Postural tachycardia syndrome (PoTS) is a recently recognised condition that usually affects younger women, who develop symptoms of orthostatic intolerance and a persistent tachycardia on standing upright. Healthcare professionals, patients and the national patient support group (PoTS UK) together created a survey, and the responses of 779 UK PoTS patients were analysed. The most common symptoms of PoTS at presentation were the triad of fatigue, lightheadedness and palpitations. Mobility, ability to work or attend education, and quality of life were significantly restricted. Cardiologists, followed by patients, were most likely to be the first to suggest the diagnosis of PoTS. Patients waited a mean of almost four years from presentation to obtain their diagnosis and, meantime, psychiatric mislabeling was common. Advice given to patients regarding lifestyle changes was variable, and those referred to specialist practitioners for help, found practitioners had limited knowledge about management of PoTS. Increased education of healthcare professionals and improved services for patients are recommended.
Introduction
Postural tachycardia syndrome (PoTS) is an abnormal response by the autonomic nervous system to upright posture. It was formally recognised and defined in 1993, but is considered to be the same as Da Costa syndrome, which affected soldiers during the American Civil War,1 and as described in Sir James Mackenzie’s BMJ article ‘The Soldier’s Heart’ in 1916.2 However, PoTS primarily affects younger women who can be very disabled when upright by symptoms that are similar to those of orthostatic hypotension. The most recent consensus document,3 defines PoTS as a clinical syndrome that is usually characterised by:
- Frequent symptoms that occur with standing, such as lightheadedness, palpitations, tremulousness, generalised weakness, blurred vision, exercise intolerance, and fatigue.
- An increase in heart rate of 30 bpm or greater when moving from a recumbent to a standing position held for more than 30 seconds (or 40+ bpm in individuals 12 to 19 years of age).
- The absence of orthostatic hypotension.

Diagnosis is usually made by active stand test or tilt-table testing. Few treatments for PoTS have been tested in randomised-controlled trials (table 1). Patients are initially managed with increased fluid and salt intake to increase blood volume, avoidance of symptom triggers (heat, prolonged standing, alcohol, drugs that induce tachycardia or hypotension), small frequent meals (low in refined carbohydrates), graded exercise (initially in a horizontal position) and compression garments to reduce venous pooling. Drug treatment can be aimed at reducing tachycardia (low-dose beta blockers, ivabradine, pyridostigmine), vasoconstriction (midodrine), boosting blood volume (fludrocortisone, desmopressin) or for their sympatholytic effects in hyperadrenergic PoTS (clonidine, methyl dopa).3,4
Most published studies of PoTS patients involve small numbers and USA populations, and little is known about UK PoTS patients.
Aims
This survey was developed to obtain a current profile of PoTS patients and their experience of health services in the UK. It is hoped that the results will be used to increase the knowledge of healthcare professionals and inform the development of appropriate services to meet the needs of this group of patients. We, therefore, undertook the largest study of PoTS patients to date, engaging 1,005 people, mostly from the UK.
Methods
A group of clinicians and scientists with an interest in PoTS, patients, and trustees of PoTS UK created a survey to answer questions that were relevant to their role in assisting patients. The questions covered topics such as age, gender, location, comorbidities, diagnostic journey, support from healthcare professionals, mobility and ability to exercise, and impact of PoTS on work, education and quality of life.
The survey was piloted, then distributed by email to PoTS UK members and via the charity’s social media platforms. The survey was completed by 1,005 patients who described themselves as having PoTS during seven days in May 2015. There was representation from all but four counties within the UK. For the purposes of this report, only the 779 responses from those living in the UK and whom a doctor or specialist nurse had diagnosed with PoTS have been analysed.
Results
Symptom profile
Overall, 81% of respondents were between the ages of 18 and 49 years and 92% were female. The most common symptoms at presentation were fatigue (91%) lightheadedness, dizziness or presyncope (90%) and palpitations (86%). Syncope or blackouts were experienced by 58%. Other common presenting symptoms (in over 40%) included difficulty thinking (often described as brain fog), physical weakness, visual disturbances, breathlessness, vertigo, shakiness, chest pain, sweating, bloating, symptoms of anxiety, poor sleep, daily headache, acrocyanosis (purple-blue discolouration of hands and lower limbs), tingling in peripheries, nausea, abdominal pain, heat and exercise intolerance and ‘coat hanger’ pain (thought to be due to ischaemia of neck and shoulder muscles).
