Conducting clinical research is an ambition of many cardiologists and academic clinicians. Over the last decade, the National Health Service (NHS) has indicated that research is a clear priority in improving healthcare for patients. The processes leading to permission to start a clinical trial in the UK are, however, poorly understood, labyrinthine and fraught with difficulty. In this article, we aim to share our knowledge of initiating a clinical trial using a case study, with a focus on the essential documents and the communication required with different organisations.
Introduction
During 2014, one of us (AK) had a four-month research placement in the academic foundation programme. The aim was to create and conduct a clinical trial in heart failure. Although the trial was successful, the success was only achieved through motivation, organisation, good communication and luck. Because of the hurdles now placed between investigator and study, planning between supervisor and trainee started over a year in advance to discuss the idea for the trial, draft the study protocol, and complete all the documents required. The full timeline of events from conception to completion spanned 336 days. The aim of this article is to share the experience and help other clinicians understand the process of obtaining approval to carry out clinical research.
Conducting a clinical trial in the UK is certainly not an easy task (see figure 1). There are numerous points in the development of a study where it may fail: from funding and logistics to ethics committee approval and patient enrolment. In order to obtain approval, an application needs to be made to multiple organisations, each in turn requiring effective communication to prevent delay in a lengthy process.

Although the government has made medical research and innovation a priority of NHS England following publication of the policy paper Creating Change: innovation, health and wealth one year on,1 with the focus on improving the quality, and, particularly, the ease of carrying out research in the UK, the experience of academics and clinicians in applying for approval to conduct clinical research is time-consuming and fraught with difficulties.
Applications and documents
To obtain approval for a clinical trial there are a number of applications and documents required:
- Protocol, Medicines and Healthcare Products Regulatory Agency (MHRA) application
- Research & Ethics Committee (REC) application
- Research & Development (R&D) application
- Site Specific Information (SSI) application
- Summary of Product Characteristics (SmPC)
- Patient information sheet
- Consent form
- Case Report Form (CRF).
Case clinical trial
(EudraCT: 2014-003380-38)
The trial conducted was a randomised, single-blinded, cross-over study involving 31 participants with heart failure at a well-established research site in the UK. The only drug used was oxygen (room air, 28% and 40%), delivered via Venturi, while patients exercised using a cycle ergometer weekly over three visits. The main outcomes were exercise time, and peak metabolic equivalent (MET) and workload reached. Secondary outcomes were heart rate, blood pressure and oxygen saturation during exercise.
We found that increasing fraction of inspired oxygen (FiO2) to 28 or 40% acutely improves exercise capacity in patients with chronic heart failure. Increasing FiO2 also resulted in higher oxygen saturation during exercise. The heart rate during each stage of exercise was lower with FiO2 of 28% with no further drop at 40%. Changing FiO2 had no effect on blood pressure.
The trial was completed in a timely manner without any participants having noticed any ill effects during or following the study.
Relevant bodies
There are a number of relevant bodies in clinical research:
- Integrated Research Application System (IRAS)
- Medicines and Healthcare products Regulatory Agency (MHRA)
- Research and Development (R&D) department of the NHS Trust
- Research and Ethics Committee (REC).
Protocol
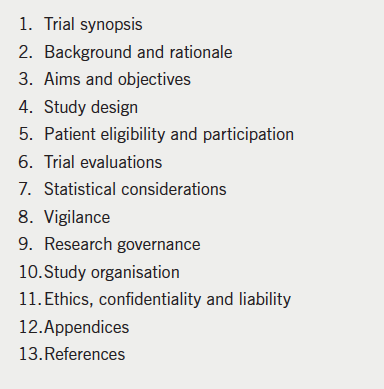
protocol
The protocol is the core document in a clinical trial, and was approximately 25 pages long in the case study (table 1). It focuses on the study objectives, design and safety measures. The protocol requires a full literature review to provide evidence for the study’s relevance. A key aspect of the protocol is safety reporting: it must be stated how and when adverse effects will be reported. Consideration must also be given to where the data will be stored.
The principle of the protocol is that on reading, one is fully aware of the clinical relevance and how to conduct the study. A key feature of the protocol is that it must be readily understandable to the reader in its entirety.
A robust protocol makes the process of applying for approval from the relevant bodies via the Integrated Research Application System (IRAS) system much more straightforward. It is the document that contains most of the information required by the relevant organisations.
In our case study, the protocol took nine major drafts and eight months before being ready for submission. During this time, there were several informal discussions with both R&D and the MHRA, ensuring that modifications to the design could be made at a (relatively) early stage (see figure 2).

