Correspondence from the world of cardiology
Dear Sirs,
We read with interest the article by Dr Ward in the BJC, and we greatly welcome his refreshing physiological overview of the jugular venous (JV) pulse.1 We might, however, not have been quite so dismissive of modern technology. Although Paul Wood was concerned not to place too much reliance on machines (“… we are in danger of losing our clinical heritage and of pinning too much faith in figures thrown up by machines.”),2 the superb film cited (http://archive.org/details/Thejugularvenouspulse-wellcome) makes it clear that he, too, was not averse to using the technology of the day where appropriate.
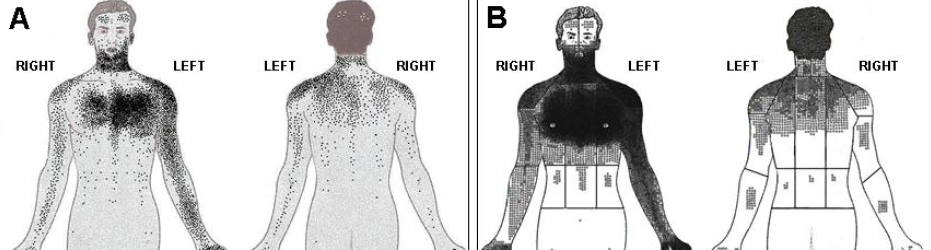
The height of the JV pressure is an important prognostic marker in patients with heart failure.3 However, many doctors are now not familiar with its measurement, and the reported height of the JV pressure is not highly reproducible when measured clinically.4 It is straightforward to make an estimate of right atrial pressure from the inferior vena cava (IVC) diameter particularly with the widespread availability of echocardiography. In ambulatory heart failure patients, echocardiographic evaluation of IVC diameter provides similar prognostic information to that obtained from natriuretic peptides.5 An ultrasound probe can also be used in the neck of patients and can tell what even a highly skilled doctor might have missed if, for instance, the habitus of the patient does not allow a simple identification of the internal jugular vein. Different methods are possible. By using a 10 MHz ultrasound probe, we described how the ratio between JV diameter during a Valsalva manoeuvre to that at rest (figure 1) identifies those ambulatory patients with heart failure and raised natriuretic peptides, but also with more severe right ventricular dysfunction and raised pulmonary artery pressure.6 We have also recently presented preliminary results, showing that this method can provide independent prognostic information.7 Some other researchers have measured the cross-sectional area of the internal jugular vein, rather than its diameter. Again, the response of the vein area to respiratory manoeuvres can easily identify those patients who have elevated right atrial pressures invasively measured.8 Other devices are currently being explored and it seems they can provide accurate and reproducible non-invasive reading of the right atrial pressure in most of the cases.9
Although we agree with Ward that continuing training on JV pressure assessment is mandatory, we have to recognise that for many clinicians it is a difficult sign to elicit and that modern technology offers a reliable substitute for the fallible clinician!
Conflict of interest
None declared.
Pierpaolo Pellicori
Research Fellow in Cardiology
(pierpaolo.pellicori@hey.nhs.uk)
Andrew L Clark
Chair of Clinical Cardiology and Honorary Consultant Cardiologist
Department of Cardiology, Hull York Medical School, Hull and East Yorkshire Medical Research and Teaching Centre, Castle Hill Hospital, Cottingham, Kingston upon Hull, HU16 5JQ
References
1. Ward D. Where has the jugular venous pressure gone? Br J Cardiol 2014;21:49–50. http://dx.doi.org/10.5837/bjc.2014.014
2. Wood P. Diseases of the Heart and Circulation. London: Eyre and Spottiswoode, 1950.
3. Drazner MH, Rame JE, Stevenson LW, Dries DL. Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med 2001;345:574–81. http://dx.doi.org/10.1056/NEJMoa010641
4. Cook DJ. Clinical assessment of central venous pressure in the critically ill. Am J Med Sci 1990;299:175–8. http://dx.doi.org/10.1097/00000441-199003000-00006
5. Pellicori P, Carubelli V, Zhang J et al. IVC diameter in patients with chronic heart failure: relationships and prognostic significance. JACC Cardiovasc Imaging 2013;6:16–28. http://dx.doi.org/10.1016/j.jcmg.2012.08.012
6. Pellicori P, Kallvikbacka-Bennett A, Zhang J et al. Revisiting a classical clinical sign: jugular venous ultrasound. Int J Cardiol 2014;170:364–70. http://dx.doi.org/10.1016/j.ijcard.2013.11.015
7. Pellicori P, Bennett A, Zhang J et al. Echocardiographic assessment of jugular vein distensibility in patients with heart failure and its prognostic significance. Eur J Heart Fail 2014;16(suppl 2):291. http://dx.doi.org/10.1002/ejhf.93_18
8. Simon MA, Kliner DE, Girod JP et al. Detection of elevated right atrial pressure using a simple bedside ultrasound measure. Am Heart J 2010;159:421–7. http://dx.doi.org/10.1016/j.ahj.2010.01.004
9. Pellicori P, Bennett A, Lomax S et al. A novel non-invasive method of assessing right atrial pressure. A report from the SICA-HF study. Eur J Heart Fail 2014;16(suppl 2):321. http://dx.doi.org/10.1002/ejhf.93_21