Levels of disability (figure 1)
Of responders, 5% were bedbound and 23% were wheelchair users. Only 7% were mobile without restriction, while 11% had lost their driving licence.
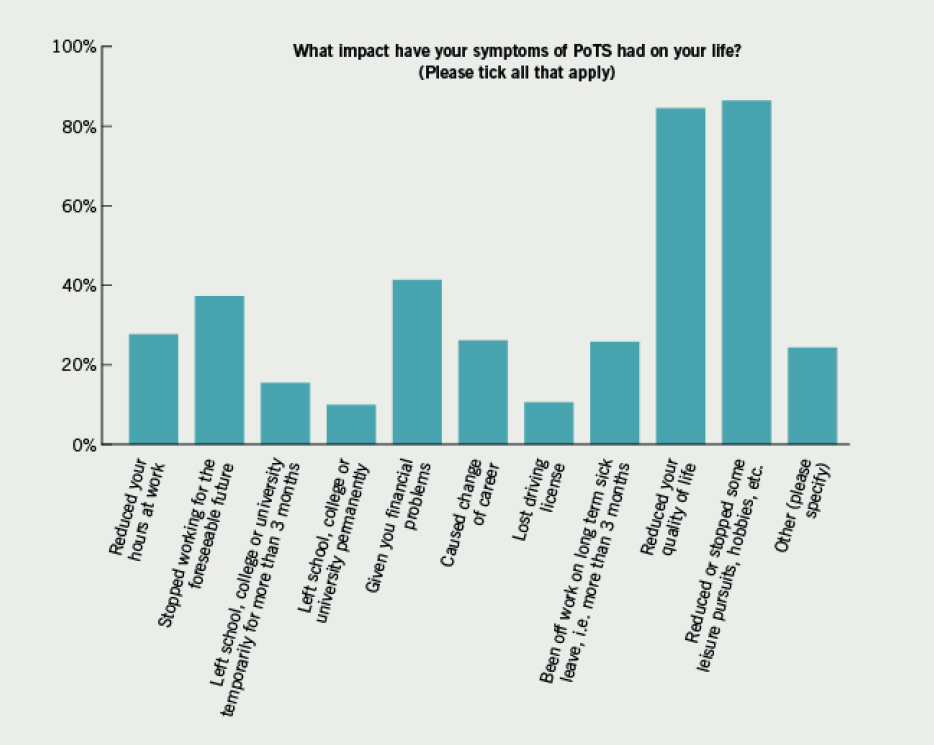
There were 37% who had to stop working for the foreseeable future due to symptoms of PoTS: 28% reduced their working hours, 26% changed their career as a consequence of their symptoms, and 41% experienced financial difficulties due to this illness. Of those under 18 years of age, 50% had been unable to attend school for more than three months and 16% were unable to attend permanently. Of all patients, 84% described a reduction in their quality of life.
Obtaining a diagnosis
Cardiologists were most likely to suggest that PoTS was the diagnosis (34%). However, a fifth of patients had to suggest a diagnosis of PoTS to their healthcare professional themselves, and in only 7% did the GP propose that the patient had PoTS. Three-quarters were diagnosed by head-up tilt-table testing. The mean time from first consulting a healthcare professional with PoTS symptoms to obtaining a diagnosis was 3.7 years. There were 48% advised that these symptoms were due to a psychological or psychiatric disorder, such as anxiety, panic disorder, depression, or hypochondriasis. This misdiagnosis occurred in a higher proportion of women (75% of female patients) than men (25% of males).
