Palpitations are a common symptom leading to primary care consultation. Establishing a symptom-rhythm correlation is important for providing a diagnosis. The Kardia Mobile personalised smartphone electrocardiogram (ECG) can provide patient-driven real-time ECG recording over extended periods. We investigated if this device might provide an effective alternative to conventional ECG recorders as the first-line investigation of low-risk palpitations.
Patients referred to our institution for investigation of intermittent palpitations but without syncope were supplied with a Kardia Mobile device if they had access to a compatible smartphone. Patients were asked to record an ECG when symptomatic.
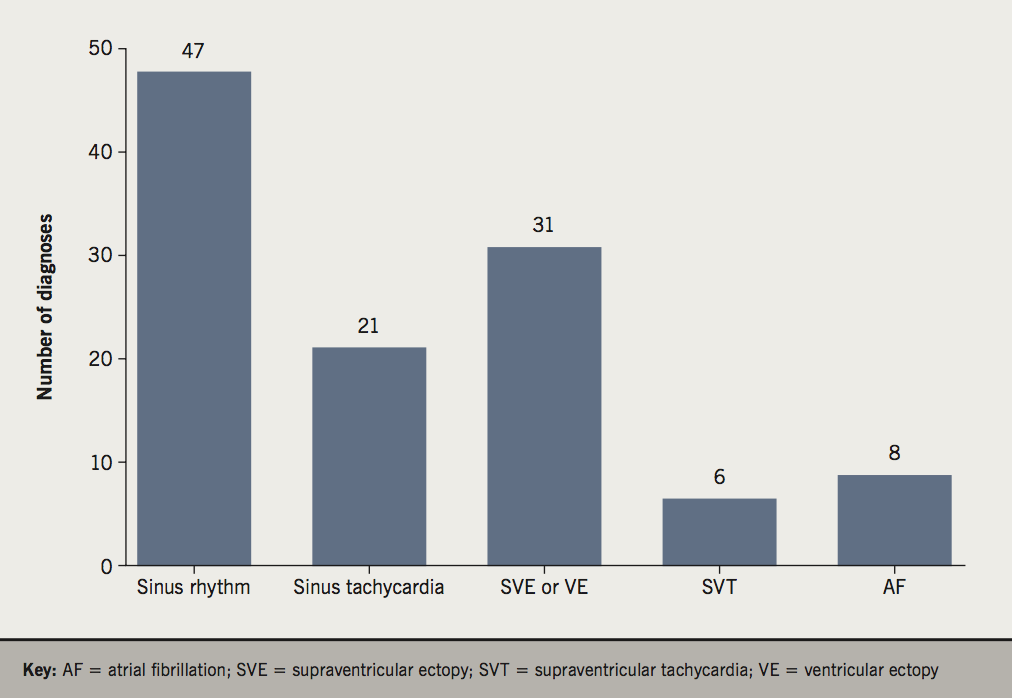
Between March 2015 and June 2016, 148 patients were issued with a Kardia Mobile: 113 (76.4%) patients made symptomatic recordings during this period. A symptom-rhythm correlation was possible for all patients who submitted downloads. Median time to diagnosis was nine days (1–287 days). Diagnoses were: sinus rhythm n=47 (41.6%), sinus tachycardia n=21 (18.6%), supraventricular/ventricular ectopics n=31 (27.4%), atrial fibrillation n=8 (7.1%), and supraventricular tachycardia n=6 (5.3%).
In conclusion, the Kardia Mobile diagnosed the cause of intermittent palpitations in the majority of patients referred for specialist evaluation. Use of the Kardia Mobile may permit patients with palpitations to be evaluated in primary care.

