This case describes the discovery and subsequent attempts at removal of a migrated venous stent.
Case report


A 38-year-old man with pelvic chondro-sarcoma diagnosed in 1999 had a right femoral venous stent for extrinsic compression by the tumour in June 2004. Two months later, computed tomography (CT) scan of the chest with a view for chemotherapy unexpectedly showed the venous stent within the right heart.
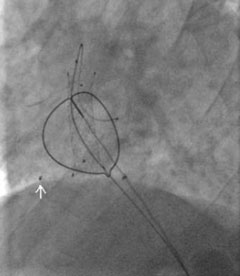
Though asymptomatic, he was referred for catheter retrieval of the venous stent, as potential serious complications include thrombus formation, pulmonary embolism, sepsis, endocarditis, myocardial perforation and cardiac tamponade. Transthoracic echocardiogram showed the stent was lodged across the tricuspid valve (figures 1 and 2).
The procedure was performed with vascular and cardiothoracic surgical backup. A 14-French sheath was used via the left femoral vein. The stent was retracted down to the left iliac vein after eventually catheterising the stent under fluoroscopy with a large loop snare (figures 3 and 4), following an initially unsuccessful attempt with a Dormier catheter. One strut was splayed in the right atrium remote from the stent prior to the start (arrow), and was not retrieved, as it was certainly endothelialised.
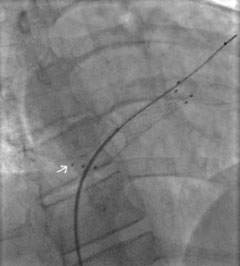
The stent size could not allow withdrawal without surgery and it was decided to deploy it in the left iliac vein with a 9/40 mm balloon. Thrombus was noted locally and extracted, followed by anticoagulation with heparin for 48 hours and planned warfarin for three months. Post-procedure transthoracic echocardiogram was normal.
Discussion
Venous stents can migrate into cardiac cavities or the pulmonary artery. The diameter of the stent must exceed that of the designated vein to prevent migration as respiratory movements induce great variability in the diameter of the vein.
Conflict of interest
None declared.