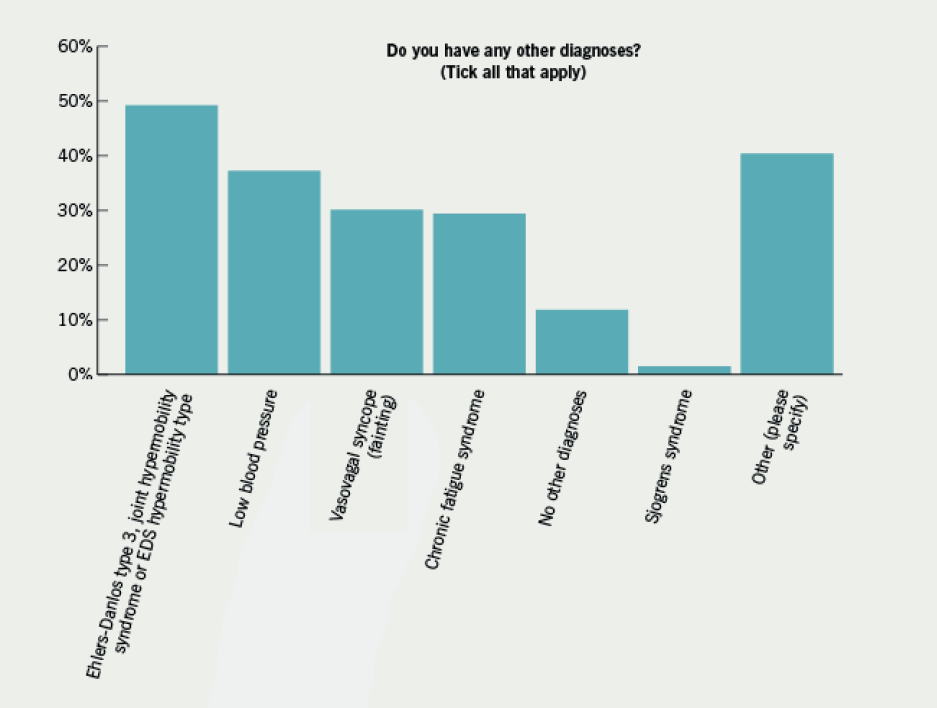
Comorbidities (figure 2)
Co-existing low blood pressure was described by 37%, 49% had Ehlers-Danlos syndrome or joint hypermobility syndrome (considered to be indistinguishable from Ehlers-Danlos hypermobility type)5 and 29% of responders had chronic fatigue syndrome. Under ‘other conditions’, 40 people reported fibromyalgia.
Treatment
The majority (93%) of patients were given lifestyle advice by their healthcare professional. Most (over 86%) were advised to increase their fluid and salt intake; 25% of patients were advised to take regular exercise. Other advice included postural manoeuvres to avoid presyncope and syncope, compression tights, reducing intake of refined carbohydrates, avoiding hot showers and baths and pacing techniques. Almost a fifth of patients were referred to a centre over 50 miles from their home for lifestyle advice. Of advisors, 43% admitted to the patient that they did not know what advice to give them.
Physical activity/exercise
Immediately before the onset of PoTS, 66% were participating in regular aerobic exercise twice a week or more; after onset only 25% were able to do so, and 48% were not undertaking any aerobic exercise. The majority who said they could exercise did so in a recumbent position, e.g. lying flat, in a chair, or swimming. A recumbent exercise bike was favoured over an upright one. Only 12% were able to exercise without limitation in an upright manner. The main barriers to exercise were fatigue and feeling unwell or faint during or after exercise: 20% were afraid they would harm themselves with exercise and 19% did not know how to exercise with PoTS. Of respondents, 15% were referred to an exercise physiologist, physiotherapist or fitness instructor in a gym.
Discussion
This is the largest survey of PoTS patients to date. Only those who had been diagnosed by a doctor or specialist nurse were included in this report. It is possible that the survey’s target group (PoTS patients who interacted with PoTS UK social media) self-selected a particular group of patients. However, their demographics were broadly in keeping with other descriptions of PoTS patients,3 i.e. younger women.
The most common symptoms described by patients at presentation were a triad of fatigue, lightheadedness and palpitations, which is the same symptom group most frequently reported in a cohort of patients in the USA.6 Patients experienced mean diagnostic delays of almost four years, although there were many who reported delays of over 20 years.
In only 7% of cases did the GP suggest PoTS as a diagnosis. This may be due to lack of awareness in primary care about PoTS or the non-specific and multiple symptoms that are associated with PoTS. However, it is possible to undertake a 10-minute stand test in a consulting room,4 and perhaps this should be considered in patients with relevant medically unexplained symptoms or chronic fatigue, especially if there is a postural link to symptoms.
