the effects of treatment using an ARB on the risk of MI, CV and all-cause death, as compared with conventional treatment or placebo. Twenty trials were evaluated comprising 108,909 patients, and this study concluded that the risk of MI was similar in patients treated with an ARB compared with other antihypertensive drugs in a wide range of clinical situations.10
ARBs in hypertension and ventricular hypertrophy
Left ventricular hypertrophy (LVH) is a strong independent indicator of risk of CV morbidity and death in patients with hypertension. Dahlöf et al. aimed to establish whether selective blocking of angiotensin II with losartan or atenolol improves LVH beyond the reduction in BP, and whether this consequently reduced CV morbidity and death. Results showed that losartan reduced a composite end point of morbidity and death (driven predominantly by a reduction in stroke) to a greater extent than atenolol for a similar reduction in BP.11 It would appear that ARBs (in this case, losartan) confer benefits on LVH and CV risk, specifically stroke events, beyond just effectively controlling BP.
ARBs in hypertension and stroke
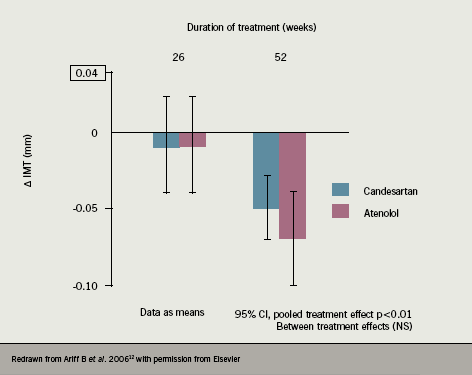
The Candesartan Atenolol Carotid Haemodynamics Endpoint Trial (CACHET) was conducted by Ariff et al. to investigate whether ARB treatment compared to beta-blocker treatment caused cardiac and large artery remodelling, and the relationship of any arterial remodelling to haemodynamic changes. Results showed that both candesartan (8 to 16 mg per day) and atenolol (50 to 100 mg per day) reduced intima-media thickness (IMT) and intima-media area (IMA) and increased distensibility to similar extents after 52 weeks of treatment. However, despite similar reductions in BP, treatment with atenolol resulted in a lesser reduction in left ventricular mass index, a decrease in lumen diameter and a reduction in carotid blood flow compared with candesartan. Therefore, candesartan demonstrated BP-independent effects on ventricular and carotid arterial structure, which may be a contributory factor to the beneficial effects of antihypertensive treatment with ARBs on some components of CV disease12 (figure 4).
The beneficial effects of ARBs on stroke risk but not CHD risk reduction can also be seen in the results of the Losartan Intervention For Endpoint reduction in hypertension (LIFE) study, which demonstrated superior stroke outcome for losartan versus atenolol beyond BP reduction.11
The ACCESS study13 was designed to assess the effects of ARB therapy within 36 hours after a stroke in patients with elevated BP. Cumulative 12-month mortality and the number of vascular events differed significantly in favour of candesartan versus placebo (odds ratio 0.475; 95% CI 0.252 to 0.895). The study concluded that early neurohumoral inhibition using an ARB has beneficial effects in cerebral and myocardial ischaemia and, unless contra-indicated, early antihypertensive therapy using candesartan is a well tolerated therapeutic option.
However, not all ARBs have shown consistent clinical benefits in various randomised clinical trials, perhaps reflecting differential effects on BP lowering. The VALUE trial was designed to test the hypothesis that, for the same BP control, valsartan would reduce cardiac morbidity and mortality more than amlodipine in hypertensive patients with a high CV risk. Results showed that BP was reduced by both valsartan and amlodipine treatments, but the effects of the amlodipine-based regimen were more pronounced, especially in the early period (BP 4.0/2.1 mmHg lower in amlodipine group compared to valsartan group after one month, and lower by 1.5/1.3 mmHg after one year; p<0.001 between groups). These BP differences were associated with a trend towards fewer fatal and non-fatal strokes in the amlodipine group (322 versus 281 in the valsartan and amlodipine groups, respectively, HR=1.15 [95% CI 0.98, 1.36], p=0.08).14 Similarly, the PRoFESS trial investigated the effect of lowering BP with the angiotensin receptor blocker, telmisartan within 120 days after a stroke. A total of 20,332 patients were enrolled who recently had an ischaemic stroke and the study evaluated the effects of therapy with telmisartan (80 mg daily) versus placebo. Results showed that therapy with telmisartan initiated after an ischaemic stroke and continued for 2.5 years did not significantly lower the rate of recurrent stroke, major CV events or diabetes compared with placebo.15
Diabetogenic potential of antihypertensive drugs
Both diuretics and beta-blockers induce adverse effects on glucose metabolism and may cause new‑onset diabetes (NOD). The size of this effect is variable within these two drug classes and is affected by drug dose. Elliott et al. undertook a systematic review to assess the effects of antihypertensive agents on the risk of NOD, including 22 clinical trials with 143,153 patients. The study concluded that the risk of NOD with antihypertensive drugs was lowest for ARBs and ACE inhibitors, followed by CCBs and placebo, beta-blockers and diuretics, in rank order16 (figure 5).
