In this new regular series ‘ECGs for the fainthearted’ Dr Heather Wetherell will be interpreting ECGs in a non-threatening and simple way. She hopes this will help keep the art alive in primary care. In the latest article, she looks at abnormal ECGs
In the last few articles in this series, we have considered the methodological approach of working through an electrocardiogram (ECG), shared a few ‘hot tips’ and discovered the importance of actually looking at the ECG rather than relying on the digital interpretation! We have seen examples of how the digital interpretation can be very misleading at best, and totally inaccurate at worst.
Hopefully by now, you know how to simply describe what you see, and from there build up the pieces of information to create a reasonable interpretation.
So this issue, we are going to study an abnormal ECG and work through it. Here we are faced with a typical presentation in general practice – sufficiently vague and non-acute to wonder if the presentation is indeed relevant, or simply incidental to our findings.
Let’s see how we get on.
Case
A delightful 84-year-old man comes to see you in surgery. Among other things, he mentions some chest pains. His symptoms are a bit vague and non-specific. He’s been having them for six years. They don’t sound cardiac, but you know him well, and know that he has a history of ischaemic heart disease (IHD).
He is not a fit man, but on the other hand, he is not clinically unwell today. He seems much the same as usual. Along with his known IHD and chronic kidney disease stage 5 (CKD5), he is also pretty immobile from his osteoarthritis and obesity. He seems a bit breathless today, much the same as usual. You think, “this could be anything….”.
He has a lot of potential problems. You note from his recent annual review blood checks that he has chronic stable anaemia (haemoglobin around 10.5 g/dL for many years) secondary to his CKD. His renal function is poor but stable (estimated glomerular filtration rate [eGFR] is 10–12 ml/min/1.73 m2).
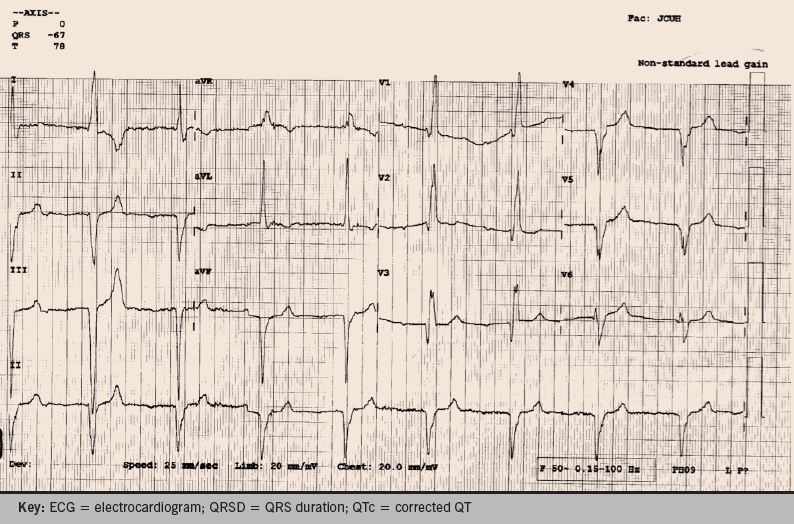
You decide it might be wise to get an ECG while you consider how best to take this forward. The practice nurse pops it back in front of you – figure 1.
Now what should you do? Are you any the wiser?
Let’s look at the ECG methodically and see if it helps. All ECGs can be analysed with a few simple rules. Remember, if in doubt, just describe what you see.
Rate
Comment – what is the rate?
The rate has already been calculated for you at 52 bpm. If not, assuming standard paper speed of 25 mm/s, a quick ready reckoner is as follows:
- For regular rhythms: rate = 300 divided by the number of large squares between two complexes.
- For irregular rhythms: rate = the number of complexes in 30 large squares (i.e. 6 seconds) multiplied by 10.
A rate of 52 bpm, by definition, is a bradycardia (normal rate = 60–100 bpm). So, we already have something to say.
This ECG shows a bradycardic rhythm.
Rhythm
Comment – is this a regular or an irregular rhythm?
It is regular. This is best seen by studying the QRS complexes in long lead II. If there is no rhythm strip on a 12-lead ECG, you may only have three complexes to study and regularity can be very difficult/impossible to determine.
We can now add – this ECG shows a regular, bradycardic, rhythm.
P-waves
Are there any P-waves?
Are they obvious – or perhaps hidden in other waves, or non-existent?
