Evidence from randomised trials supports percutaneous coronary intervention (PCI) in patients with acute coronary syndromes (ACS): PCI has been shown to improve clinical outcomes and to reduce events. Its role in the broader group of patients with chronic angina and stable coronary artery disease has been less certain, however.
We have known for two decades that PCI improves angina and short-term exercise capacity but we have been unable to answer five key questions. Compared to optimal medical therapy in patients with chronic angina and stable coronary artery disease (CAD), does PCI:
- prolong survival?
- decrease the risk of subsequent myocardial infarction (MI)?
- reduce hospitalisation for unstable angina?
- decrease the need for subsequent surgery?
- improve the quality of life?
Perhaps the most important trial that was never accorded much significance was the Randomised Intervention Treatment of Angina (RITA-2) trial1. It randomised 1,018 patients with stable CAD to either balloon angioplasty or medical therapy (which at this time consisted principally of aspirin, nitrates and beta blockers since it was the pre-statin, pre-ACE-inhibitor, pre-clopidogrel era). Nevertheless, there was a two-fold difference in death and definite MI between the two groups in favour of medical therapy over 2.7 years of follow-up, with very convincing Kaplan-Meier curves (3.3% versus 6.3%).
At the time of Katritsis 2005 meta-analysis, the totality of randomised controlled trial data in patients with stable angina comprised fewer than 3,000 patients2. Meta-analysis of these data showed no significant treatment difference between PCI and conservative therapy with regard to mortality, cardiac death or MI, non-fatal MI or need for subsequent revascularisation.
The COURAGE trial
This then was the background to the COURAGE (Clinical Outcomes Utilising Revascularisation and Aggressive Drug Evaluation) trial3. A total of 1,149 patients were randomised to PCI combined with optimal medical therapy and 1,138 to optimal medical therapy alone. The primary outcome was death from any cause and non-fatal MI during a follow-up period of 2.5 to 7.0 years (median 4.6 years).
The optimal medical therapy used in the study was really robust by contemporary standards: every drug within drug classes that had been shown individually in placebo-controlled studies to be of clinical benefit was employed. Thus, patients received antiplatelet agents, statins, angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers, beta blockers, calcium channel blockers and nitrates, as required. Lifestyle interventions included smoking cessation, exercise programmes, nutrition counselling and weight control. These were applied equally to both arms by protocol and case-managed by nurses. Good control of blood pressure and blood lipids was achieved and maintained throughout the seven years of follow-up.
Although the trial has been criticised for enrolling low-risk patients, in the trial population 34% of patients had diabetes, 71% had dyslipidaemia, 67% had hypertension, 29% were smokers, 39% had prior MI, 26% had prior revascularisation, 70% had multivessel CAD and 68% had left anterior descending (LAD) disease. At baseline, patients had experienced angina for a duration of 26 months, and angina frequency was six or more episodes per week. Eighty-five percent had inducible ischaemia, 67% had multiple reversible perfusion defects on stress myocardial perfusion imaging, and the death/event rate was 4.3% per annum. So this was at least an intermediate-risk group.
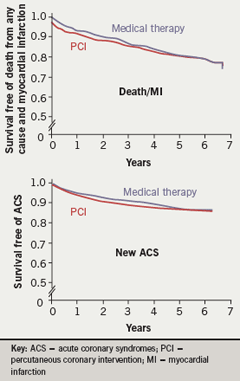
The primary end point in the COURAGE trial, the composite outcome of survival free of death from any cause or MI in the two treatment groups, showed no significant differences at the end of a 4.6-year median follow-up, with a hazard ratio of 1.05 (p=0.62), and if anything with a trend in favour of better clinical outcomes for patients in the optimal medical therapy group in roughly the first two years. The Kaplan-Meier curves are very similar (figure 1): in particular, the mortality rate curves are virtually superimposable over the whole follow-up period. No incremental benefit could be identified for PCI on top of a background of optimal medical therapy for any of these prognostically important end points.
There was an overall crossover rate of 33% from optimal medical therapy to PCI during the seven-year follow-up period. The median time to revascularisation was approximately 11 months and thus, only 16.5% of medically-treated patients crossed over to PCI during this interval. After this time, the crossover rate was only 2.8% per year. Importantly, 67% of patients did not ever require even a first revascularisation procedure after their initial assignment.
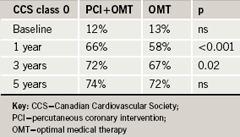
As expected, PCI was superior to optimal medical therapy for the relief of angina using the Canadian Cardiovascular Society (CCS) classification (table 1). At one year and even at three years there was a statistically significant benefit for PCI compared with medical therapy. But the medical therapy group also improved greatly over one year and, with more prolonged follow-up, the differences attenuated and narrowed between the groups.
