After two years of virtual meetings, the Cardiorenal Forum’s recent 17th Annual Scientific Meeting (ASM) was able to return to a face-to-face event with delegates enjoying the opportunity to network, hear and discuss presentations in person again. The meeting was held at the King’s Fund, London, on 7th October 2022. Karin Pola and Sarah Birkhoelzer report some of its highlights.
What’s new in transplantation
Are kidney donors worse off?

The meeting was opened by Dr Anna Price (Queen Elizabeth University Hospital, Birmingham) who addressed the long-term cardiovascular effects of unilateral nephrectomy in living kidney donors.1 Previous studies have shown a significant prevalence of cardiovascular morbidity and mortality in patients with chronic kidney disease (CKD),2,3 but the effects of reduced renal function in living kidney donors has been unexplored until now.
A recent study by Price et al. demonstrated that living kidney donors had a reduction in estimated glomerular filtration rate (eGFR) from 95 to 67 ml/min/1.73m2 during a five-year follow-up, but that there was no change in blood pressure or left ventricular mass or volumes after five years compared to baseline values. Although kidney donors have a reduction in eGFR during long-term follow-up, the study showed no long-term adverse changes in cardiovascular structure or function.
Should LVAD become destination rather than bridge therapy?
The number of heart transplantations in the UK has increased over the past 10 years, from around 200 to 250 transplantations per year.4 Mechanical circulatory support is offered to candidates on the waiting list for heart transplantation; the two-year survival rate of patients with a left ventricular assist device (LVAD) has risen to 85%.5 Could LVAD also be considered as a destination therapy?
Dr Jayan Parameshwar (Royal Papworth Hospital NHS Foundation Trust, Cambridge) presented recent advancements made in the field, and highlighted the main remaining obstacles. Firstly, the challenges to manage expectations of patients and their families, but also the medical professionals. Secondly, limitations in funding for long-term follow-up and for associated care providers. Thirdly, attracting and retaining the skills of the surgical team. In the end, it comes down to priorities. How much does the quality of life and life expectancy of patients with LVAD need to increase to be considered valuable enough to be offered as a destination therapy?

Diabetes, obesity and cardiovascular disease
The right drug for the right patients
Metformin is widely used as a first-line medication for patients with type 2 diabetes. With an increasing number of drug options, the question is: what drug is right for which patient? Professor Cliff Bailey (Aston University, Birmingham), translated complex guidelines into simplified recommendations.6–8 The key is to define the contributing comorbidities of the patient and the subsequent primary goal of therapy. Is it to manage glucose levels, weight, or long-term cardiovascular morbidities and cardiorenal diseases? For second-line pharmacotherapy, consider cardiorenal risks independently of glycated haemoglobin (HbA1c), and add an SGLT-2 inhibitor or GLP-1 receptor agonists if the patient has a high-risk profile. Then consider an additional glucose-lowering drug, such as tirzepatide, insulin, sulfonylureas, thiazolidinediones, or a DPP-4 inhibitor, and a weight-management programme.
Bariatric surgery to prevent cardiorenal disease
Lifestyle plays an important role in the management of type 2 diabetes. Dr Safwaan Adam (The Christie NHS Foundation Hospital, Manchester) addressed the relationship between obesity and microvascular disease, and whether subsequent weight loss with calory restriction or bariatric surgery can reduce cardiovascular risks.
Studies have shown that obesity independently increases the risk of CKD, nephropathy, and neuropathy,9–10 but few studies have investigated the long-term implications of weight loss. Different approaches of weight loss have been studied, such as calorie restriction, medical weight management and bariatric surgery, but the end points are often crude, and the effects are multimodal. Although the evidence is not extensive for the long-term effects of weight loss on microvascular disease, multimodal risk factor reduction is key in managing patients with diabetes. Weight loss with calorie restriction or bariatric surgery seems to either directly or indirectly benefit patients, but the main issue is the difficulty for patients to lose weight and maintain a healthier lifestyle. The challenge remains how to invite patients to discuss their weight and how to train medical professionals in giving appropriate and effective advice. One approach Dr Adam highlighted is the 20-20-20 rule to aid weight reduction: advise patients to reduce meal size by 20%, to take small bites no larger than a 20 pence coin, and to chew each bite for 20 seconds.
CKD and iron deficiency: complex problem, simple solution?
