Rhythm disturbances in healthy subjects undergoing Holter recording are well described. The purpose of this study has been to determine the frequency of rhythm disturbances, in particular of multi-focal atrial rhythm, on the 12-lead ECG of patients complaining of palpitation presenting to their GP.
There were 500 electrocardiograms (ECGs) studied. Rhythms were categorised as supraventricular rhythm disturbances, ventricular rhythm disturbances, multi-focal atrial rhythm, sinus arrhythmia and sinus rhythm. Multi-focal atrial rhythm was diagnosed either if there were a minimum of two complexes of each of three or more distinct P-wave shapes, none of which were obvious atrial ectopics, or if an ectopic atrial rhythm morphed into an ectopic atrial rhythm from another atrial focus.
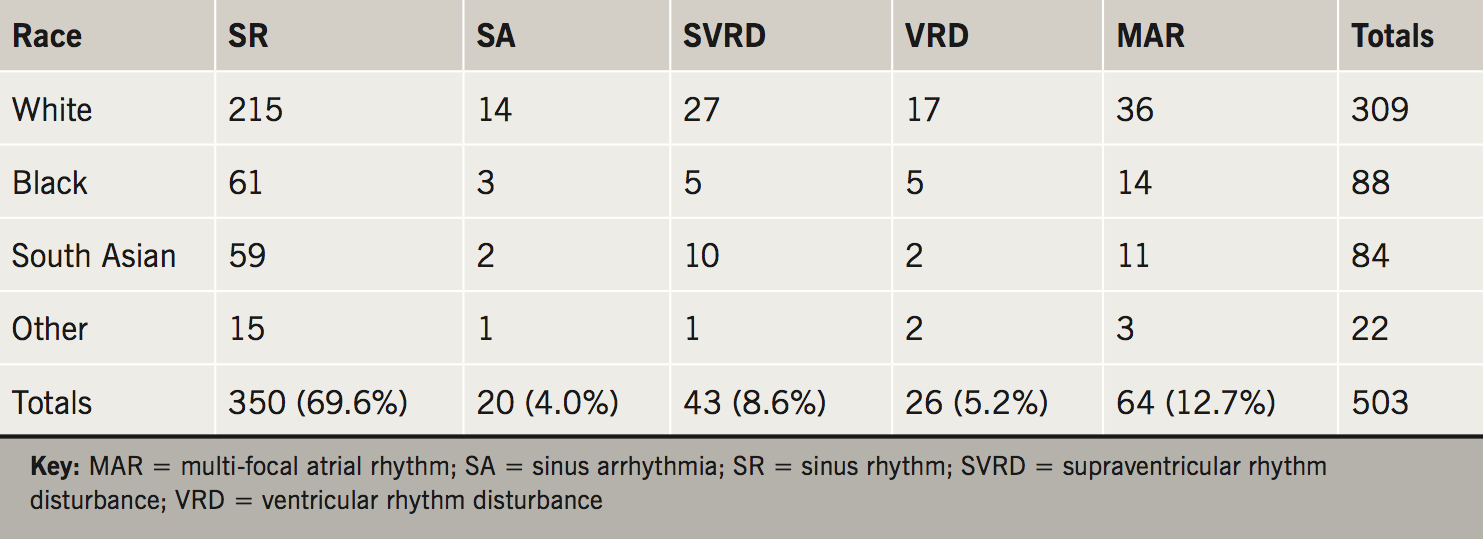
Supraventricular rhythm disturbances (8.6%) were more common than ventricular rhythm disturbances (5.2%). Multi-focal atrial rhythm was found in 12.7% of ECGs and sinus arrhythmia in 4.0%. The relative frequency of the rhythms varied significantly with age, but not by gender or by ethnicity.
In conclusion, a quarter of the subjects with palpitation had a rhythm disturbance on a 10-second 12-lead ECG. Multi-focal atrial rhythm should be considered as a potential cause of palpitation.