Integrated research application system (IRAS)
The IRAS was launched in 2008. It is an online database, which underpins (and purportedly streamlines) the application process for submission to the relevant bodies. It is both free and simple to create an account. The application starts with a number of filter questions to identify the most appropriate application pathway for the investigating team to follow. It is essential to fill out the preliminary section correctly. IRAS receives applications to conduct a wide variety of studies ranging from audits, questionnaire-based research, physiological research, trials involving medicinal products, trials working with human tissue and gene therapy. While there is significant overlap between some of these, specific considerations pertaining to the trial will need to be made. The IRAS filter ensures that only the relevant sections of the total application process are completed by the investigating team.
Once the filter questions are completed, the online application is left open as a project for the investigating team to complete and submit. There is a wealth of documentation and support available on the website, which includes a contacts list page, FAQ and an e-learning module to become more accustomed with using the system.
If there is doubt as to the classification of a trial, it is helpful to discuss the issues with organisations such as the MHRA and local R&D department. These groups are experienced in the development of clinical studies, and will help reduce the risk of an incorrect application being made in an already lengthy process.
Even though the system automatically completes questions which overlap with the demands of other organisations, such as the REC and MHRA, the IRAS application is burdensome. For the case study trial, the application was 46 pages long and had 160 questions to be answered. Once an application to the relevant body is ready for submission, it must be electronically signed by both the principal investigator and representative of the sponsor. An important note is that any change to a data entry point on the application subsequently invalidates the signatures and means the document requires re-signing.
International registry
It is becoming increasingly important to place a clinical trial in an international registry and is expected on submission to the MHRA and R&D. If you are applying for funding, trial registration is regarded as essential. A EudraCT number can be obtained relatively simply, website: https://eudract.ema.europa.eu
Funding
Obtaining external funding for a clinical trial requires a long application process in itself. Funds are needed to pay for the time, equipment, travel and services associated with a clinical trial. Each potential organisation has different requirements and expectations that have to be met. Most of the documentation needed is similar (but not, of course, identical) to that required by the relevant bodies for trial approval.
Our study was internally funded by the Academic Cardiology department, avoiding the need to raise external monies.
Sponsor
A sponsor is required for a clinical trial to take place. It can be an investigator, individual(s) or organisation.
The sponsor takes responsibility for indemnity and liability. The sponsor rarely funds the study; instead conducts a full review of all the documentation during the early phases of the trial. The sponsor also confirms that the relevant documentation has been completed and monitors the study, particularly in regard to safety reporting. In addition, they ensure that good clinical practice is followed throughout.
In our study, the sponsor was the Trust Research & Development department. This was approved following review of the protocol, evaluation of the investigating team (including CVs) and agreement of costings.
Good Clinical Practice (GCP)
The investigators in any clinical study must comply with Good Clinical Practice2 and should, thus, hold valid GCP training certificates. GCP training is helpful in understanding how a clinical trial should be conducted, along with the responsibilities of the relevant bodies and investigating team.
MHRA
All studies involving medicines require authorisation from the MHRA. The MHRA is responsible for the clinical safety of trials and undertakes a thorough review of a study design before approval. An application to the MHRA costs £250 with a subsequent charge of £250 for each substantial amendment made to the application.
A study can be divided into types A, B and C, depending upon the level of risk. Type A trials do not carry increased risk to patients, as compared with usual medical care. Type B and C studies carry somewhat higher risk to patients. It can be unclear as to the level of risk that is appropriate for a given study, which affects the submission. Oxygen, as in our case study, presented an ‘unclear risk’, requiring multiple conversations with the MHRA for agreement on its classification.
Type A trials can be submitted to the MHRA under the notification scheme. Research in this category often investigates the effects of medication under licenced indications or unlicensed but common practice. The notification scheme allows fast-track applications for appropriate low-risk studies. An application under the scheme does not incur the standard fee of £250.
We were eventually successful in obtaining approval for the study from the MHRA under the notification scheme.
Trust Research & Development department (R&D)
Trials in the UK are usually conducted on NHS property, which means that the Trust R&D department often acts as both the monitor and sponsor. The R&D department is answerable to the Health Research Authority with regards to the conduct and documentation of the study.
The R&D department plays a crucial role in the development and approval of a study. In the case study, the R&D department reviewed all documentation before submission to the REC and MHRA. This approach required intensive communication between us and the R&D department, but was helpful in obtaining relatively quick approval through identifying potential issues early.
After trial approval, the R&D department remains involved as monitor. A mid-trial assessment is usually carried out to review the safety and conduct of the study. A debrief is necessary to close the trial with a subsequent archiving procedure.
Research and Ethics Committee (REC)
A national system has seen a reduction in the number of individual RECs. The more centralised system reduces variability between RECs, but has introduced delay in many cases. The quality of REC review is said to be better. The role of the REC is to ensure that the safety, dignity and health of the participants in the prospective study are not disproportionately compromised. The REC is answerable to the Health Research Authority (HRA) for its conduct.