How do they appear? (Morphology? Orientation? Size?)
Do they have a consistent appearance?
Do they have a consistent relationship with the QRS?
We can just see P-waves in the chest leads v1–6, but they are subtle. The poor quality baseline, with interference, makes them barely visible in the limb leads, or in the rhythm strip. (Cheats tip: if you are not sure about seeing complexes – get a repeat ECG with the ‘gain’ increased to magnify the complexes. Indeed, this was necessary in this case – you may have noticed the comment on the top right of the ECG: “non-standard lead gain”).
On this man’s standard ECG, it was not possible to see if there were P-waves or not. If there were no P-waves, then this would be a ventricular escape rhythm, i.e. no atrial activity seen, and the ventricles have helpfully responded by setting up their own pacemaker focus somewhere within them.
Of the few P-waves we can see, their shape is uniformly round. They appear to be upright in v1 but possibly inverted in v2–6.
Those we can see, appear to have a consistent relationship with the following QRS complexes, HOWEVER, the PR-interval is prolonged… The normal PR-interval (start of P-wave to the first deflection of the QRS complex) should be 3–5 small squares (0.11 to 0.20 seconds). In this case, the PR-interval is between 8–9 small squares (>0.32 seconds).
We are building gradually.
This ECG shows a regular, bradycardic rhythm, with a first-degree heart block.
QRS complexes
Now we need to study the QRS complexes. We have already decided they are regular. We cannot really comment on the size, because we now know that the gain has been increased. So, there is no point thinking about left ventricular hypertrophy (LVH) on this ECG.
We can consider their shape. Are they consistent in all leads? What about their orientation? Is there any axis deviation? What is their duration? A normal QRS complex should be no wider than 1.5 to 2.5 small squares (0.06–0.11 seconds).
In a heart with a healthy conduction system, once the impulse passes through the atrioventricular (AV) node, it travels through the bundle of His, and down the left and right bundle branches. As long as there is no delay in this conduction, this gives rise to a narrow QRS complex (less than three small squares).
If, however, after the impulse reaches the bundle of His, there is any delay in the conduction, through either the left or right bundle branch, then the QRS complex will be widened. Left bundle branch block (LBBB) usually gives rise to a wider QRS complex than a right bundle branch block (RBBB). In LBBB, the width of the QRS is >120 ms (i.e. more than three small squares), whereas RBBB is often ≤3 small squares.
- LBBB = left chest leads (I, v5 and v6) show RSR pattern (remember: WiLLiaM).
- RBBB = right chest leads (v1 and v2) show RSR pattern (remember MaRRoW).
If we go back to the ECG we notice that the QRS complexes are slightly broad, with RBBB formation.
We now know that this ECG shows a regular bradycardia, with a first-degree heart block, AND a right bundle branch block.
But, that’s not all….
If you have successfully worked out the cardiac axis, you will also see that there is a left axis deviation. RBBB alone would not normally alter the cardiac axis. Common causes of left axis deviation are:
- LVH
- Inferior myocardial infarction (MI)
- Normal variant in obese, or stocky body habitus.
If we know that none of these situations apply in this man, then we know something else must be going on.
The left bundle branch divides into two – the anterior fascicle and the posterior fascicle. If both fascicles are blocked, then it becomes a full LBBB, but if only one fascicle is blocked, this is known as a ‘hemiblock’ or ‘fascicular’ block. A left anterior hemiblock (left fascicular block), will always cause a left axis deviation.
If you ever see RBBB + left axis deviation, on an ECG, then you almost certainly have a left anterior hemiblock.
So this 84-year-old man has a first-degree heart block, RBBB and left anterior hemiblock.
In fact, he is relying entirely on his small posterior fascicle, of the left bundle branch for ventricular conduction. If that fails him, he’s in trouble. It is still difficult to know how many of his presenting symptoms were relevant to this, but a history of syncope should now be actively sought. Unsurprisingly, an echo revealed severely reduced left ventricular systolic function. He needs a full cardiology assessment and consideration for pacing.
How did you do?
Further information
For GPs interested in progressing their confidence in ECG skills, there is an excellent e-Module available, on which these teachings are based:
http://www.tees.ac.uk/parttime_courses/Health_&_Social_Care/University_Certificate_in_Continuing_Education_ECG_Interpretation_for_General_Practitioners.cfm
And for those of you who are even more e-savvy, don’t forget @ECGclass!