Iron deficiency is common in the general population and has a significant impact on the overall physical wellbeing and quality of life, particularly in patients with heart failure and CKD.11–13 Repletion of iron in patients with heart failure and iron deficiency has been demonstrated to improve exercise capacity and quality of life.14 Dr Sharlene Greenwood (UK Kidney Association and King’s College Hospital, London) presented a randomised, controlled trial soon to be published, studying patients with CKD and iron deficiency but without anaemia, investigating the effects of iron repletion (ferric carboxymaltose) on physical capacity, quality-of-life, and skeletal muscle metabolism. In a study population of 75 participants, 38 were randomised to intravenous iron repletion and 37 to placebo. At three-months follow-up, there was no statistically significant difference from baseline in six-minutes walking test or renal function between the groups. However, a small sample size, short follow-up and an imbalance in baseline characteristics makes it difficult to draw solid conclusions as to whether iron repletion in CKD is beneficial for patients.
Professor Jonathan Barratt (University of Leicester) presented an overview of potential targets for treatment of anaemia. Several factors contribute to anaemia, including inflammation, erythropoietin (EPO) and iron deficiency, decreased oxygen sensing, uraemic toxins, blood loss from the gastrointestinal tract, and increased red blood cell haemolysis. Hypoxia-inducible factor prolyl hydroxylase inhibitors (HIF-PHi) have recently been released on the market as an oral tablet drug. This group of drugs mimics the body’s response to hypoxia and drives erythropoiesis and iron metabolism. HIF-PHi are effective in achieving and maintaining target haemoglobin levels in adult patients with CKD and anaemia, and clinical data generally support a favourable risk-benefit profile for cardiovascular disease and general safety.15 HIF-PHi have recently been approved by the National Institute for Health and Care Excellence (NICE) for patients with CKD stage 3 to 5 with no iron deficiency and in those who are not on dialysis. HIF-Phi agents include daprodustat, roxadustat and vadadustat.
Heart failure and diabetes – insights from imaging

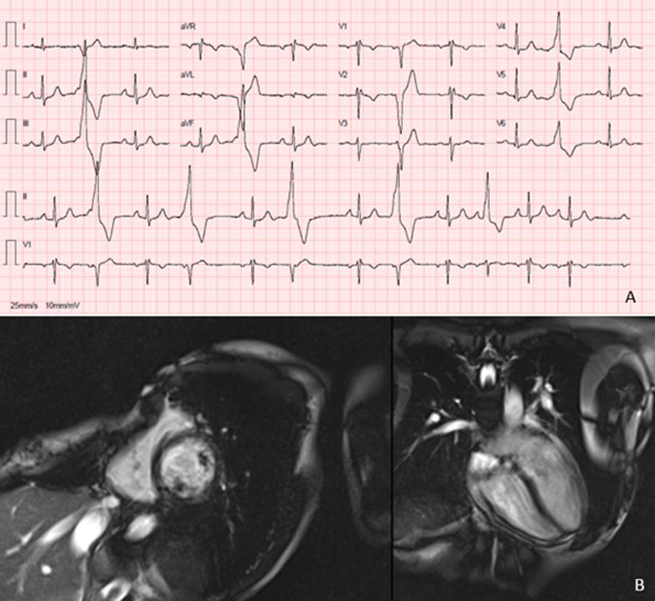
Type 2 diabetes confers up to a two-fold increased risk for developing heart failure,17 but the underlying pathological mechanisms start long before the patient develops any symptoms. Professor Gerry McCann (University of Leicester) conducts research on early signs of heart failure in patients with type 2 diabetes. Diabetes is associated with smaller cardiac volumes and increased ventricular mass. Advanced cardiac magnetic resonance imaging can detect subclinical structural changes, such as fibrosis and inflammation, in patients with type 2 diabetes.18
Professor McCann’s research group has investigated the cardiovascular effects of exercise or a meal replacement diet of around 800 calories per day in patients with type 2 diabetes, compared to standard care.19 Results showed differences in the fibro-inflammatory and cardiovascular structure and function profile in patients with type 2 diabetes without symptoms of cardiovascular disease compared to healthy controls. A 12-week diet with meal replacement powder in patients with type 2 diabetes is associated with improved fibro-inflammatory markers and cardiovascular structure. There was no independent association between exercise and improved cardiac function. However, overall lifestyle improvements should always be encouraged for a general risk reduction.
Cardiorenal clinical trials update
Dr Geraint Morton (Portsmouth Hospitals University NHS Trust) presented his update of the latest clinical trials looking at the most common treatments for patients with cardiovascular disease summarised in table 1.