Introduction
A 24-hour Holter recording is not a way of reassuring a subject that he/she has no rhythm disturbance, as the vast majority of such recordings show some disturbance of rhythm.1-7 Among the frequently occurring rhythm disturbances on Holter recordings we have noticed is multi-focal atrial rhythm. Multi-focal atrial tachycardia is a well-recognised rhythm disturbance in patients with acute exacerbations of chronic lung disease.8-9 Multi-focal atrial rhythm or ‘wandering atrial pacemaker’ is a less well-defined entity. The rhythm is characterised by a change of atrial focus and may be accompanied by a change in heart rate. When the change in atrial focus is accompanied by a change in heart rate of 20 beats per minute, even for a few beats, the subject may notice it and experience it as palpitation. The purpose of this study has been to determine the frequency of rhythm disturbances, in particular of multi-focal atrial rhythm, on the 12-lead electrocardiogram (ECG) of patients complaining of palpitation presenting to their GP.
Materials and methods
Subjects older than 19 years referred by their GP to the Hammersmith Hospital ECG department for a direct-access 12-lead ECG with a diagnosis of palpitation were studied. A bespoke database recorded every subject referred to the ECG department for an investigation. Subject data included name, date of birth, gender, ethnicity, source of referral and the GP’s diagnosis. Computer interpretation of the ECG was performed by GE-Marquette 12SL v235 ECG interpretation software. The majority of the ECGs that were recorded were stored on floppy disc by the cardiographer or clinical physiologist recording the ECG. Each ECG that had been stored on floppy disc, together with its measurements and its diagnostic statements, was extracted and stored in a Microsoft Access database using bespoke software. The cardiac infarction injury score (CIIS)10 was calculated for each subject to assess the risk of cardiovascular disease in the population. The ECG files were paired with their patient data and merged using date of birth, date of ECG recording and the first four letters of the surname. Between April 2002 and May 2006, 705 adults with a diagnosis of palpitation were referred by their GP to the hospital’s ECG department for a 12-lead ECG. Of these 705 ECGs, 500 were stored on floppy disc and available for visual analysis using a standard 12-lead setup along with 10-second rhythm strips of leads I, II and V1 to V6.
The ECGs were analysed for rhythm disturbances, and divided into five different categories: ECGs displaying a supraventricular rhythm disturbance; ECGs displaying a ventricular rhythm disturbance; ECGs displaying multi-focal atrial rhythm; ECGs displaying sinus arrhythmia and ECGs displaying solely sinus rhythm. Sinus rhythm was diagnosed if the P-wave shape was consistent, the frontal plane P-wave axis was between 15 and 75 degrees, the P–R interval constant and the maximum variation in R–R interval was less than 20%. Sinus arrhythmia was diagnosed if the R–R interval varied cyclically, the maximum variation in R–R interval was more than 20%, the P-wave shape was consistent or changed in time with the variation in R–R interval, the frontal plane P-wave axis was between 15 and 75 degrees and the P–R interval constant. Supraventricular rhythm disturbance included sinus rhythm with atrial or junctional ectopics, atrial fibrillation and atrial flutter. It also included ectopic atrial rhythm in which the P-wave shape was consistent, the frontal plane P-wave axis was outside the range from 15 and 75 degrees and the P–R interval constant. Ventricular rhythm disturbance included sinus rhythm with ventricular ectopics. Multi-focal atrial rhythm was diagnosed either if there were a minimum of two complexes of each of three or more distinct P-wave shapes, none of which were obvious atrial ectopics, or if an ectopic atrial rhythm morphed into an ectopic atrial rhythm from another atrial focus. MAH read all 500 ECGs. PJB read those ECGs that MAH thought were or might be multi-focal atrial rhythm.

Frequency tables of the different rhythm disturbances stratified by age, gender and ethnicity were created. Due to the number of different ethnicities, three main groups were developed: ‘White’, ‘Black’ and ‘Middle-Eastern/South Asian’. Ethnicities that did not apply to these groups or had fewer than 20 subjects were designated ‘Other’. The Pearson’s Chi-squared test of independence was used to identify any significant differences in numbers between different population strata using version 3.2.3 of the R statistical package.
