Implementation of a new specialty training Curriculum in Cardiology from August 2007 will bring significant changes to specialist training in cardiology. The format, delivery and evaluation will differ, and these changes are relevant to both existing and newly appointed trainees. This article aims to summarise the changes and incorporates presentations by the Cardiology Specialist Advisory Committee at the British Cardiovascular Society conference in June 2007.
The 2007 Curriculum in Cardiology
The 2007 Curriculum in Cardiology builds on the existing curriculum and aims for a competency-based approach to assessment.1 It will be implemented for all new trainees starting at ST3 level from August 2007. Newly enrolled trainees will undertake three years’ core training followed by two years of subspecialty modules (figure 1). The emphasis on some disciplines will change, for example, less emphasis on pacing numbers, and more emphasis on echocardiography experience, more structured training in adult congenital heart disease, and the introduction of new areas of training, e.g. cardiovascular magnetic resonance.
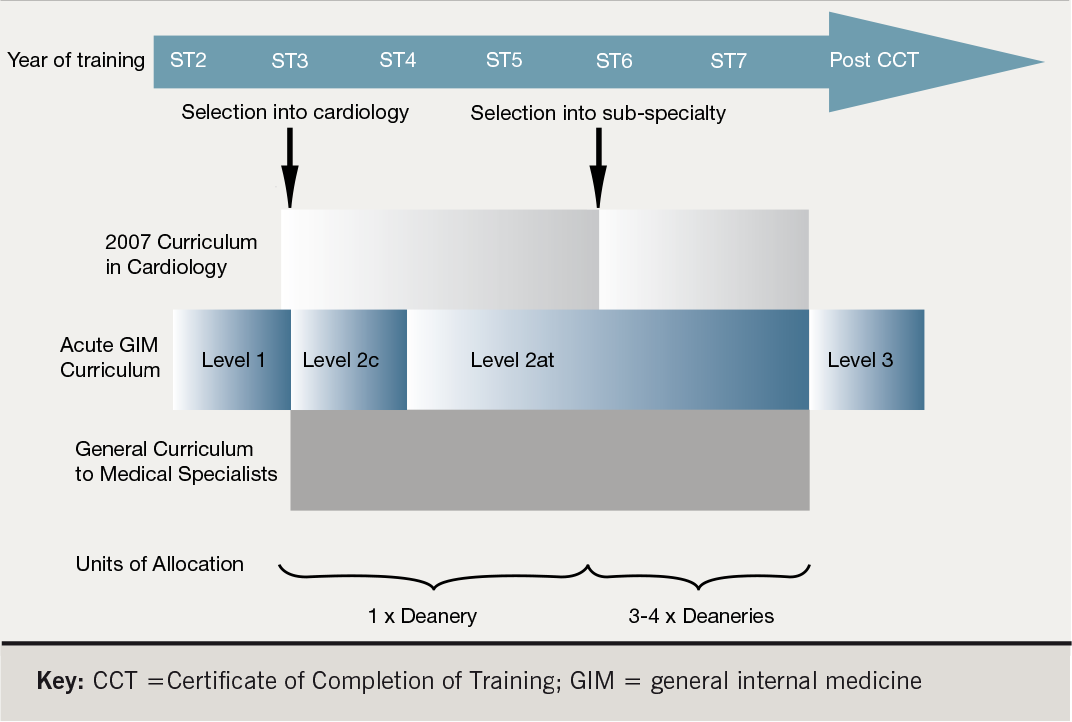
Training in cardiology will run alongside the generic curriculum for medical specialists and the acute General Internal Medicine (GIM) curriculum.2,3 Trainees will be required to demonstrate leadership, management, teaching, research and generic clinical skills. Research competency is a key part of the generic curriculum and out of programme research is encouraged.
Basic acute GIM training should be completed in the first year (ST1). Further training is required, but is dependent on the level aimed for:
- Level 1 achieved by the end of ST2
- Level 2c (core competency in GIM for all cardiologists) usually achieved by the end of ST3
- Level 2at (if desired, for competency to participate in acute GIM as a consultant) achieved by the end of ST7
- Level 3 will only be required for those trainees who wish to be qualified as a clinical lead in GIM, i.e. to run an acute admissions unit. This will require additional (post certificate of completion of training [CCT]) training in GIM (unless the subspecialty chosen lends itself to further GIM training).
Therefore all trainees should have completed core medical training in ST1 and ST2, requiring Level 1 competence in acute medicine. In ST3, all trainees must acquire Level 2 competence in those elements of acute medicine relevant to cardiology. Those who wish to undertake acute medicine at consultant level will have to obtain the remainder of the Level 2 competencies in ST6 and ST7.