Table 1. Cardiology trials update summary
| Trial name | Take-home message |
| REVIVED20 | In patients with left ventricular systolic dysfunction and stable coronary artery disease, revascularisation with percutaneous coronary intervention is not better than medical therapy |
| SYMPLICITY HTN-321 | No convincing long-term or event-driven data on the effects of renal denervation. It should therefore be limited to the UK registry |
| TIME22 | Antihypertensive medication can be taken at any time of the day, as timing has no influence on cardiovascular outcomes |
| SGLT2 inhibitors in heart failure23 | SGLT2 inhibitors have a positive effect in patients with heart failure regardless of ejection fraction |
| Key: REVIVED = Study of Efficacy and Safety of Percutaneous Coronary Intervention to Improve Survival in Heart Failure; SGLT2 = sodium-glucose co-transporter 2; TIME = Treatment in Morning versus Evening | |
An update in renal trials was given by Dr David Lappin (Galway University Hospitals), who highlighted three beneficial drugs for patients with CKD (see table 2).
Table 2. Renal trials update summary
| Trial name | Take-home message |
| CLICK24 | In patients with advanced CKD and poorly controlled hypertension, the addition of chlorthalidone to other antihypertensive medications improved blood pressure after 12 weeks compared to placebo. |
| TESTING25 | Among patients with IgA nephropathy at high risk of progression, treatment with oral methylprednisolone for six to nine months reduced the risk of the composite outcome of kidney function decline, kidney failure, or death due to kidney disease. |
| FIDELITY pooled analysis26 | Finerenone reduced the risk of clinically relevant cardiovascular and kidney outcomes in patients with CKD and type 2 diabetes. |
| Key: CKD = chronic kidney disease; CLICK = Chlorthalidone for Hypertension in Advanced Kidney Disease; FIDELITY = Fineronone in Chronic Kidney Disease and Type 2 Diabetes; IgA = immunoglobulin A; TESTING = The Therapeutic Evaluation of Steroids in IgA Nephropathy Global | |
£1 in every £77 of the NHS budget is spent on CKD
The prevention of kidney disease has decreased in the last five years, and end-stage CKD has increased in the UK.27 Professor Smeeta Sinha (Salford Royal NHS Trust and University of Manchester) presented the results of a joint working project with AstraZeneca to create a multimorbidity multi-disciplinary team (MDT) clinic. Patients with type 2 diabetes and CKD have a 4.5 times increased 10-year mortality compared to patients with type 2 diabetes without kidney disease.28 To prevent the progression to CKD, The London Kidney Network has developed an action plan for adults with type 2 diabetes and CKD (see table 3). There should be a continuity of healthcare for patients, where there is a link between primary care, multi-specialty MDT and multimorbidity MDT clinics.
Table 3. Three key actions within three months (London Kidney Network, September 2022)
| ACTION 1 (month 1) |
| Maximum intensity RAS/ RAAS blockade |
| First, ensure the patient is on a statin, unless contraindicated. Start ACE inhibitor or ARB and titrate dose to maximum tolerated dose within one month. |
| ACTION 2 (month 2) |
| Initiate SGLT2 inhibitor |
| Counsel the patient on the risks of diabetic ketoacidosis (which may be euglycaemic), sick day rules, and the risk of urinary tract infections. Consider adjusting sulfonylureas or insulin where eGFR is >45 ml/min and HbA1c is <59 mmol/mol to mitigate the risk of hypoglycaemia |
| ACTION 3 (month 3) |
| Initiate further blood pressure agent to target 140/90 mmHg |
| If urine albumin-creatinine ratio is >70 mg/mmol, the blood pressure target is 120–129/80 mmHg. If blood pressure remains above target, initiate second-line blood pressure agents as per NICE guidance |
| Key: ACE = angiotensin-converting enzyme; ARB = angiotensin receptor II blocker; eGFR = estimated glomerular filtration rate; NICE = National Institute of Health and Care Excellence; RAS/RAAS = renin-angiotensin system/renin-angiotensin-aldosterone system; SGLT2 = sodium-glucose co-transporter 2 |
Clinical cases in cardiorenal disease
The meeting ended with the popular clinical cases session.
Anticoagulation in advanced renal disease
Miss Kathrine Parker (Manchester University NHS Foundation Trust) presented clinical cases of patients with renal disease and atrial fibrillation, and the challenges of anticoagulation in patients with CKD, dialysis and post-renal transplantation. The conclusion was that evidence is sparse and that clinical decisions need to be made in collaboration with the patient and based on the individual risk profile.