Results
Table 1 shows the rhythms of all of the 500 subjects, the majority of whom showed sinus rhythm. Table 2 shows the five rhythms stratified by age. Sinus arrhythmia, supraventricular rhythm disturbances and multi-focal atrial rhythm were less common in those over the age of 39 than those up to the age of 39, while ventricular rhythm disturbances were more common in those over 39. Analysis comparing the age distributions 20–39 and over 39 showed a Chi-square value of 35.6 with four degrees of freedom (p<0.0001).
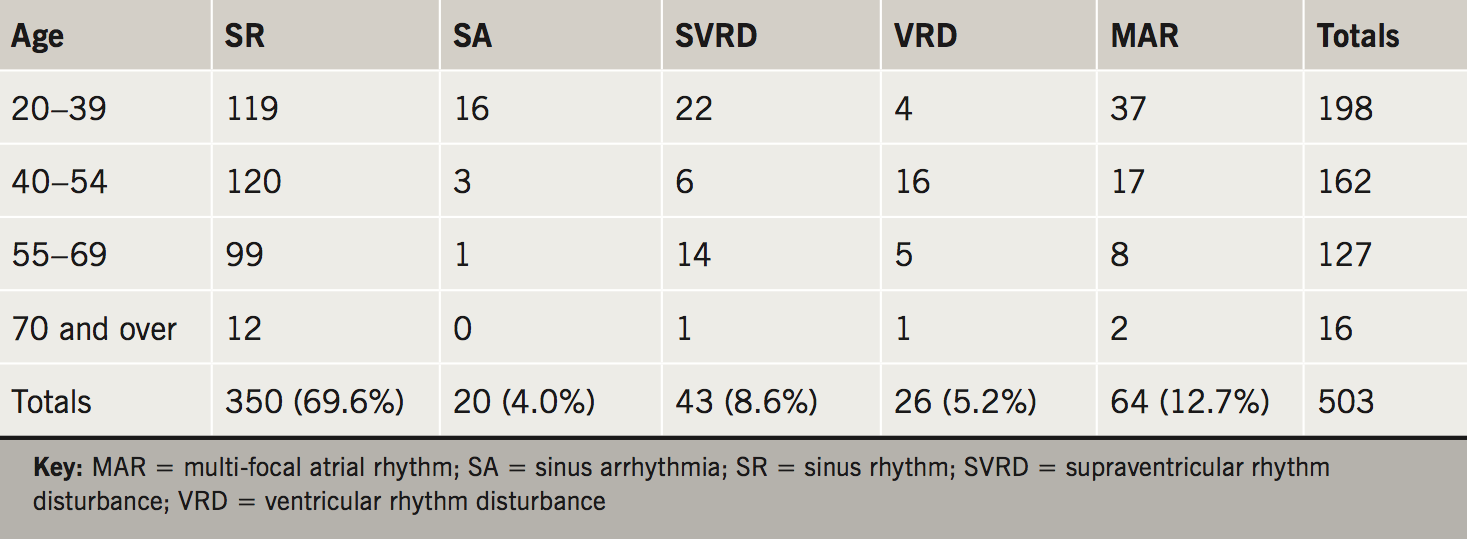
Table 3 shows the five rhythms stratified by gender. The population included roughly twice as many females as males. Analysis comparing the two gender distributions showed a Chi-square value of 3.0 with four degrees of freedom (p=0.55).
