Heart failure (HF) accounts for 5% of all emergency hospital admissions in the UK. To ensure cost-effectiveness, the potential for any intervention to reduce admissions must be balanced against its required investment. This economic analysis compared cost-effectiveness of home- versus hospital-based exercise training as delivered within a randomised-controlled trial (RCT) for HF.
The additional costs of delivering eight weeks of home- versus hospital-based training for 46 people with HF, within an established cardiac rehabilitation service, were balanced against emergency hospital admission costs incurred by home-training (n=15), hospital-training (n=15) and control (n=16) groups over five years.
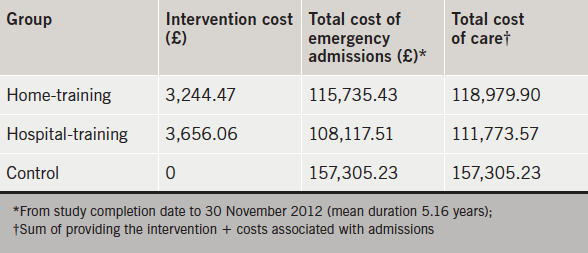
The total cost of home-training was £3,244.47 (£196.53 per patient) – much of which was a fixed cost attributed to producing the home-training package. Hospital-training cost £3,656.06 (£221.58 per patient). Over five years, total admission costs for controls (of £157,305.23) were considerably higher than for both home- (£115,735.43) and hospital- (£108,117.51) training groups.
In conclusion, both training programmes incurred similar costs, which were offset by a reduction in emergency admission costs, compared with controls. Although hospital-training offered greater potential for reducing admission costs, with larger patient numbers, the cost of home-training per patient would decrease, increasing its likelihood of being the more cost-effective option.
Introduction
Heart failure (HF) costs the National Health Service (NHS) £625 million per year and accounts for 5% of all emergency medical hospital admissions in the UK.1,2 Interventions with the potential to reduce admissions and lessen this economic burden are always of clinical interest; however, any such potential for cost-avoidance must always be balanced against the financial cost of the intervention.
While there is evidence to suggest that exercise training may reduce emergency admissions in HF,3,4 this research invariably focuses on training that includes a hospital-based component. Though exercising at home may offer a more practical rehabilitation option for this frailer, more elderly cardiac group,5-7 the potential of home-training to reduce emergency hospital admissions in HF has neither been established, nor compared with that of hospital-training. Further, the cost of delivering the two types of training for HF within the framework of the NHS has not been compared.3,7

The purpose of this economic analysis was to compare the cost-effectiveness of home- versus hospital-based exercise training (versus control) as delivered within a randomised-controlled trial (RCT) in patients with HF.5,6 This analysis balanced the additional short-term cost of running this study within an established comprehensive cardiac rehabilitation service already offered to other cardiac groups, against longer-term hospital admission costs incurred by all three groups over five years after the RCT.
Data collection for the RCT took place between May 2007 and August 2008, and was conducted entirely within NHS Ayrshire and Arran, Scotland. In the RCT (figure 1), 60 patients with HF were randomised into three groups: home-training (n=20), hospital-training (n=20), and control (n=20). For all groups, the intervention period lasted eight weeks. Exercise capacity, quality of life (QoL), and physical activity outcomes were collected from all participants at baseline, and post-intervention. No structured training interventions were provided after this point, and there were no adverse events during training. A calculation derived from a similar UK trial8 indicated that 45 people were required to complete the RCT for exercise capacity and QoL outcomes to be adequately powered. The RCT was completed by 46 individuals (n=15 from hospital-training, n=15 from home-training, n=16 from control), and data from only these participants is relevant to this cost analysis.
Methods
Costing the interventions
To ensure consistency with National Institute for Health and Care Excellence (NICE),9,10 costs were taken from an NHS perspective and a total cost for each training intervention calculated by focusing upon the associated NHS resource use. Salary costs were based on NHS salaries (Agenda for Change [AfC], 2013/14), using midpoints of the salary banding scales, and represent the gross cost to the NHS employer (i.e. including National Insurance and Superannuation [13.5%] contributions). Staff groups involved were either AfC band 8a (salary range £47,748–£57,712; midpoint £53,555), AfC band 7 (salary range £37,247–£49,400; midpoint £46,115), or AfC band 3 (salary range £19,290–£23,004; midpoint £21,786), and hourly rates were based upon a 37.5-hour week.
The hospital-training intervention was delivered as a one-hour, interval training, aerobic circuit class, twice per week, for eight weeks.5,6 At each class, a senior cardiac rehabilitation physiotherapist (AfC band 7), physiotherapy technical instructor (AfC band 3) and a senior cardiac nurse (AfC band 7) were present.