Dyslipidaemia in high-risk patients
Dr Wei Yang (Imperial College London) addressed new treatment options used in the clinic for dyslipidaemia in high-risk patients. Treatment options for patients with dyslipidaemia despite statins or with contraindications to statins, are as follows:
- Alirocumab and evolocumab – monoclonal antibodies which inhibit PCSK9
- Inclisiran, a small interfering RNA agent that limits production of PCSK9, increasing uptake of low-density lipoprotein (LDL) cholesterol and thereby lowering levels in the blood.
- Bempedoic acid, an adenosine triphosphare citrate lyase (ACL) inhibitor which inhibits cholesterol synthesis in the liver, thereby lowering LDL-cholesterol
Finerenone in CKD
With all the recent cardiovascular outcome trials, how do we chip away at residual risk in CKD and diabetic kidney disease?” Dr Kieran McCafferty (Barts Health NHS Trust, London) asked delegates. Presenting results from the FIDELIO (Finerenone in patients with CKD and type II diabetes with and without heart failure) study, he showed that finerenone had improved clinically relevant cardiorenal outcomes in patients with CKD and type II diabetes irrespective of SGLT2 inhibitor use at baseline. The study has led to a renewed interest in the use of mineralocorticoid receptor antagonists (MRAs) in cardiorenal disease.
Acknowledgements
The Cardiorenal Forum would like to thank the following companies for their funding and support of this independent meeting: A Menarini Farmaceutica UK Ltd, Astellas Pharma Ltd, AstraZeneca UK Ltd, Bayer plc, CSL Vifor, GSK, Novo Nordisk Ltd, and Sanofi.
Diary date
The 18th Annual Scientific Meeting of the Cardiorenal Forum will take place in London on Friday 6th October 2023.
Further information
To find out more about the Cardiorenal Forum and its activites, visit https://cardiorenalforum.com/
Karin Pola
PhD student
Cardiac MR Group, Department of Clinical Sciences, Lund University, Sweden
Sarah Birkhoelzer
Clinical Research Fellow
Oxford Centre for Clinical Magnetic Resonance Research, University of Oxford
References
1. Price AM, Moody WE, Stoll VM, et al. Cardiovascular effects of unilateral nephrectomy in living kidney donors at 5 years. Hypertension 2021;77:1273–84. https://doi.org/10.1161/HYPERTENSIONAHA.120.15398
2. Moody WE, Ferro CJ, Edwards NC, et al. Cardiovascular effects of unilateral nephrectomy in living kidney donors. Hypertension 2016;67:368–77. https://doi.org/10.1161/HYPERTENSIONAHA.115.06608
3. Altmann U, Böger CA, Farkas S, et al. Effects of reduced kidney function because of living kidney donation on left ventricular mass. Hypertension 2017;69:297–303. https://doi.org/10.1161/HYPERTENSIONAHA.116.08175
4. NHS Blood and Transplant. Annual report on cardiothoracic transplantation. 2022. https://nhsbtdbe.blob.core.windows.net/umbraco-assets-corp/27816/nhsbt-annual-report-on-cardiothoracic-organ-transplantation-202122.pdf (last accessed 10 January 2023)
5. Mehra MR, Uriel N, Naka Y, et al. A fully magnetically levitated left ventricular assist device — final report. N Engl J Med 2019;380:1618–27. https://doi.org/10.1056/NEJMoa1900486
6. Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2022;65:1925–66. https://doi.org/10.1007/s00125-022-05787-2
7. American Diabetes Association Professional Practice Committee. 9. Pharmacologic approaches to glycemic treatment: Standards of medical care in diabetes—2022. Diabetes Care 2022;45(Suppl 1):S125–S143. https://doi.org/10.2337/dc22-S009
8. Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 2020;41:255–323. https://doi.org/10.1093/eurheartj/ehz486
9. Gray N, Picone G, Sloan F, Yashkin A. The relationship between BMI and onset of diabetes mellitus and its complications. South Med J 2015;108:29–36. https://doi.org/10.14423/SMJ.000000000000021
10. Gelber RP, Kurth T, Kausz AT, et al. Association between body mass index and CKD in apparently healthy men. Am J Kidney Dis 2005;46:871–80. https://doi.org/10.1053/j.ajkd.2005.08.015
