We provide the details of three cases utilising intravascular lithotripsy, a novel approach to percutaneous coronary intervention (PCI).
Case 1 – off-label use
A 57-year-old man was referred to the chest pain clinic for further investigation with complaints of progressive dyspnoea on minimal exertion, consistent with New York Heart Association (NYHA) class 3 symptoms. His past medical history included hypertension, hypercholesterolaemia, ischaemic heart disease (ST-elevation myocardial infarction in 2003 requiring percutaneous coronary intervention [PCI] to the distal right coronary artery [RCA]) and a high body mass index (BMI). On examination his vital signs were normal and there were no significant clinical findings. He underwent an electrocardiogram (ECG), routine blood tests, and a Bruce protocol exercise stress test (EST). His ECG showed sinus rhythm at a rate of 77 bpm with ventricular ectopy. His EST was positive for increasing ventricular ectopy, breathlessness and minor ST depression.
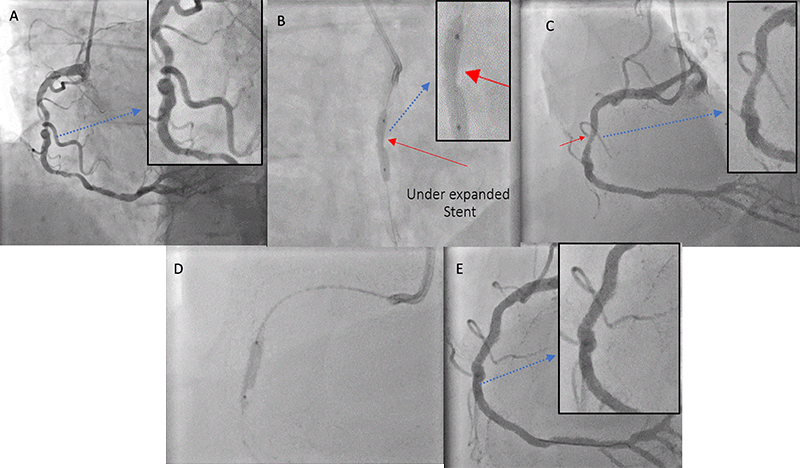
Coronary angiography was performed electively (figure 1) and showed a right dominant system with 90% mid-vessel left anterior descending artery (LAD) disease, non-obstructive plaque in the circumflex, and 70–80% RCA mid-vessel and distal-vessel disease (figure 1A). The vessels were heavily calcified. The patient was admitted and referred for multi-vessel PCI, but the option of coronary artery bypass graft (CABG) was also discussed. Stents were successfully deployed to the LAD and distal RCA immediately before the previous distal RCA stent, which was not significantly re-stenosed since treatment in 2003. There was acceptable stent expansion in the LAD, however, due to significant concentric calcification and tortuosity of the mid-RCA, the mid-vessel stent was suboptimally deployed (figure 1B), despite extensive pre-dilation with a 3 mm non-compliant balloon to high pressure (figure 1C). Attempts were made to deliver a cutting balloon, but this proved impossible due to the combination of tortuosity and calcification (figure 1C). The non-compliant balloon was taken again and inflated to 18 atmospheres in attempts to sufficiently prepare the lesion, and although it appeared expanded on angiography, once the stent was subsequently deployed, there had been a clear failure to sufficiently prepare the lesion. Stent deformation and under-expansion was readily identified at this point (figure 1C). Initially, post-dilation with a 3.0 NC balloon to 20 atmospheres for multiple inflations was attempted. Subsequent to this, a double-layer 3 mm (OPN) balloon was initially deployed at 30 atmospheres, and then 35 atmospheres. Further upsizing of OPN balloons was not performed as there were concerns that the risk of rupture was potentially high. A decision was made to stop, and arrange for ShockwaveTM lithotripsy the following morning. The second procedure involved introducing a 3 mm Shockwave lithotripsy balloon to four atmospheres deploying acoustic energy in 10 pulses before inflating to six atmospheres for three treatment cycles (figure 1D). This generated an estimated equivalent energy to 50 atmospheres of pressure in a safe, controlled manner. The procedure resulted in successful stent expansion and significant luminal gain (figure 1E). The lithotripsy procedure time was 15 minutes. The patient was discharged home the following day and remained clinically well.