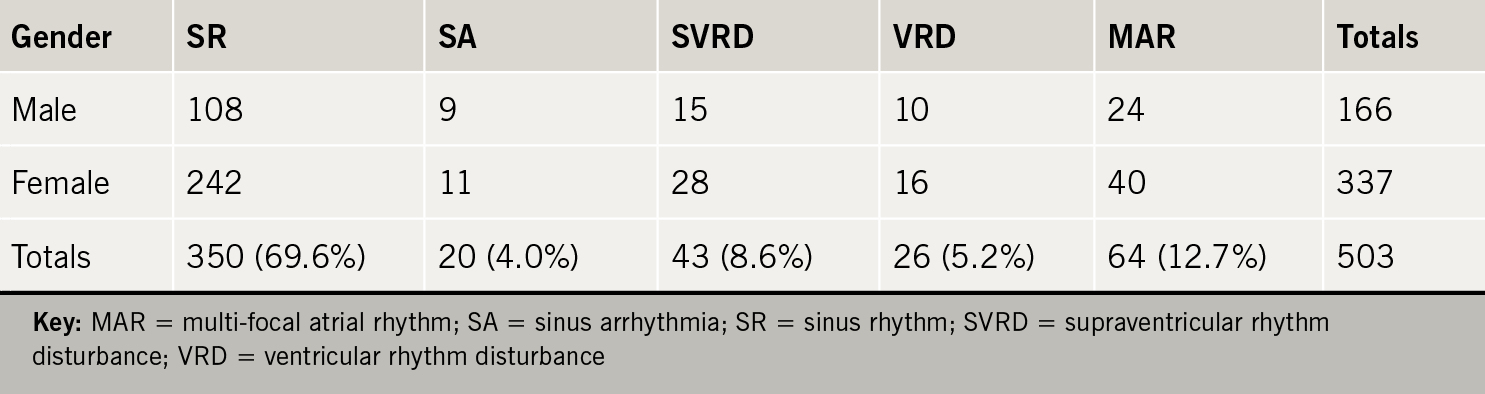
Table 4 shows the five rhythms stratified by ethnicity. Analysis comparing the Whites’ distribution with that of the remainder showed a Chi-square value of 1.6 with four degrees of freedom (p=0.82).
The computer-interpreted diagnostic statements of the 500 ECGs included 21 with a possible myocardial infarction, 10 with suspected myocardial ischaemia, nine with left ventricular hypertrophy and nine with an intra-ventricular conduction defect. The mean of the cardiac injury infarction score was –1.42 (standard deviation [SD] 7.63). The score ranges from –25 to +40 with healthy subjects having values below zero.
Discussion
This study has looked at rhythm disturbances among subjects complaining of palpitation to their GP in a West London community. Palpitation is a common presenting complaint. The subject may have felt ‘an extra beat’ or ‘a missed beat’ or ‘a run of beats’ or may have felt that the heart was beating particularly hard. There are many known triggers of palpitation including caffeine, alcohol, smoking tobacco, anxiety and drugs, both recreational and therapeutic.11-17 For instance, a healthy person, who on a night out consumes an excess of alcohol, may have a ‘hangover’ the following day and at the same time notice ‘missed beats’ or ‘runs of beats’. Although a 10-second 12-lead ECG cannot be definitive as to whether or not the subject has a rhythm disturbance, a 24-hour Holter recording is not a way of reassuring a subject that he/she has no rhythm disturbance, as the vast majority of such recordings show some disturbance of rhythm.1-7 Therefore, requesting a 24-hour Holter recording may not be appropriate if the clinician seeks to reassure the patient. In fact, it was the unpublished observations of individual clinical physiologists in the ECG department that between 50 and 90% of Holter recordings show a marked change in P-wave shape together with a change in R–R interval in the absence of movement artefact, which stimulated this study of multi-focal atrial rhythm on the 12-lead ECG. The multi-focal atrial rhythm usually occurs at night, so the patient does not notice it, but Holter diaries sometimes indicate that the patient noticed a sudden change of heart rate, particularly if the change is of the order of 20 beats per minute even for a few seconds. However, few instances of multi-focal atrial rhythm result in such a rate change.
The availability of ECGs for this analysis depended on the person recording the ECG storing that ECG on floppy disc. Only 70% were stored on floppy disc, so any prevalence estimate is at best an approximation. The measurements of cardiac infarction injury score (CIIS) suggest that the ECGs were recorded from a sample of the general population. Richardson et al.18 recommended that a cardiac damage score should be calculated as part of all computerised ECG interpretations. They found that CIIS outperformed the other ECG classifications determining prognosis that they studied. Bourdillon,19 while validating a method for the heart rate correction of QT interval, found that the CIIS values of Afro-Caribbeans were lower, and those of South Asians were higher, than other ethnic groups in West London. The mean and standard deviations of the CIIS measurements in that study were similar to those in this study.