The current system, akin to choose-and-book, allows the principal investigator to select the most appropriate centre from approximately 80 in the UK. Individual REC meetings are conducted only a few times a year, and so the nearest REC might not be the most appropriate for gaining approval rapidly. Furthermore, committee members have up to 60 days per submission to give an opinion. The majority of studies require amendments before a favourable opinion is obtained.
Most centres will make an assessment of a study in the absence of the investigating team; some have teleconferencing facilities available; a few may regard the presence of the investigators as being more-or-less mandatory.
There are five potential outcomes following a REC meeting for a clinical study:
- Full favourable opinion for the study to proceed.
- Favourable opinion with clarifications required.
- Likely favourable opinion following a review of the submitted clarifications by a REC sub-committee.
- Possible favourable opinion following a review of the submitted clarifications by a full REC committee.
- Not approved as a clinical study, usually due to problems with core aspects of study concept or design.
It is usually at this point that many trials stagnate. It is extremely rare for a trial to obtain approval on its first review with the REC; it often takes many months before full approval is given.
In the submission of our case study, the first decision was that minor clarifications should be made. It took 33 days from submission to obtaining REC approval.
Site Specific Information (SSI)
An SSI form has to be completed for trials taking place on NHS premises. The form is short compared with the others described above, but it requires the investigating team to estimate the amount of time that will be spent on the study, with a focus on the logistics and the potential effects on existing service provision. The SSI form is usually reviewed by the Trust R&D department.
Further permissions are usually required from the clinical and managerial leads in the relevant specialty for approval to be given. Some Trusts also require internal peer-review of a study, even after approval has been obtained from all the other bodies.
Other key documents
Summary of Product Characteristics (SmPC): An approved legal document required for medicinal products prior to authorisation. The SmPC is freely available and contains the posology of the drug. The MHRA requires a copy of the SmPC with submission.
Patient information sheet (PIS): A document written in easily understood language for potential participants in the study. It describes the trial procedures and any risks of the study. The REC pays particularly close attention to the quality of the PIS.
Consent form: A structured form for participants to give their official consent to taking part in the study. The REC and R&D department review the quality of the consent form very closely.
Case Report Form (CRF): The document used to record the data for the study. A well-designed CRF ensures that participants meet eligibility criteria and are properly consented. It makes it straightforward to record all the data required for the study. A poorly constructed CRF causes visits to become inefficient, allows incomplete or inaccurate results to be recorded and at worst can invalidate a study.
Key learning points
- Obtaining approval for conducting clinical research is an extremely lengthy endeavour. The process makes a four-month term in research almost useless, unless you begin the application process at least nine months in advance of a trial’s expected start date. You will need more than a year if you are applying for external funding.
- Work closely with the relevant organisations, particularly the R&D department of your Trust, the REC and the MHRA to prevent avoidable errors and delay.
- A robust study protocol is essential for a successful application and trial.
- Be guided by your academic supervisor: his/her advice is invaluable.
- Complete the online or face-to-face GCP course offered by the NIHR. It improves your understanding of clinical research. Successful completion of a GCP course is mandatory for those conducting clinical trials.
- Be ready to learn. You will acquire many skills during the application process: patience and endurance; effective communication and time management; critical appraisal; appreciation of ethical issues and patient safety.
- To be successful, the investigators have to communicate their capacity to manage potential complications, complete the trial and present the results of a relevant, well-designed study.
The future
The biggest losers in the current complex application process for clinical research approval are potential investigators who want to conduct studies without industry support.3 The effect this has had for patients is immeasurable.
In response to the complexities of the current system, the R&D submission is currently being modified into a single process called ‘HRA approval’.4 We hope that HRA approval will streamline applications further to reduce delays in approving suitable trials. The new programme will place more emphasis on obtaining expert opinion earlier, particularly in regard to safety for participants. We hope that the changes will, at least partially, reverse the long-term decline in clinical research in the UK.
Key messages
- Organising a clinical study is both complex and lengthy
- With improvements on the horizon, the process may become simpler
Conflict of interest
None declared.
References
1. NHS: Innovation Health & Wealth. Creating change: innovation, health and wealth one year on. London: Department of Health, December 2012. Available from: https://www.gov.uk/government/publications/creating-change-innovation-health-and-wealth-one-year-on
2. Department of Health. Research governance framework for health and social care: second edition. London: DoH, 2005. Available from: https://www.gov.uk/government/publications/research-governance-framework-for-health-and-social-care-second-edition
3. Clark AL, Buchanan GL. Is research declining amongst gastroenterology trainees in the United Kingdom? Clin Med 2013;13:323. http://dx.doi.org/10.7861/clinmedicine.13-3-323
4. NHS: Health Research Authority. Summary of plans for Health Research Authority assessment and approval. London: DoH, March 2014. Available from: http://www.hra.nhs.uk/documents/2014/03/summary-plans.pdf