Case 2 – off-label use
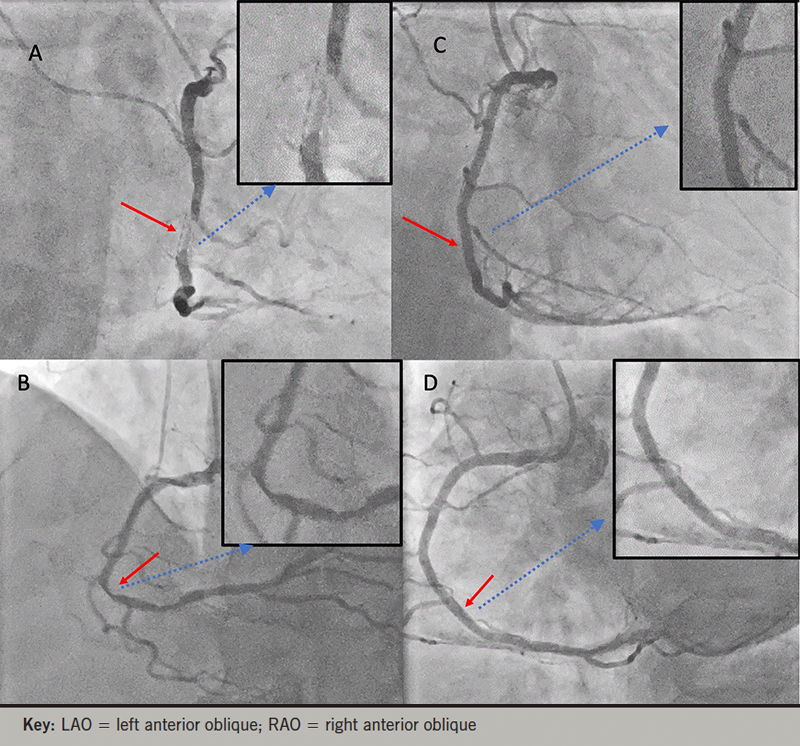
A 70-year-old man presented with a 20-year history of exertional angina that had significantly progressed over the two weeks prior to presentation. He had a history of bare-metal stent deployment in his RCA in 1999 and was told that he had stent failure within one year, which was not amenable to a further stent. As he had single-vessel disease, he was managed medically. His angiogram revealed a grossly under-deployed bare-metal stent with a subtotal occlusion (figures 2A and 2B). This was treated with a 3.5 mm Shockwave balloon resulting in full expansion of the old under-deployed stent, followed by repeat PCI with an everolimus stent with an excellent angiographic result (figures 2C and 2D). Surprisingly, despite chronic ischaemic symptoms, he had gross ST-elevation upon wiring of his RCA, with complete symptomatic remission following PCI and return to exercise after 20 years of a sedentary lifestyle.
Case 3 – on-label use
An 82-year-old man presented with recurrent episodes of prolonged rest angina and angina on minimal exertion. His background included atrial fibrillation, hypertension, hyperlipidaemia, type 2 diabetes, metastatic prostate adenocarcinoma, and a recent pulmonary embolus. Despite long-acting oral nitrates, maximum beta blocker doses and ranolazine, the patient continued to have angina. Angiography showed severe calcific three-vessel coronary disease including diffuse circumferential RCA calcification with sequential subtotal occlusions (figure 3A), significant ramus intermediate disease, and a diffusely calcified LAD. His left ventricular function was normal. He was discussed at a multi-disciplinary conference, but due to his comorbidities, he was declined for CABG. We elected, therefore, to treat his right coronary and ramus intermediate disease with PCI (figure 3).
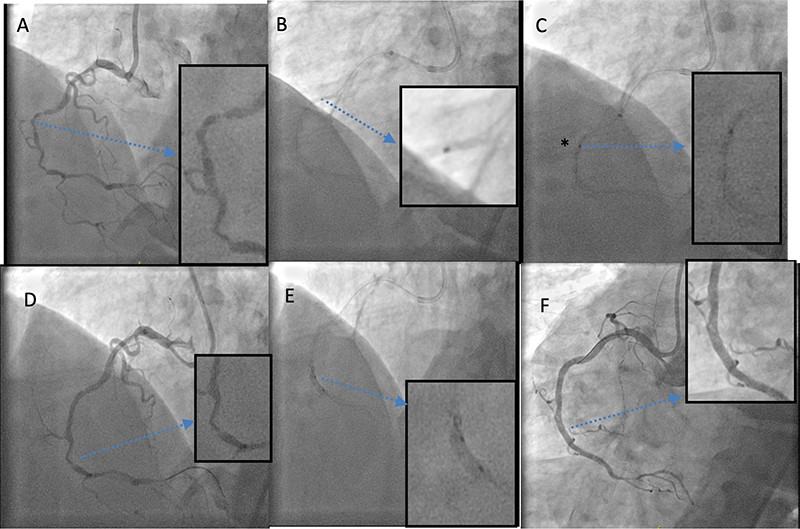
Due to severe peripheral arterial disease, radial access was used. Guide support was problematic, requiring buddy guidewire and guideliner catheter use for back-up support. Wiring the RCA proved difficult due to calcification and excessive tortuosity and frictional forces. Eventually, using a Corsair microcatheter and a Fielder XTA 0.014 guidewire, the distal vessel was accessed. Using a guideliner for support, the calcified disease in the RCA was sequentially pre-dilated with a 1.5, 2.0, and 2.5 mm non-compliant balloon at up to 20 atmospheres. Despite this, there was a resistant waist (figure 3C) on the balloons throughout the treated segment. Eventually, the segment of disease was sequentially treated from the distal vessel back to the proximal segment using a Shockwave IVL 2.5/12 mm balloon with 10 treatments for a total lithotripsy time of 10 minutes. Fluoroscopy demonstrated complete balloon expansion after IVL therapy (figure 3E). The RCA was then stented from distal to proximal with four overlapped drug-eluting stents; 2.5/24 mm, 3.0/36 mm, 3.5/26 mm, and a 3.5/14 mm, all post-dilated with a 3.5/20 mm non-compliant balloon at 20 atmospheres with an excellent angiographic result.
Conflicts of interest
None declared.
Funding
None.
Patient consent
The patients were made aware of the novel approach and written consent was obtained prior to the procedure. Informed consent was also obtained for this article to be written so that its success could be shared, and the technique implemented in other cases in the hopes of achieving similar favourable outcomes.
Editors’ note
Please see the Intervention article for a review of the available literature on the use of IVL.