The results indicate that sinus arrhythmia, supraventricular rhythm disturbances and multi-focal atrial rhythm all decrease with age while ventricular rhythm disturbances increase with age. On the other hand, there is no significant difference in the distributions of the five rhythm disturbances when stratified by gender or when stratified by ethnicity, although there were twice as many females as males in the population studied.
Previous literature has implied the existence of multi-focal atrial rhythm. Brody et al.20 attempted to improve the low-frequency signal-to-noise ratio of P-waves by signal averaging but discovered that no single P-wave morphology existed for a normal subject. Boineau et al.21 demonstrated the presence of competing atrial pacemakers by mapping electrical signals using a net of electrodes on the epicardium of subjects undergoing surgery for pre-excitation. They illustrated two patients, both of whom showed two atrial foci about 40 mm apart.
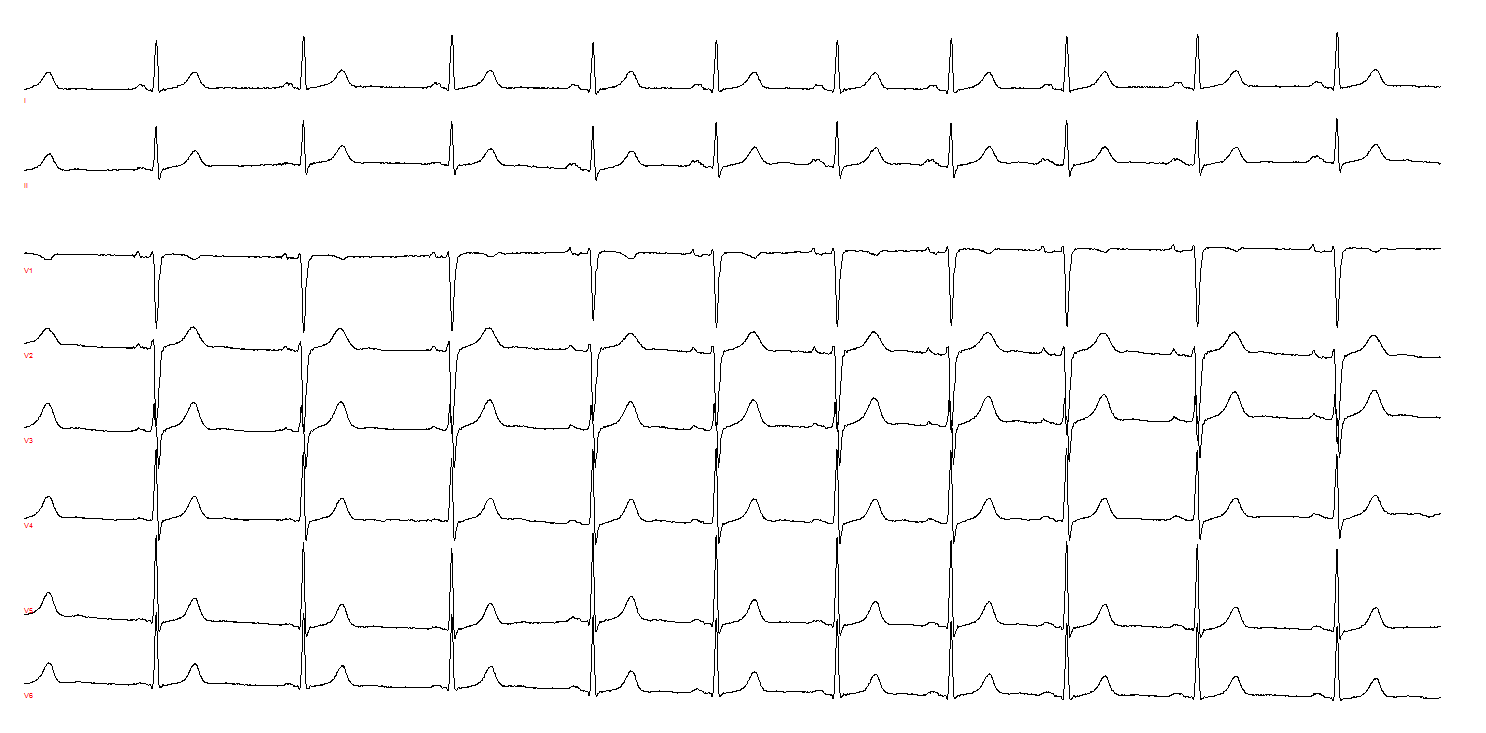
In an attempt to define multi-focal atrial rhythm for the 12-lead ECG, we have diagnosed it either when there was a minimum of two complexes of each of three or more distinct P-wave shapes, none of which were obvious atrial ectopics, or when an ectopic atrial rhythm morphed into an ectopic atrial rhythm from another atrial focus. Changes in P-wave shape indicate a critical difference between multi-focal atrial rhythm and sinus arrhythmia. Sinus arrhythmia does not present with marked P-wave changes, as the heart rate variation is caused by nervous influence on the pacemaker, whereas multi-focal atrial rhythm involves a shift in pacemaker location. The changes in P-wave morphology, therefore, cannot be explained by sinus arrhythmia. Some examples of multi-focal atrial rhythm are shown in figures 1, 2 and 3.