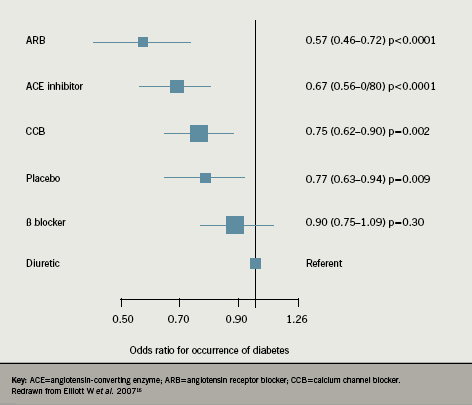
It is therefore recommended that the combination of a diuretic and beta-blocker should be avoided for the routine treatment of hypertension, except in cases where compelling reasons apply. Conversely, drugs that block the renin-angiotensin system appear to afford an important degree of protection against the onset of NOD, therefore, drugs such as ACE inhibitors or ARBs (that block the renin-angiotensin system) should usually form part of the cocktail of agents necessary to lower BP in patients with impaired glucose tolerance, and also in patients who already have type 2 diabetes.
Conclusions
Hypertension diagnosis and treatment has improved markedly in the UK in the past decade, with hypertension management being simplified by the publication of the NICE/BHS ‘ACD’ algorithm. Evidence shows that ARBs are better tolerated compared to the other major drug classes in the treatment of hypertensive patients. ARBs vary in terms of duration of action and BP‑lowering efficacy.
Overall, CV protective effects are similar between ACE inhibitors and ARBs, but compared with other agents there is some evidence that ARBs may offer better stroke protection and like ACE inhibitors, may be associated with a reduced risk of developing new-onset diabetes. There is no robust evidence that ARBs are associated with significantly increased CV events, including MI, compared to other antihypertensive drugs.
Conflict of interest
NP has served as consultant and received travel expenses, payment for speaking at meetings, or funding for research from several pharmaceutical companies, including Takeda.
Key messages
- Control of hypertension in the UK is improving, with good guidelines provided by the National Institute for Health and Clinical Excellence (NICE)/British Hypertension Society (BHS) ‘ACD’ algorithm
- Angiotensin receptor blockers (ARBs) demonstrate good efficacy in hypertension and a good safety profile: early fears about increased risk of myocardial infarction (MI) have been discredited by recent meta-analyses and trials
References
- Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S, Murray CJ (Comparative Risk Assessment Collaborating Group). Selected major risk factors and global and regional burden of disease. Lancet 2002;360(9343):1347–60.
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet 2005;365(9455):217–23.
- Lewington S, Clarke R, Qizilbash N, Peto R, Collins R (Prospective Studies Collaboration). Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 2002;360(9349):1903–13.
- MacMahon S, Neal B, Rodgers A. Blood pressure lowering for the primary and secondary prevention of coronary and cerebrovascular disease. Schweiz Med Wochenschr 1995;125(51-52):2479–86.
- Williams B, Poulter NR, Brown MJ et al. (British Hypertension Society). Guidelines for management of hypertension: report of the fourth working party of the British Hypertension Society, 2004-BHS IV. J Hum Hypertens 2004;18(3):139–85.
- Hypertension – full guideline. NICE/British Hypertension Society and National Collaborating Centre for Chronic Conditions 2006 (www.nice.org.uk/CG034)
- Bloom BS. Continuation of initial antihypertensive medication after 1 year of therapy. Clin Ther 1998;20(4):671–81.
- Verma S, Strauss M. Angiotensin receptor blockers and myocardial infarction. BMJ 2004;329(7477):1248–9.
- McDonald MA, Simpson SH, Ezekowitz JA, Gyenes G, Tsuyuki RT. Angiotensin receptor blockers and risk of myocardial infarction: systematic review. BMJ 2005;331(7521):873.
- Volpe M, Tocci G, Sciarretta S, Verdecchia P, Trimarco B, Mancia G. Angiotensin II receptor blockers and myocardial infarction: an updated analysis of randomized clinical trials. J Hypertens 2009;27(5):941–6.
- Dahlöf B, Devereux RB, Kjeldsen SE et al. (LIFE Study Group). Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 2002;359(9311):995–1003.
- Ariff B, Zambanini A, Vamadeva S et al. Candesartan- and atenolol-based treatments induce different patterns of carotid artery and left ventricular remodeling in hypertension (CACHET Trial). Stroke 2006;37(9):2381–4.
- Schrader J, Lüders S, Kulschewski A et al. (Acute Candesartan Cilexetil Therapy in Stroke Survivors Study Group). The ACCESS Study: evaluation of Acute Candesartan Cilexetil Therapy in Stroke Survivors. Stroke 2003; 34(7):1699–703.
- Julius S, Kjeldsen SE, Weber M et al. (VALUE trial group). Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004;363(9426):2022–31.
- Yusuf S, Diener HC, Sacco RL et al. (PRoFESS Study Group). Telmisartan to prevent recurrent stroke and cardiovascular events. N Engl J Med 2008;359(12):1225–37.
- Elliott WJ, Meyer PM. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 2007;369(9557):201–07.