Workplace-based assessment
workplace-based assessments
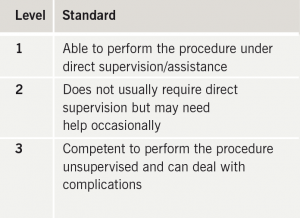
Until now, there has been limited workplace-based assessment of trainees.4,5 Competency-based assessments are designed to measure achievement, maintain standards, motivate trainees, identify learning needs, and predict future performance.5,6 It will be central to the 2007 Curriculum and comprise knowledge-based assessment (KBA), multi-source feedback (MSF, 360), mini clinical evaluation exercise (Mini-CEX), and directly observed procedural skills (DOPS).7-10 Other assessment formats under development include: patient satisfaction questionnaires (PSQ), case-based discussions (CBD), acute care assessment tool (ACAT), and DOPS for advanced procedural skills. There will be three recognised levels of competence (table 1). To assure full competence, six DOPS assessments (by a minimum of two different assessors) are required for each of cardiac catheterisation, echocardiography, pacing, cardioversion and pericardiocentesis. Workplace-based assessments will apply to trainees appointed to ST3 from August 2007 and form part of a portfolio of evidence on trainees’ progress, reviewed at the Record of In Training Assessment (RITA). Trainees who have failed their assessments may be offered targeted training. Current trainees are encouraged to undertake these assessments, but with appropriate flexibility, as advised by their training programme directors during the transition period. The Cardiology RITA Decision Grid will map the 2007 Curriculum to assessments for each learning point on the curriculum according to the Postgraduate Medical Education & Training Board (PMETB) principles of assessment.11 The Grid outlines the expected competency requirements of trainees as they progress through core and subspecialty training and the parallel Generic and GIM (acute) medicine curricula.
Selection into ST3
This is currently unclear as the future of Modernising Medical Careers (MMC) and the whole process of selection into specialist training are under review by a committee chaired by Sir John Tooke. In its evidence to the Tooke review, the Royal College of Physicians advocated uncoupling of run-through training, with re-establishment of selection into specialties (e.g. cardiology) at ST3 level. This position is supported by the Specialist Advisory Committee, who have developed a cardiology-specific application process for entry into ST3. If the proposals are approved, this will comprise three elements:
- A national person specification.
- A national application form detailing qualifications, previous experience, competencies achieved in acute medicine, evidence of audit, information technology (IT) skills, research, and evidence of outstanding achievement inside and outside of medicine. There will be a wide score range and more weight given to a completed MD/PhD, grant funded research and publications than under the current MMC criteria.
- A structured interview process, probably at deanery level.
Selection into subspecialties
A formalised subspecialty training programme for the final two years of training (ST6 and 7) has been proposed, based around the clustering of three to four neighbouring deaneries into geographical ‘Units of Application’ large enough to offer the relevant posts in all subspecialties, except perhaps Grown Up Congenital Heart Disease (GUCH). Competitive selection to these deanery groups would occur, and a national clearing scheme would also be in place. These proposals, together with the detailed curricula for the subspecialty programmes themselves, await ratification from PMETB.
Existing specialist registrars
At present, existing specialist registrars (SpRs) will not be re-designated as specialty registrars (StRs). However, it is recommended that current SpRs acquaint themselves with the 2007 Curriculum and assessment tools. Assessments are mandatory for all trainees appointed after 2003 (although current SpRs will not be bound to the 2007 Curriculum). Trainees wishing to adopt some aspects of the 2007 Curriculum will need to negotiate with Training Programme Directors/Specialty Training Committees. SpRs will continue to have the option of an ‘out of programme’ experience for research if prospectively approved.
Summary
Training in cardiology is undergoing a significant process of change. It will become more structured and trainees will be formally evaluated by several methods. Both newly appointed and existing SpRs should therefore familiarise themselves with these changes. Further information may be obtained by accessing the Joint Royal Colleges of Physicians Training Board website, www.jrcptb.org.uk.
Conflict of interest
None declared.
References
- Joint Royal Colleges of Physicians Training Board. Specialty training curriculum for Cardiology.
May 2007. Available from: www.jrcptb.org.uk/Specialty/Pages/Cardiology.aspx - Joint Royal Colleges of Physicians Training Board. Generic curriculum for medical specialists. 2007. Available from: www.jrcptb.org.uk/Specialty/Documents/
- Joint Royal Colleges of Physicians Training Board. General internal medicine (acute) curriculum. 2007. Available from: www.jrcptb.org.uk/Specialty/Documents
- Wragg A, Wade W, Fuller G, Cowan G, Mills P. Assessing the performance of specialist registrars. Clin Med 2003;3:131–4.
- PMETB Workplace Based Assessment Subcommittee. Workplace based assessment. Postgraduate Medical Education Training Board, 2005.
- Norcini JJ. Work based assessment. In: Cantillon P, Hutchinson L, Wood D (ed.). ABC of learning and teaching in medicine. London: BMJ publishing group, 2003;36–8.
- Harden RM, Crossley J, Davis MH. An introduction to outcome-based education. Medical Teacher 1999;21:7–14.
- Miller GE. The assessment of clinical skills/competence/performance. Acad Med 1990;65:S63–S67.
- Norcini JJ, Blank LL, Arnold GK, Kimball HR. The Mini-CEX (Clinical Evaluation Exercise). A Preliminary Investigation. Ann Intern Med 1995;123:795–9.
- Holmeboe ES. Faculty and the observation of trainees’ clinical skills: problems and opportunities. Acad Med 2004;79:16–22.
- Southgate L, Grant J. Principles for an assessment system for postgraduate medical training. A working paper from the Postgraduate Medical Education Training Board. Postgraduate Medical Education Training Board, 2004.