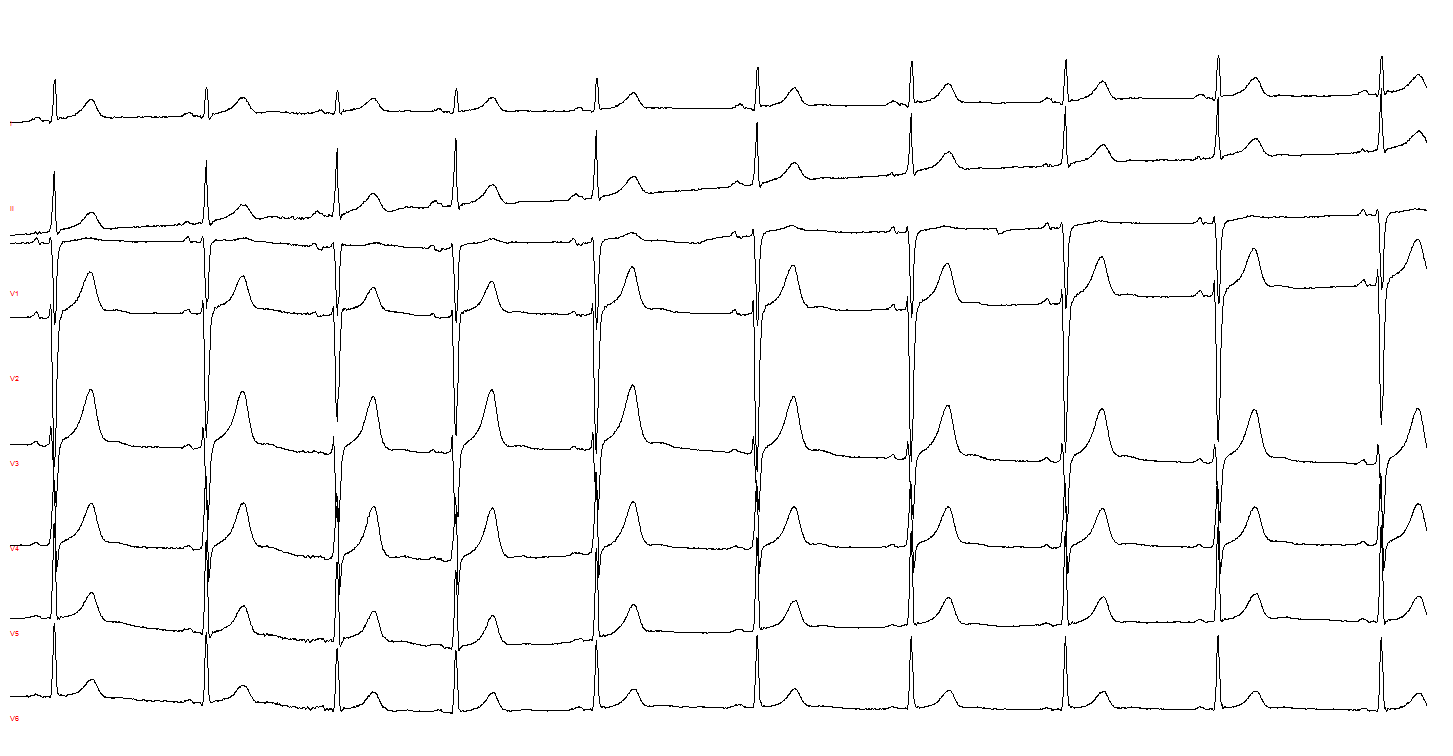

Multi-focal atrial rhythm appears to be a benign rhythm disturbance which is not noticed most of the time. However, if the heart rate changes by more than 20 beats per minute when the atrial focus changes, this may well be noticed, and provides a potential cause of anxiety. Reassuring a subject that multi-focal atrial rhythm is a benign cause of a noticeable rate change may be sufficient to allay any anxiety. It can be argued that as multi-focal atrial rhythm is often labelled as sinus arrhythmia, any anxiety a subject might have will be allayed anyway so the differentiation is unimportant. However, until it has been shown that multi-focal atrial rhythm has no prognostic significance, such an argument is premature. The mechanism of sinus arrhythmia is better understood than that of multi-focal atrial rhythm. Differences in mechanisms may well mean different relationships with other rhythm disturbances, so that proper investigation of the prognostic value of multi-focal atrial rhythm will require wider recognition of the entity. Perhaps more importantly, another implication of the study is that attempts to predict the onset of atrial fibrillation using high-frequency filtering and signal-averaging of P-waves22,23 should only be undertaken if there are no visible changes in the corresponding ‘unfiltered’ P-waves.
This audit has identified four main types of rhythm change in a community setting: supraventricular, ventricular, sinus arrhythmia and multi-focal atrial rhythm. A quarter of the patients complaining of palpitation presenting to their GP had a rhythm disturbance on a 10-second 12-lead ECG. All rhythms, other than ventricular rhythm disturbances, were more common in younger subjects. Multi-focal atrial rhythm was the most common rhythm disturbance seen. The presence of a