The home-training intervention consisted of a one-hour, interval training, aerobic circuit DVD which participants completed twice per week, for eight weeks. The cost of producing the DVD was £1.50 per DVD, and the cost of filming and producing the DVD was estimated at one week of senior cardiac rehabilitation physiotherapist (AfC band 7) time, and one week of senior medical photography (AfC band 8a) time. The home group were monitored by a senior cardiac rehabilitation physiotherapist (AfC band 7) by telephone, twice during their eight-week intervention (estimated as two 20-minute calls, plus 10 minutes documentation, i.e. one hour per patient).
To guide training intensity, a heart rate monitor was purchased for every participant undertaking either home- or hospital-based training. Both training interventions incurred additional costs, which are difficult to allocate with such small patient numbers. These include booklets and support leaflets, and reimbursement of travel expenses. To account for these unallocated costs in the analysis, the total estimated cost of each intervention was inflated by 10%.
The cost of usual care was not calculated as this was standard to all three groups. Usual care included specialist HF nursing input, which in itself has been found to generate a net saving in admission costs of £1,826 per patient;2 thus, this economic analysis examined the cost-effectiveness of exercise training over and above this service. Additionally, time invested to obtain baseline and post-intervention measurement of exercise capacity, QoL and physical activity level was almost identical across all three groups, therefore, excluded from analysis.
Admission costs
To investigate emergency bed days incurred, case notes of participants from all three groups were checked for emergency HF, cardiovascular, or general medical admissions between completion of the RCT and 30 November 2012, and these data were cross-checked against locally stored data provided by the Health Intelligence function within NHS Ayrshire and Arran. Bed days incurred by each group were combined with Information Services Division (ISD) 2011/12 references in order to cost admissions. Differences in group size were accounted for through standardisation. Deaths were not excluded as they were similar across the groups (hospital-training three; home-training three; control two).
Economic analysis
Economic evaluation refers to comparative analysis of alternative courses of action in terms of both cost and consequence.11 To be meaningful, the analysis should follow an incremental approach and examine the additional costs that one intervention, service or programme imposes over another, compared with the additional effects or benefits it achieves.11 An incremental analysis approach was adopted in the present paper; the additional cost of the training interventions (as provided for n=15 per group) over usual care was compared with any potential notional saving made through emergency hospital admission avoidance. Further, cost-effectiveness (costs incurred and potential cost-avoidance) associated with the two training interventions was compared. To explore robustness of the results (i.e. account for underestimation in this analysis, or overspend in clinical practice) the cost of the more cost-effective intervention was inflated by up to 100%.
Results
Patient characteristics
Characteristics of all 46 participants are shown in table 1. A full list of inclusion and exclusion criteria for the RCT has been published previously.5,6

Cost of the interventions
Resources incurred through the interventions are shown in table 2. The estimated total cost of delivering home-based training was £3,244.47 (£196.53 per patient), while the total cost of hospital-based training was £3,656.06 (£221.58 per patient).

Admission costs

Over five years, total admission costs for controls (of £157,305.23) were considerably higher than for both training groups (£115,735.43 for home-training, £108,117.51 for hospital-training). In particular, the control group incurred more HF-related and general medical admissions. For all three groups, most admissions occurred due to HF (table 3).
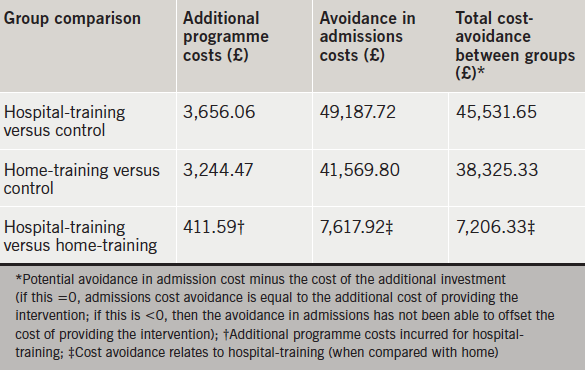
Although the two training interventions were more expensive than providing usual care, the sum total cost of care for patients in the two training groups (i.e. intervention costs, plus admission costs) was still less than for the control group (table 4). Table 5 shows that hospital-training appeared to be the more cost-effective intervention, generating potential cost-avoidance of £45,531.65 compared with controls, and £7,206.33 compared with home-training. The sensitivity analysis (table 6) shows that even if the cost of delivering hospital-training was increased by 100%, the intervention still offered a potential total cost avoidance of £3,550.27 over home-training.
Discussion
The purpose of this economic analysis was to examine the potential cost-effectiveness of home- versus hospital-based exercise training (versus control) as part of an RCT for HF delivered within an established comprehensive cardiac rehabilitation service already offered to other cardiac groups. The analysis found that the total cost of home- and hospital-based training was similar, and that both training groups offset these costs over five years by reducing emergency hospital admission costs, compared with usual care.