Introduction
Palpitations are a common symptom in the general population. A significant proportion of individuals experiencing palpitations will present to their primary care provider for advice. Many will be referred to a cardiologist for specialist evaluation accounting for up to one-fifth of all cardiology referrals.1-4 Usually, morbidity and mortality associated with palpitations is low. The minority of patients will have an arrhythmia.5 Even in the absence of underlying arrhythmia, unexplained symptoms can have a significant impact on quality of life, and may lead to anxiety.6
Palpitations are typically intermittent, and a diagnosis can only be made through establishing a symptom-rhythm correlation. Various techniques for the investigation of palpitations are available. The joint Practice Guidelines from the American College of Cardiology (ACC)/American Heart Association (AHA)/European Society of Cardiology (ESC) recommend a 12-lead electrocardiogram (ECG) as first line in all patients with palpitations.7 Consensus of the Heart Rhythm Society (HRS) and guidelines published by the UK National Institute for Health and Care Excellence (NICE) recommend the use of ambulatory electrocardiographic (AECG) monitoring (either Holter or event monitoring) in patients with frequent but transient symptoms.8-9 As symptoms tend to be intermittent, reported diagnostic yield of 24-hour AECG monitoring is typically only between 15% and 39%.8,10-13 A higher rate of diagnosis can be achieved with more prolonged ambulatory monitoring of up to 14 days, but compliance is often compromised due to the irritation caused by the device electrodes, with the median actual use being 11.1 days.8,13,14 In addition, the high volumes of data produced require more time for technician analysis and interpretation. Prolonged continuous monitoring can be achieved with an implantable loop recorder, but is relatively expensive, requires an invasive procedure, and has a cosmetic impact, which might be particularly relevant in a younger population.8,14,15
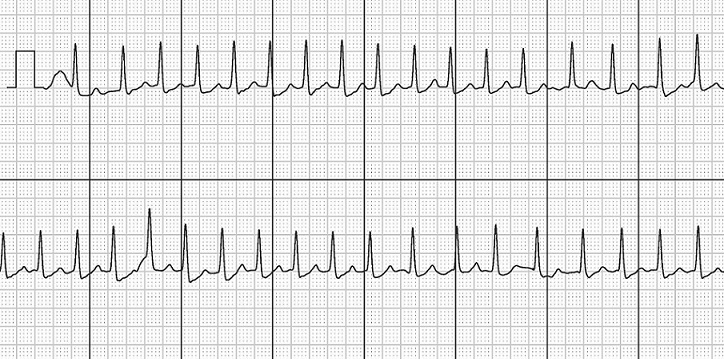
Smartphone usage has increased exponentially in the last decade. Approximately 80% of adults in the USA and UK are regular smartphone users with an estimated 1.75 billion users worldwide.16,17 Smartphones are already successfully used for telemedicine, collecting and transferring data, such as blood pressure and oxygen saturations, for remote clinical review.18 The Kardia Mobile personal ECG device (AliveCor, San Francisco, USA) is a validated Food and Drug Administration (FDA) approved, Conformité Européene (CE) marked, single-channel ECG recorder that can be paired with a smartphone, permitting intermittent, non-invasive monitoring over prolonged time periods. The device consists of electrode plates held between fingers of each hand (figure 1). The device transmits data ultrasonically, which is detected by the smartphone microphone. These data are then reconstructed into an ECG by the Kardia App software (figure 2). The Kardia Mobile (previously called AliveCor) was initially developed for detection of atrial fibrillation (AF) for which the automatic diagnostic algorithm has excellent sensitivity and specificity.19 It has been successfully used for population screening for AF in various settings.14 Feasibility for use on other rhythm disorders including supraventricular tachycardia (SVT) has been investigated elsewhere.17 The advantage of the Kardia over conventional monitoring devices for the broader investigations of palpitations has yet to be fully tested, but the device is supported for clinical use in a NICE technology appraisal.19,20
We sought to examine the acceptability and suitability of the Kardia Mobile as an alternative to traditional AECG in the initial investigation of palpitations.
Methods
From March 2015 to June 2016 our institution (UK, District General Hospital) used the Kardia Mobile as an alternative to wearable ambulatory ECG monitors for the initial investigation of intermittent palpitations. Inclusion criteria were patients referred to a cardiologist for investigation of palpitations occurring less than daily with (a) access to a compatible smartphone and (b) willingness and ability to use a device. Patients with a history of syncope were excluded. The project was registered with our institution’s internal clinical governance board.
Patients were supplied with a Kardia Mobile device and the software downloaded to their smartphone. A demonstration of the device was given. Patients were asked to use the device when experiencing palpitations. The ECG was automatically uploaded to a secure database. Initial interpretation of recordings was made by a cardiac physiologist, with diagnosis confirmed by a cardiologist. Data regarding patient demographics, symptoms and correlating rhythm were collated in a spreadsheet. Use of the device continued until a symptom-rhythm correlation was established and ECG diagnosis made.
