The extent of the problem: Most people with stable angina, irrespective of treatment, will get symptoms again over a prolonged follow-up period. The ACRE (Appropriateness of Coronary Revascularisation) study, for example, showed that in a consecutive unselected patient series of 1,020 patients, more than 50% treated with percutaneous coronary intervention (PCI) or medical treatment had symptoms at six years.(1)
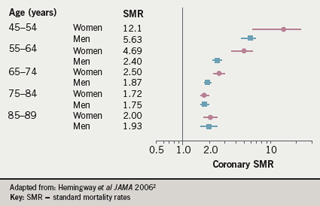
Healthcare professionals may perhaps be motivated more by coronary death rates and acute coronary syndrome events. Primary care registry data from Finland in some 27,000 patients are shown in figure 12. The coronary standardised mortality rates (SMRs) from coronary heart disease in patients with test-positive angina are strongly elevated in the younger age groups; although the SMR declines by the time patients reach their ninth decade, it is still double the rate in the general population.
Interestingly, data from Hemingway3 suggest that there is no evidence of male excess with respect to the prevalence of typical symptoms of angina. This systematic review and meta-analysis looked at 74 population studies in 31 countries across the world: the countries varied dramatically in terms of underlying myocardial infarction (MI) mortality rates, smoking rates and access to healthcare for women. Nevertheless, for the 24,000 patients included, stable angina prevalence showed a small female excess, with a pooled sex ratio of 1.20.
Other data from Hemingway2 also suggest no marked evidence of male excess in physician-diagnosed angina cases. The findings imply that the risk factors for chronic stable coronary disease may be slightly different from the risk factors for acute coronary syndromes, where one would expect to see a marked male excess. They also raise issues about what is appropriate investigation and management in women.
In a study of patients enrolled consecutively without exclusion criteria, the highest probability of death or acute MI was found to occur among people who are appropriate for coronary artery bypass graft (CABG) but who receive only medical management4. There is a large difference in event rates between these patients and rates in those who are appropriate for CABG and who actually receive it. The discrepancy is consistent with the difference that might be expected from randomised trials.
Decision support
The advantage of being able to define each individual patient according to the likely effectiveness of their treatment is that it then becomes possible to measure systematically in all patients whether that treatment is given. This is also a valid approach to the use of investigations, such as angiography. Clinicians may be invited to assess whether angiography should be done on a nine-point scale of appropriateness, for example. An estimate of overall appropriateness can be obtained from epidemiological evidence and clinical judgement, and can then be tested empirically to see whether it is valid.
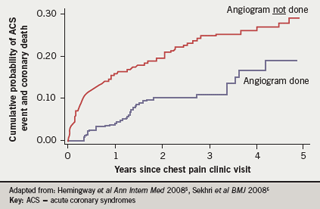
There is some observational evidence that people who are appropriate for angiography but in whom it is not done have a higher coronary event rate than patients appropriate for angiography in whom it is done (figure 2)5,6. We are interested in discovering whether clinicians can be supported to make the right decisions, and to make them systematically. Results from a randomised trial, the Appropriateness of Referral and Investigation in Angina (ARIA) trial7, imply that clinicians (n=300) given patient vignettes make better decisions compared with those using broad clinical guidelines. In this trial, patient-specific ratings, unlike conventional guidelines from the American Heart Association (AHA) and European Society of Cardiology (ESC), had the potential to reduce practice variations and to increase the appropriate use of exercise ECG and angiography.
This observation is now going to be tested in a real patient cluster randomised trial looking at optimising management of angina (OMA). In this trial, 50 chest pain clinics will be randomised to either usual care or to an intervention which includes decision support for angiography as well as risk-based decision support for secondary prevention drugs and behaviour change for smoking cessation and exercise.
At initial presentation many patients do not fulfil the same criteria as patients selected into randomised trials for initiation of many of the classes of agents used for secondary prevention. They are in diagnostic purgatory for some time yet treatment decisions still need to be made.
Looking ahead
There is a role for much better prognosis research, observational studies that understand the progression of people with a pre-existing disease. Myocardial infarction mortality is decreasing rapidly in the general population, but the prevalence of doctor-diagnosed angina in the general population assessed over five waves of Health Survey for England data between 1991 and 2003 in approximately 70,000 patients is not showing any evidence of decline. So, with an ageing population, the absolute number of people living with a diagnosis of angina is increasing.
Conflict of interest statement
None declared.
References
- Griffin SC, Barber JA, Manca A et al. Cost-effectiveness of clinically appropriate decisions on alternative treatments for angina pectoris: prospective observational study. BMJ 2007;334:624-31.
- Hemingway H, McCallum A, Shipley M et al. Incidence and prognostic implications of stable angina pectoris among women and men. JAMA 2006;295:1404-11.
- Hemingway H, Langenberg C, Damant J et al. Prevalence of angina in women versus men: a systematic review and meta-analysis of international variations across 31 countries. Circulation 2008;117:1526-36.
- Hemingway H, Crook AM, Feder G et al. Underuse of coronary revascularization procedures in patients considered appropriate candidates for revascularization. N Engl J Med 2001;344:645-64.
- Hemingway H, Chen R, Junghans C et al. Appropriateness criteria for coronary angiography in angina: reliability and validity. Ann Intern Med 2008;149:221-31.
- Sekhri N, Timmis A, Chen R et al. Inequity of access to investigation and effect on clinical outcomes: prognostic study of coronary angiography for suspected stable angina pectoris. BMJ 2008;336:1058-61.
- Junghans C, Timmis AD, Eldridge S et al. Effect of patient-specific ratings vs conventional guidelines on investigation decisions in angina. Arch Intern Med 2007; 167:195-202.
