The multi-disciplinary approach provides a forum for peer review of angiographic data. We aimed to examine the outcomes of our multi-disciplinary team (MDT) meetings in a two-year follow-up study. A total of 191 patients were studied and mainly divided into groups offering conservative therapy, percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABG). CABG was offered to 60% of patients with left main stem disease, 45% with proximal left anterior descending artery lesions and 59% with triple-vessel disease. PCI was offered to 40% of patients with single-vessel disease. One death was observed in the PCI group at two years, substantially lower than deaths in other groups. Overall mortality at two years was 6.4%. PCI conferred a significantly higher need for repeat revascularisation compared with surgery (odds ratio 5.71, p=0.005). Our results resonate with outcomes of published trial data comparing CABG and PCI.
Introduction
Approximately 77,000 percutaneous coronary interventions (PCI) and 25,000 coronary artery bypass grafting (CABG) surgeries are performed in the UK every year.1 Revascularisation strategies may vary between institutions, medical attendants, and based upon patients’ preferences. Anatomic considerations are also important, and lesion location, severity and extent may influence decisions on revascularisation.
The multi-disciplinary team (MDT) approach provides clinicians with an opportunity for peer consultations and provides ‘best-practice’ treatment strategies after review of angiographic recordings. Our weekly MDT meetings are attended by four cardiologists, a visiting cardiac surgeon, junior doctors, cardiac nurse specialists and radiographers. To date, no published data exist on cardiology–cardiothoracic MDT meetings.
We aimed to examine the characteristics of patients reviewed in the MDT meetings, the revascularisation strategies and a two-year follow-up on outcomes.
Methods
A retrospective survey was conducted on all patients discussed at our local cardiology–cardiothoracic MDT meetings between April and October 2006.
Patients were divided into four groups; those offered conservative medical therapy (group 1), PCI (group 2) or CABG (group 3). Those who required further review pending more investigations were analysed separately (group 4).
Data were collected from the MDT-meeting register, angiogram reports, clinic letters and the hospital patient database. Statistical analyses were done using Fisher’s exact test. All analyses were conducted according to ‘intention to treat’. This study received approval from the local ethics committee.
Results
In the seven-month period, 209 patients were discussed in the MDT meetings. This represented 42% of all patients who had angiograms within the study period. Of these, 191 (92%) were patients with coronary artery disease (CAD). Only stable patients were included in these meetings.
This study focuses on those with CAD. Sixty patients (31%) were offered conservative therapy, 42 (22%) PCI and 70 (37%) CABG. Nineteen (10%) patients required further investigations (group 4).
Demographics
The male to female ratio was 3:1, with a median age of 67 years. Caucasians formed 63% of the study population.
The most common risk factors were hypertension (24%), background ischaemic heart disease (23%) and hypercholesterolaemia (20%). Co-morbidities that may affect revascularisation decisions and outcomes were also studied. A total of 21% of patients had severe left ventricular (LV) impairment (ejection fraction <30%) and 32% had poor mobility. Other co-morbidities, like chronic obstructive airway disease and malignancy, were not present in our study population.
Patients with multiple co-morbidities were less likely to receive interventional therapy. None of those with severe LV impairment received angioplasty, one received CABG and seven were treated conservatively.
Angiographic findings
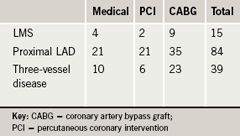
Coronary stenoses of 50% or more were considered significant. Fifteen patients (9%) had left main stem (LMS) lesions, 84 (49%) had proximal left anterior descending artery (LAD) involvement and 39 (23%) had three-vessel disease (3vD) (table 1). Sixty per cent of patients with LMS lesions, 45% with proximal LAD stenosis and 59% with 3vD were offered CABG.
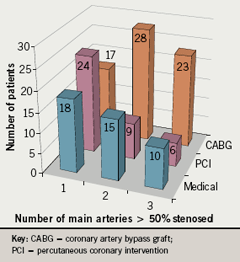
Figure 1 illustrates the allocation of patients to treatments based on number of main arteries involved (LAD, left circumflex artery [LCX] and right coronary artery [RCA]). Forty per cent (n=24) of patients with single-vessel disease were treated with PCI. Those with two or more diseased vessels tended to be selected for CABG (n=51).