Results
There were 148 patients (53 male, 95 female; average age 41 years, range 7 to 78) issued with a Kardia between March 2015 and June 2016. The median period of use of the device was 244 days (range 4–484). In total, 113 (76.4%) patients made symptomatic recordings. One patient (0.68%) returned the device before a diagnosis could be made because they reported an audible high-pitch noise from the device and another patient (0.68%) misplaced their Kardia Mobile. A total of 516 symptomatic downloads were made of which 10 (1.94%) were deemed uninterpretable, but all subsequent downloads were of diagnostic quality.
Symptomatic recordings related to sinus rhythm in 41.6%, supraventricular (SVE) or ventricular ectopy (VE) in 27.4%, sinus tachycardia (heart rate >100 bpm) in 18.6%. AF and SVT were detected in 7.1% and 5.3% respectively (figure 3).
The median time to diagnosis in those submitting symptomatic downloads was nine days (1–287 days). In the eight patients diagnosed with AF the median time to diagnosis was 12 days (1–66 days).
Discussion
In our cohort of patients with intermittent palpitations, use of the Kardia Mobile enabled the correlation of symptoms with heart rhythm in the bulk (76%) of individuals. This compares favourably to the reported diagnostic yield of 24-hour Holter recordings.21 In most cases no significant cardiac rhythm disturbance was found; patients were reassured, and further investigations avoided. Nonetheless, in a significant number of patients (12.4% with AF/SVT) an important arrhythmia was identified. The early detection of AF (median 12 days) allowed prompt initiation of anticoagulant treatment for stroke prevention and the establishment of a forward management plan. This time to diagnosis compares very favourably with registry data, where there is reportedly a mean delay of 1.7 years between patients reporting AF symptoms and diagnosis.22
Traditional methods of ECG recording over a fixed period in an attempt to capture an episode of palpitations provide poor diagnostic yields, incur diagnostic delays, and require considerable investment of time and financial resources.10-14 Failure to establish a timely diagnosis can result in repeated presentations to healthcare providers, cumulative costs, increased patient anxiety, and potential ongoing exposure to arrhythmias, including AF with the inherent thromboembolic risk.
The widespread uptake of smartphones makes the Kardia Mobile an appealing method for investigating intermittent palpitations in the absence of syncope. In our experience, the vast majority of patients were able to use the device at the time of symptoms, and a symptom-rhythm correlation was possible for all patients who submitted recordings. The device was also well tolerated, with only a single patient returning the device prematurely.
In the UK, there is support for the use of Kardia Mobile from both NICE and the NHS Innovation Accelerator (NIA) programme. The cost of the re-usable device ($99/£90) compares favourably with the cost of traditional event monitoring. Its simplicity of use and interpretation make it particularly suitable for the primary care setting. This approach could permit affordable and timely means for the first-line investigation of palpitations.
One limitation of using this method is the relatively lower rate of smartphone usage in the older population. Only two patients in our cohort were aged 75 years or over. Patients also need to follow the correct procedure to record interpretable ECGs.
Conclusion
We have demonstrated the utility of the Kardia Mobile in the diagnosis of intermittent palpitations in a low-risk population. Based on our findings we propose that many patients presenting with intermittent palpitations could be investigated in primary care. The minority of patients diagnosed with an arrhythmia can then be triaged appropriately allowing cardiologists to target patients who need their expertise. There is the potential to reduce the time to diagnosis of AF and shorten delays to treatment, thereby reducing stroke risk and improving symptom control. Reducing delays in diagnosis of arrhythmia or reassurance of normal heart rhythm will improve the patient experience. We plan to expand this service to primary care providers in our locality and further evaluate this hypothesis.
Key messages
- Palpitations are a common symptom leading to primary care consultation
- Using current methods, correlating symptoms with rhythm can be difficult
- Kardia Mobile provides convenient patient-driven electrocardiogram (ECG) recording over extended periods
Acknowledgements
We wish to thank the staff in the cardiology department at St. Richard’s Hospital, Chichester, for their support in this project.
Conflict of interest
None declared.