rhythm disturbance on a 12-lead ECG does not prove that a person’s symptoms are due to the rhythm disturbance, but this study highlights that rhythm disturbances are commonplace. Similarly, the absence of a rhythm disturbance on a 12-lead ECG does not exclude the possibility that the patient has rhythm disturbances.
This study has proposed a definition for multi-focal atrial rhythm and has estimated its prevalence in a population of people complaining of palpitation.
Key messages
- A quarter of the patients complaining of palpitation presenting to their GP had a rhythm disturbance on a 10-second 12-lead electrocardiogram (ECG)
- All rhythms, other than ventricular rhythm disturbances, were more common in younger subjects
- Multi-focal atrial rhythm was the most common rhythm disturbance seen.
Acknowledgements
The storing on floppy disc of ECGs recorded for clinical purposes by the cardiographers and clinical physiologists of the ECG Department at Hammersmith Hospital is much appreciated.
Conflict of interest
None declared.
References
1. Brodsky M, Wu D, Denes P, Kanakis C, Rosen K. Arrhythmias documented by 24 hour continuous electrocardiographic monitoring in 50 male medical students without apparent heart disease. Am J Cardiol 1977;39:390–5. https://doi.org/10.1016/S0002-9149(77)80094-5
2. Chow G, Marine J, Fleg J. Epidemiology of arrhythmias and conduction disorders in older adults. Clin Geriatr Med 2012;28:539–53. https://doi.org/10.1016/j.cger.2012.07.003
3. Fleg J, Kennedy H. Cardiac arrhythmias in a healthy elderly population: detection by 24-hour ambulatory electrocardiography. Chest 1982;81:302–07. https://doi.org/10.1378/chest.81.3.302
4. Folarin V, Fitzsimmons P, Kruyer W. Holter monitor findings in asymptomatic male military aviators without structural heart disease. Aviat Space Environ Med 2001;72:836–8.