Outcomes
No deaths were seen in the PCI group at six months. The number of deaths at two years was considerably smaller in the PCI group (n=1, 2.4%) compared with those treated conservatively (n=6, 10%) or with CABG (n=4, 5.7%). A higher proportion of patients (n=7, 37%) from group 4 died within two years.
Six patients in group 1 required revascularisation within two years; four required PCI and two had CABG. Ten (24%) PCI recipients required further revascularisation within two years compared with only three (4.3%) CABG recipients (odds ratio [OR] 5.71, p=0.005).
Discussion
To date, there are no National Institute for Health and Clinical Excellence (NICE) guidelines on revascularisation. The Scottish Intercollegiate Guidelines Network (SIGN) recommends CABG for patients with significant LMS and 3vD, but PCI to those with single- or double-vessel disease if optimal medical therapy fails.2
Randomised Intervention Trial of Unstable Angina (RITA 3) examined the long-term outcomes of interventional versus conservative strategy in non-ST-elevation myocardial infarction (NSTEMI).3 In the five-year follow-up, death or non-fatal myocardial infarction (MI) were less prevalent with intervention than without (16.6% vs. 20.0%, p=0.044).
The Synergy between PCI with Taxus and Cardiac Surgery (SYNTAX trial) examined 1,800 randomised patients with previously untreated LMS and 3vD. Major adverse cardiac and cerebrovascular events (MACCE) were more prevalent with PCI than with CABG (17.8% vs. 12.4%, p=0.002) due to a higher rate in repeat revascularisation (13.5% vs. 5.9%, p<0.001).4 Removing repeat revascularisation from the outcome, MACCE rates did not differ between subgroups (7.6% for PCI and 7.7% for CABG, p=0.98). A similar trend is seen in our study. A further 1,275 patients were not randomised in SYNTAX but nested in separate PCI and CABG registries due to their suitability for only one of the interventions.
Taking into account anatomic considerations, a New York observational study (n=59,576) found better survival advantage with PCI in those with one-vessel disease and less than 70% stenosis.5 Of those with similar characteristics in our study, no mortality was observed with PCI, but five deaths occurred in those treated otherwise (p>0.05). The observational study also saw a better survival advantage with CABG in those with at least 70% proximal LAD stenosis and 3vD. This difference was not reproduced in our study.
The presence of severe valvular disease may influence decisions in favour of surgical revascularisation; a limitation of this study. Those with anatomically simpler lesions may also receive treatment without prior discussions at the MDT meetings.
Conclusion
Each of the three treatment modalities has its own advantage. CABG is preferred for complex lesions and multiple-vessel disease. Those with single-vessel disease or isolated lesions will receive greater benefit with PCI.
Our revascularisation results guided by MDT meetings concur with published trial data. We concluded that the MDT approach should be the way forward in making good revascularisation decisions.
Acknowledgement
We wish to record our thanks to the Cardiac specialist nurses at Whipps Cross University Hospital.
Conflict of interest
The authors have no competing interests and did not receive funding for this study.
Key messages
- Coronary artery bypass grafting (CABG) was offered mostly to patients with left main stem disease, proximal left anterior descending artery and triple-vessel disease
- Percutaneous coronary intervention (PCI) was offered mostly to those with single-vessel disease
- Mortality is lowest in the PCI group
- A higher rate of repeat revascularisation was observed in the PCI group
References
- British Cardiovascular Intervention Society. British Cardiovascular Intervention Society PCI audit. Available from: http://www.bcis.org.uk/resources/audit [accessed 23 April 2009].
- Scottish Intercollegiate Guidelines Network. Management of stable angina. Edinburgh: SIGN, 2007. Available from: http://www.sign.ac.uk/pdf/qrgchd.pdf [accessed 23 April 2009].
- Fox K, Poole-Wilson P, Clayton TC et al. 5-year outcome of an interventional strategy in non-ST-elevation acute coronary syndrome: the British Heart Foundation RITA 3 randomized trial. Lancet 2005;366:914–20.
- Serruys PW, Morice MC, Kappetein P et al. Percutaneous coronary intervention versus coronary artery bypass grafting for severe coronary artery disease. N Engl J Med 2009;360:961–72.
- Hannan E, Racz M, McCallister B et al. A comparison of three-year survival after coronary artery bypass graft surgery and percutaneous transluminal coronary angioplasty. J Am Coll Cardiol 1999;33:63–72.