In studies of those with other cardiac diagnoses, the costs associated with home- and hospital-based exercise training are generally comparable, and like the present analysis, equate to approximately £200 per patient.7 Further, the average cost of comprehensive cardiac rehabilitation in its entirety, i.e. accounting for all inpatient and outpatient components, and all disciplines involved in delivery, has been estimated as between £350 (staff only) and £490 (total) per patient with any cardiac diagnosis.12,13 Thus, if the cost per patient for the exercise component used in the RCT – delivered as an ‘add-on’ within the framework of an established cardiac rehabilitation service – was inflated to £490, to incorporate all other aspects of cardiac rehabilitation, including pre- and post-training assessment and totalling £7,350 for 15 patients, whether patients chose to undertake their rehabilitation at home or to attend hospital classes, the cost-avoidance achieved in terms of emergency hospital admissions would still render this expense potentially cost-effective.
For this sample, using the costs outlined in table 2, hospital-training appeared to be the more cost-effective intervention generating a potential cost-avoidance of £45,531.65 compared with the control group, and £7,206.33 compared with home-training. Even when its cost was inflated by 100%, hospital-training still demonstrated a potential cost-avoidance of £3,550.27 compared with home-training.
However, much of the cost incurred by the home programme was attributable to staffing input required to create the DVD. This would remain a non-recurring, fixed cost regardless of the number of participants to whom the intervention was provided – if the group sizes were expanded, the cost per patient for providing home-training would decrease, while the cost per patient for hospital-based training would remain relatively constant. Indeed, excluding the cost of developing the DVD, the ongoing cost of delivering home-training for 15 individuals (including 10% unallocated) is only £996.47 (£64.43 per patient), which is substantially less than the cost of providing ongoing hospital-training.
As advocated by NICE,9,10 this analysis used an NHS perspective to calculate the costs of training, however, analysing from a societal perspective enables a wider set of costs to be included – including the cost to the patient in terms of travel expenses and time, work days lost to attend clinics or follow-up, and cost-implications for other organisations such as private providers or social care.11,14 Thus, although the hospital-training group’s travel expenses were reimbursed and incorporated within ‘unallocated costs’, it may be expected that the wider cost of training was greater for them than for those exercising at home, and future research could employ a societal costing perspective to provide a wider analysis of the relative cost-effectiveness of the training programmes.
The RCT found that both training programmes significantly improved participants’ exercise capacity, though neither significantly improved QoL or total daily physical activity level.5,6 Though not statistically different, the improvement in exercise capacity was larger for hospital-training (31% vs. 16% for home-training) and only the hospital group maintained their QoL scores and significantly improved their daily walking endurance.5,6
The larger physical gains from hospital-training may have been related to its better adherence (86% vs. 77% for home-training), combined with the fact that professional and peer support may have encouraged the hospital group to work harder than those exercising alone at home – resulting in a higher training ‘dose’.6 Peer support and/or the larger physical improvement with hospital-training was thought to have helped maintain QoL, which was considered to be clinically important, given the psychosocial decline that tends to occur with HF progression.6 Thus, perhaps the significant improvement in exercise capacity with training enabled participants to stay fitter, and, therefore, more able than the control group to avoid costly emergency hospital re-admissions – and perhaps the larger physical and wider psychosocial gains elicited by hospital-training reduced its admission costs further.
Higher admission costs incurred by the control group may have been related to participants’ characteristics, however table 1 shows that they were actually the youngest group and that they presented with similar characteristics to the other two groups. Conversely, the hospital-training group were the eldest, yet had the lowest admission costs. It is unsurprising that, for all three groups, most admissions were HF-related, but noteworthy that the control group’s general medical admission costs were considerably higher, indicating that perhaps other comorbidities, not included in table 1 – which might never have been improved with exercise-based rehabilitation – may have been responsible.
Finally, results were obtained from a small sample of 46, which was too small to have performed any meaningful survival analysis, and future studies examining effects of training upon mortality and morbidity in HF should use larger numbers to ensure validity of data. Indeed, although adequately powered for the outcomes used in the original RCT, the small sample used in this economic analysis certainly must be acknowledged as a limitation when considering and applying its findings, especially in relation to the effect that larger patient numbers would have upon reducing the per patient cost of home-based training.
Conclusion
The purpose of this economic analysis was to examine the potential cost-effectiveness of home versus hospital-based exercise training (versus control) as part of an RCT for HF delivered within an established comprehensive cardiac rehabilitation service. The analysis shows that both training programmes incurred similar costs for 15 patients over the eight-week intervention period, and both offset these costs through a reduction in emergency hospital admissions over five years, when compared with usual care. Although hospital-training offered greater potential for reducing admission costs, with larger patient numbers, the cost of home-training per patient would decrease, increasing its likelihood of being the more cost-effective option
Conflict of interest
None declared.