5. Larsen B, Kumarathurai P, Nielsen O, Sajadieh A. The circadian variation of premature atrial contractions. Europace 2016;18:1573–80. https://doi.org/10.1016/j.jacc.2015.05.018
6. Manolio T, Furberg C, Rautaharju P et al. Cardiac arrhythmias on 24-h ambulatory electrocardiography in older women and men: the Cardiovascular Health Study. J Am Coll Cardiol 1994;23:916–25. https://doi.org/10.1016/0735-1097(94)90638-6
7. Rossi A. Twenty-four hour electrocardiographic study in the active very elderly. Cardiology 1987;74:159–66. https://doi.org/10.1159/000174192
8. Kastor J. Multifocal atrial tachycardia. N Engl J Med 1990;322:1713–17. https://doi.org/10.1056/NEJM199006143222405
9. Scher D, Arsura E. Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment. Am Heart J 1989;118:574–80. https://doi.org/10.1016/0002-8703(89)90275-5
10. Rautaharju PM, Warren JW, Jain U, Wolf HK, Nielsen CL. Cardiac infarction injury score: an electrocardiographic coding scheme for ischemic heart disease. Circulation 1981;64:249–56. https://doi.org/10.1161/01.CIR.64.2.249
11. Buckley U, Shivkumar K. Stress-induced cardiac arrhythmias: the heart–brain interaction. Trends Cardiovasc Med 2016;26:78–80. https://doi.org/10.1016/j.tcm.2015.05.001
12. D’Allesandro A, Boeckelmann I, Hammwhoner M, Goette A. Nicotine, cigarette smoking and cardiac arrhythmia: an overview. Eur J Prev Cardiol 2012;19:297–305. https://doi.org/10.1177/1741826711411738
13. Greenspon A, Stang J, Lewis R, Schaal S. Provocation of ventricular tachycardia after consumption of alcohol. N Engl J Med 1979;301:1050. https://doi.org/10.1056/NEJM197911083011906
14. Jayaprasan N, Francis J. Atrial fibrillation and hyperthyroidism. Indian Pacing Electrophysiol J 2005;5:305–11. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1431605/
15. Johnson S, Domino E. Some cardiovascular effects of marijuana smoking in normal volunteers. Clin Pharmacol Ther 1971;12:762–8. https://doi.org/10.1002/cpt1971125762
16. Podrid P. Can antiarrhythmic drugs cause arrhythmia? J Clin Pharmacol 1984;24:313–19. https://doi.org/10.1002/j.1552-4604.1984.tb01840.x
17. Shirlow M, Mathers C. A study of caffeine consumption and symptoms: indigestion, palpitations, tremor, headache and insomnia. Int J Epidemiol 1985;14:239–48. https://doi.org/10.1093/ije/14.2.239
18. Richardson K, Engel G, Yamazaki T, Chun S, Froelicher VF. Electrocardiographic damage scores and cardiovascular mortality. Am Heart J 2005;149:458–653. https://doi.org/10.1016/j.ahj.2004.06.025
19. Bourdillon PJ. Not another formula for heart rate correction of QT interval. Ann Noninvasive Electrocardiol 2009;14:80–5. https://doi.org/10.1111/j.1542-474X.2008.00277.x
20. Brody DA, Woolsey MD, Arzbaecher RC. Application of computer techniques in the detection and analysis of spontaneous P-wave variations. Circulation 1967;36:359–71. https://doi.org/10.1161/01.CIR.36.3.359
21. Boineau JP, Canavan TE, Schuessler RB, Can ME, Corr PB, Cox JL. Demonstration of a widely distributed atrial pacemaker complex in the human heart. Circulation 1988;77:1221–37. https://doi.org/10.1161/01.CIR.77.6.1221
22. Blanche C, Tran N, Rigamonti F, Burri H, Zimmermann M. Value of P-wave signal averaging to predict atrial fibrillation recurrences after pulmonary vein isolation. EP Europace 2013;15:198–204. https://doi.org/10.1093/europace/eus251
23. Darbar DI, Jahangir A, Hammill SC, Gersh BJ. P wave signal-averaged electrocardiography to identify risk for atrial fibrillation. Pacing Clin Electrophysiol 2002;25:1447–53. https://doi.org/10.1046/j.1460-9592.2002.01447.x