References
1. Abbott AV. Diagnostic approach to palpitations. Am Fam Physician 2005;71:743–50. Available from: http://www.aafp.org/afp/2005/0215/p743.html
2. Messineo FC. Ventricular ectopic activity: prevalence and risk. Am J Cardiol 1989;64:53J–56J. https://doi.org/10.1016/0002-9149(89)91200-9
3. Kroenke K, Arrington ME, Mangelsdorff AD. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch Intern Med 1990;150:1685–9. https://doi.org/10.1001/archinte.150.8.1685
4. Knudson MP. The natural history of palpitations in a family practice. J Fam Pract 1987;24:357–60.
5. Weber BE, Kapoor WH. Evaluations and outcomes of patients with palpitations. Am J Med 1996;100:138–48. https://doi.org/10.1016/S0002-9343(97)89451-X
6. Barsky AJ, Cleary PD, Coeytaux RR et al. The clinical course of palpitations in medical outpatients. Arch Intern Med 1995;155:1782–8. https://doi.org/10.1001/archinte.1995.00430160124012
7. Blomstrom-Lundqvist C, Sheinman MM, Aliot EM et al. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias – executive summary. J Am Coll Cardiol 2003;42:1493–531. https://doi.org/10.1016/j.jacc.2003.08.013
8. Antonio R, Franco G, Lennart B et al. Management of patients with palpitations: a position paper from the European Heart Rhythm Association. Europace 2011;13:920–34. https://doi.org/10.1093/europace/eur130
9. National Institute for Health and Care Excellence. NICE clinical knowledge summaries. Palpitations. London: NICE, May 2015. Available from: https://cks.nice.org.uk/palpitations#!topicsummary [accessed June 2017].
10. Zimetbaum PJ, Josephson ME. The evolving role of ambulatory arrhythmia monitoring in general practice. Ann Intern Med 1999;150:848–56. https://doi.org/10.7326/0003-4819-130-10-199905180-00020
11. Scherr D, Dalal D, Henrikson CA et al. Prospective comparison of the diagnostic utility of a standard event monitor versus a ‘leadless’ portable ECG monitor in the evaluation of patients with palpitations. J Interv Card Electrophysiol 2008;22:39–44. https://doi.org/10.1007/s10840-008-9251-0
12. Zimetbaum PJ, Kim KY, Josephson ME et al. Diagnostic yield and optimal duration of continuous-loop event monitoring for the diagnosis of palpitations. Ann Intern Med 1998;28:890–5. https://doi.org/10.7326/0003-4819-128-11-199806010-00002
13. Barrett PM, Komatireddy R, Haaser S et al. Comparison of 24-hour Holter monitoring with 14-day novel adhesive patch electrocardiographic monitoring. Am J Med 2014;127:95.e11–95.e17. https://doi.org/10.1016/j.amjmed.2013.10.003
14. Haberman ZC, Jahn RT, Bose R et al. Wireless smartphone ECG enables large-scale screening in diverse populations. J Cardiovasc Electrophysiol 2015;26:520–6. https://doi.org/10.1111/jce.12634
15. Kanjwal K, Figueredo VM, Karabin B, Grubb BP. The implantable loop recorder: current uses, future directions. The Journal of Innovations in Cardiac Rhythm Management 2011;2:215–22. Available from: http://www.innovationsincrm.com/cardiac-rhythm-management/2011/march/60-implantable-loop-recorder-uses-and-directions
16. PEW Research Centre. Mobile fact sheet. Available at: http://www.pewinternet.org/fact-sheet/mobile/ [accessed 11/08/17].
17. Mitchell ARJ, Le Page P. Living with the handheld ECG. BMJ Innovations 2015;1:46–48. https://doi.org/10.1136/bmjinnov-2014-000029
18. Gregoski MJ, Mueller M, Vertegal A et al. Development and validation of a smartphone heart rate acquisition application for health promotion and wellness telehealth applications. Int J Telemed App 2012;2012:696324. https://doi.org/10.1155/2012/696324
19. Lau JK, Lowres N, Neubeck L et al. iPhone ECG application for community screening to detect silent atrial fibrillation: a novel technology to prevent stroke. Int J Cardiol 2013;165:193–4. https://doi.org/10.1016/j.ijcard.2013.01.220
20. National Institute for Health and Care Excellence. AliveCor heart monitor and AliveECG app (Kardia Mobile) for detecting atrial fibrillation. NICE advice MIB35. London: NICE, 2015. Available from: https://www.nice.org.uk/advice/mib35/chapter/technology-overview
21. Giada F, Gulizia M, Francese M et al. Recurrent unexplained palpitations (RUP) study comparison of implantable loop recorder versus conventional diagnostic strategy. J Am Coll Cardiol 2007;49:1951–6. https://doi.org/10.1016/j.jacc.2007.02.036
22. StopAfib.org. Out of Sync: The State of Afib in America. Available at: https://www.stopafib.org/newsitem.cfm/NEWSID/159/afib%20doubles%20the%20risk%20of%20death/atrial%20fibrillation [accessed July 2017].