11. Okonko DO, Mandal AKJ, Missouris CG, Poole-Wilson PA. Disordered iron homeostasis in chronic heart failure: Prevalence, predictors, and relation to anemia, exercise capacity, and survival. J Am Coll Cardiol 2011;58:1241–51. https://doi.org/10.1016/j.jacc.2011.04.040
12. Klip IT, Comin-Colet J, Voors AA, et al. Iron deficiency in chronic heart failure: An international pooled analysis. Am Heart J 2013;165:575–82. https://doi.org/10.1016/j.ahj.2013.01.017
13. Jankowska EA, Rozentryt P, Witkowska A, et al. Iron deficiency: An ominous sign in patients with systolic chronic heart failure. Eur Heart J 2010;31:1872–80. https://doi.org/10.1093/eurheartj/ehq158
14. Anker SD, Comin Colet J, Filippatos G, et al. Ferric carboxymaltose in patients with heart failure and iron deficiency. N Engl J Med 2009;361:2436–48. https://doi.org/10.1056/NEJMoa0908355
15. Haase VH. Hypoxia-inducible factor–prolyl hydroxylase inhibitors in the treatment of anemia of chronic kidney disease. Kidney Int Suppl 2021;11:8–25. https://doi.org/10.1016/j.kisu.2020.12.002
16. Ortiz A, Germain DP, Desnick RJ, et al. Fabry disease revisited: Management and treatment recommendations for adult patients. Mol Genet Metab 2018;123:416–27. https://doi.org/10.1016/j.ymgme.2018.02.014
17. Gulsin G, Athithan L, McCann GP. Diabetic cardiomyopathy: prevalence, determinants and potential treatments. Ther Adv Endocrinol Metab 2019;10:2042018819834869. https://doi.org/10.1177/2042018819834869
18. Jensen MT, Fung K, Aung N, et al. Changes in cardiac morphology and function in individuals with diabetes mellitus: The UK Biobank Cardiovascular Magnetic Resonance Substudy. Circ Cardiovasc Imaging 2019;12:1–10. https://doi.org/10.1161/CIRCIMAGING.119.009476
19. Gulsin GS, Swarbrick DJ, Athithan L, et al. Effects of low-energy diet or exercise on cardiovascular function in working-age adults with type 2 diabetes: A prospective, randomized, open-label, blinded end point trial. Diabetes Care 2020;43:1300–10. https://doi.org/10.2337/dc20-0129
20. Perera D, Clayton T, O’Kane PD, et al. Percutaneous revascularization for ischemic left ventricular dysfunction. N Engl J Med 2022;387:1351–60. https://doi.org/10.1056/NEJMoa2206606
21. Bhatt DL, Vaduganathan M, Kandzari DE, et al. Long-term outcomes after catheter-based renal artery denervation for resistant hypertension: final follow-up of the randomised SYMPLICITY HTN-3 Trial. Lancet 2022;400:1405–16. https://doi.org/10.1016/S0140-6736(22)01787-1
22. Mackenzie IS, Rogers A, Poulter NR, et al. Cardiovascular outcomes in adults with hypertension with evening versus morning dosing of usual antihypertensives in the UK (TIME study): a prospective, randomised, open-label, blinded-endpoint clinical trial. Lancet 2022;400:1417–25. https://doi.org/10.1016/S0140-6736(22)01786-X
23. Vaduganathan M, Docherty KF, Claggett BL, et al. SGLT-2 inhibitors in patients with heart failure: a comprehensive meta-analysis of five randomised controlled trials. Lancet 2022;400:757–67. https://doi.org/10.1016/S0140-6736(22)01429-5
24. Agarwal R, Sinha AD, Cramer AE, et al. Chlorthalidone for hypertension in advanced chronic kidney disease. N Engl J Med 2021;385:2507–19. https://doi.org/10.1056/NEJMoa2110730
25. Lv J, Wong MG, Hladunewich MA, et al. Effect of oral methylprednisolone on decline in kidney function or kidney failure in patients with IgA nephropathy: The TESTING randomized clinical trial. JAMA 2022;327:1888–98. https://doi.org/10.1001/jama.2022.5368
26. Agarwal R, Filippatos G, Pitt B, et al. Cardiovascular and kidney outcomes with finerenone in patients with type 2 diabetes and chronic kidney disease: The FIDELITY pooled analysis. Eur Heart J 2022;43:474–84. https://doi.org/10.1093/eurheartj/ehab777
27. The Renal Association. UK Renal Registry 23rd Annual Report. 2019. https://ukkidney.org/sites/renal.org/files/23rd_UKRR_ANNUAL_REPORT.pdf (last accessed 10 January 2023)
28. Afkarian M, Sachs MC, Kestenbaum B, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol 2013;24:302–8. https://doi.org/10.1681/ASN.2012070718