Key messages
- In a randomised-controlled trial (RCT) of exercise training for 46 individuals with heart failure (HF), training incurred a similar cost, whether delivered in the patient’s home (£196.53 per patient) or in a supervised hospital setting (£221.58 per patient)
- Much of the home-training cost was fixed – attributed to production of the home-training package
- Over five years after the RCT, total hospital admission costs for a control group (£157,305.22) were considerably higher than for both training groups (£115,735.43 for home-training, £108,117.51 for hospital-training) – thus, both training interventions offset their investment costs by reducing emergency hospital admissions
- Although hospital-training offered greater potential for reducing admission costs, with larger patient numbers, the cost of home-training per patient would decrease, increasing its likelihood of being the more cost-effective option
References
1. National Institute for Health and Care Excellence. Chronic heart failure: management of chronic heart failure in adults in primary and secondary care. CG108. London: NICE, 2010. Available from: http://www.nice.org.uk/guidance/CG108
2. Scottish Heart Failure Nurse Forum. Review of specialist heart failure nurse services in Scotland. Edinburgh: Chest Heart & Stroke Scotland, 2013. Available from: http://www.bhf.org.uk/pdf/SHFNF_Review_2013.pdf
3. Davies EJ, Moxham T, Rees K et al. Exercise based rehabilitation for heart failure. Cochrane Database Syst Rev 2010;(4):CD003331. http://dx.doi.org/10.1002/14651858.CD003331.pub3
4. O’Connor CM, Whellan DJ, Lee KL et al. Efficacy and safety of exercise training in patients with chronic heart failure. JAMA 2009;301:1439–50. http://dx.doi.org/10.1001/jama.2009.454
5. Cowie A, Thow MK, Granat MH, Mitchell SL. A comparison of home and hospital-based exercise training in heart failure: immediate and long-term effects upon physical activity level. Eur J Cardiovasc Prev Rehabil 2011;18:158–66. http://dx.doi.org/10.1177/1741826710389389
6. Cowie A, Thow MK, Granat MH, Mitchell SL. Effect of home versus hospital-based exercise training in chronic heart failure. Int J Cardiol 2012;158:296–8. http://dx.doi.org/10.1016/j.ijcard.2012.04.117
7. Taylor RS, Dalal H, Jolly K, Moxham T, Zawada A. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst Rev 2010;(1):CD007130. http://dx.doi.org/10.1002/14651858.CD007130.pub2
8. Austin J, Williams R, Ross L, Moseley L, Hutchison S. Randomised controlled trial of cardiac rehabilitation in elderly patients with heart failure. Eur J Heart Fail 2005;7:411–17. http://dx.doi.org/10.1016/j.ejheart.2004.10.004
9. National Institute for Health and Care Excellence. Guide to the methods of technology appraisal. London: NICE, 2013. Available from: http://www.nice.org.uk/aboutnice/ howwework/devnicetech/guideto themethodsoftechnologyappraisal.jsp
10. Claxton K, Walker S, Palmer S, Sculpher M. Appropriate perspectives for healthcare decisions. CHE Research Paper 54. York: Centre for Health Economics, 2010. Available from: http://www.york.ac.uk/che/pdf/rp54.pdf
11. Drummond MF, O’Brien B, Stoddart GL, Torrance GW. Methods for the economic evaluation of health care programmes. Second edition. Oxford: Oxford University Press, 2001.
12. Beswick AD, Rees K, Griebsch I, Taylor FC, Burke M, West RR. Provision, uptake and cost of cardiac rehabilitation programmes: improving services to under-represented groups. Health Technol Assess 2004;8:iii–iv, ix–x, 1–152. http://dx.doi.org/10.3310/hta8410
13. National Institute for Health and Care Excellence. NICE support for commissioning quality improvement and service redesign – cardiac rehabilitation services. London: NICE, 2013. Available from: http://www.nice.org.uk/usingguidance/commissioningguides/cardiacrehabilitation/cardiacrehabilitation.jsp
14. Jolly K, Taylor R, Lip GY et al. The Birmingham rehabilitation uptake maximisation study (BRUM). Home-based compared with hospital-based cardiac rehabilitation in a multi-ethnic population: cost-effectiveness and patient adherence. Health Technol Assess 2007;11:1–118. http://dx.doi.org/10.3310/hta11350
15. Criteria Committee of the New York Heart Association. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. Ninth edition. Boston, MA: Little, Brown and Company, 1994.