A recent paper has looked at quality of life4. This employed the Seattle Angina Questionnaire (SAQ), a well validated metric scale, which ranges from 0 to 100, with 0 being very symptomatic and 100 asymptomatic. Patients in both treatment groups were very symptomatic at baseline (score 51 in each group). Within a month, the SAQ score rose from 51 to 62 in the optimal medical therapy group and to 68 in the optimal medical therapy plus PCI group. At one year, the differences between the two groups were statistically significant but numerically small. At two years, the difference between the groups was not statistically significant.
PCI is of benefit in patients with ACS and acute MI but apparently not so in patients with stable CAD because the two conditions have a different pathobiology. Most patients with stable CAD have severe fibrotic and calcified plaques, which are easily detected angiographically, are mostly found on histology to have a very thick fibrous cap, a very small lipid core, and a thick circumferentially calcified artery. These changes cause exertional angina and a positive exercise test. By contrast, in acute coronary syndrome patients with the so-called ‘vulnerable’ plaque, which has a much larger lipid core and a much thinner fibrous cap, plaque rupture is more likely to occur at the shoulder margin, resulting in acute MI, unstable angina and sudden death.
Paradoxically, two thirds to three quarters of MIs occur in the presence of non-flow-limiting stenoses5. Therefore it is progression in non-flow-limiting lesions that causes plaque rupture to occur.
A study evaluating long-term outcome after PCI6 has shown that major cardiac events occur in non-target areas (or non-instrumented vessels) following a successful procedure. In this study, some 1,228 patients implanted with a bare metal stent were followed up for five years. After the first year, the average annual hazard rate was 1.7% for target-lesion events whereas it was 6.3% for non-target-lesion events. About 37% of events emanated from disease progression in native non-flow-limiting stenoses. Thus, a substantial number of cardiac events could be prevented if we knew how to identify them.
What are key opinion leaders saying about PCI versus optimal medical therapy? Holmes and others7 concluded that “in trials of patients with stable coronary artery disease, no reductions in death or MI have been observed, and these limitations of PCI in this clinical setting need to be emphasised.”
The case for optimal medical management
There is much evidence to support optimal medical therapy as the initial approach to stable CAD management. For patients undergoing elective angiography for chronic angina:
- 12 randomised controlled trials (RCTs) in more than 5,200 patients showed no difference in death, MI, stroke or other hard end points between PCI and optimal medical therapy
- an initial course of optimal medical therapy preserves the option for PCI if medical therapy fails (although only 16.5% of COURAGE optimal medical therapy patients crossed over to PCI within one year)
- over a full seven-year follow-up period, two thirds of all optimal medical therapy patients never required even a first PCI procedure
The COURAGE study has given us clarity in management of patients with chronic angina and stable CAD. Whereas PCI offers better angina relief over one to three years and better quality of life over one to two years, optimal medical therapy is a safe and viable option in selected patients who may not be good candidates for PCI (for example, those who are frail, suffer from chronic kidney disease or have multiple co-morbidities). If optimal medical therapy is used as an initial approach, this preserves PCI as a subsequent option for symptomatic/quality of life relief, if needed.
Conflict of interest statement
WEB has received research grants, speakers’ bureau honoraria or has acted as a consultant to Abbott, Bristol Myers Squibb, Gilead Scientific, Merck, Pfizer, and Sanofi-Aventis.
References
- Coronary angioplasty versus medical therapy for angina: the second Randomised Intervention Treatment of Angina (RITA-2) trial. RITA-2 trial participants. Lancet 1997;350:461–8.
- Katritsis DG, Ionnadis JP. Percutaneous coronary intervention versus conservative therapy in nonacute coronary artery disease: a meta-analysis. Circulation 2005;111:2906–12.
- Boden WE, O’Rourke RA, Teo KK et al for the COURAGE Trial Research Group. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007;356:1503–16.
- Weintraub WS, Spertus JA, Kolm P et al. Effect of PCI on quality of life in patients with stable coronary disease. N Engl J Med 2008;359:677–87.
- Falk E, Shah PK, Fuster V. Coronary plaque disruption. Circulation 1995;92: 657–71.
- Cutlip DE, Chhabra AG, Baim DS et al. Beyond restenosis. Five-year clinical outcomes from second-generation coronary stent trials. Circulation 2004;110:226–30.
- Holmes DR, Gersh BJ, Whitlow P et al. Percutaneous coronary intervention for chronic stable angina : a reassessment. JACC Cardiovasc Interv 2008;1:34–43.