Interestingly, 43% of patients reported a spinning sensation at presentation and it is possible that patients may also be presenting to ear, nose and throat (ENT) or ‘dizziness’ clinics.
With 48% of patients receiving a psychological or psychiatric misdiagnosis, opportunities to raise awareness within mental health services may improve the patient diagnostic experience.
It has been suggested that PoTS may be caused by deconditioning.7 However, this survey revealed that 66% of patients were undertaking regular aerobic exercise at the onset of PoTS, which would challenge this view and suggest it is not the cause in all patients. However, after diagnosis, only 25% are able to undertake such exercise, most commonly as a result of fatigue or because they experienced syncope/presyncope or felt unwell as a consequence. Although exercise may not be causal, disengagement and subsequent deconditioning may exacerbate symptoms of PoTS.7 There is emerging evidence from the USA8 that graded exercise rehabilitation can improve symptoms and quality of life in PoTS patients, and is now considered to be one of the first-line management strategies in PoTS.3 However, in this survey, only one quarter were advised to undertake exercise. Patients experienced difficulty in accessing local and knowledgeable lifestyle advice, despite a need for this being shown, especially in relation to exercise rehabilitation.
The survey revealed poor levels of mobility and difficulty engaging in work or education. As the group who are affected are primarily people between the ages of 18 and 49 years, it is likely that this results in significant socioeconomic morbidity and warrants further elucidation.
It is sometimes felt that patients want a pill as a ‘quick fix’ for their medical problems. Interestingly, this patient group was asked to select their research priority for PoTS and ‘most effective lifestyle changes’ proved to be more popular than research into effective medication, aetiology, prognosis and prevalence. The next question is how best to meet this need?
Further information for clinicians about PoTS is available at www.potsuk.org.
Key messages
- The most common symptoms of postural tachycardia syndrome (PoTS) at presentation are fatigue, lightheadedness and palpitations, and clinicians should be alert to considering PoTS in patients with such symptoms
- Disability is considerable; 23% are wheelchair users and 37% are unable to work
- There is a need for widespread education of health professionals about PoTS to avoid misdiagnosis and to facilitate timely diagnosis
- There is a need to improve accessible and relevant rehabilitation services for patients with PoTS in the UK
Conflict of interest
None declared.
References
1. Da Costa JM. On irritable heart; a clinical study of a form of functional cardiac disorder and its consequences. Am J Med Sci 1989;121:2–52. http://dx.doi.org/10.1097/00000441-187101000-00001
2. Mackenzie J. The Soldier’s Heart. BMJ 1916;1: 117–19. http://dx.doi.org/10.1136/bmj.1.2873.117
3. Sheldon RS, Grubb BP 2nd, Olshansky B et al. 2015 Heart Rhythm Society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm 2015;12:e41–e63. http://dx.doi.org/10.1016/j.hrthm.2015.03.029
4. Kavi L, Gammage MD, Grubb BP, Karabin BL. Postural tachycardia syndrome: multiple symptoms, but easily missed. Br J Gen Pract 2012;62:286–7. http://dx.doi.org/10.3399/bjgp12X648963
5. Tinkle BT, Bird H, Grahame R, Lavallee M, Levy HP, Sillence D. The lack of clinical distinction between the hypermobility type of Ehlers-Danlos syndrome and the joint hypermobility. Am J Med Genet A 2009;149A:2368–70. http://dx.doi.org/10.1002/ajmg.a.33070
6. Thieben M, Sandroni P, Sletten D et al. Postural orthostatic tachycardia syndrome: the Mayo Clinic experience. Mayo Clin Proc 2007;82:308–13. http://dx.doi.org/10.4065/82.3.308
7. Fu Q, VanGundy TB, Galbreath MM et al. Cardiac origins of the postural orthostatic tachycardia syndrome. J Am Coll Cardiol 2010;55:2858–68. http://dx.doi.org/10.1016/j.jacc.2010.02.043
8. Fu Q, Van Gundy TB, Shibata S, Auchus RJ, Williams GH, Levine BD. Exercise training versus propranolol in the treatment of the postural orthostatic tachycardia syndrome. Hypertension 2011;58:167–75. http://dx.doi.org/10.1161/HYPERTENSIONAHA.111.172262
