General news from the world of Cardiology
New data on intensive glucose lowering in type 2 diabetes
The results of three large trials investigating the clinical effects of intensive glucose lowering in patients with type II diabetes were presented at the recent American Diabetes Association meeting in San Francisco, USA, and have shown somewhat conflicting results.
The ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial was stopped earlier this year because of an increased mortality in the intensive glucose lowering group. The two other trials – ADVANCE (Action in Diabetes and Vascular Disease – Preterax and Diamicron MR Controlled Evaluation) and VADT (Veteran’s Affairs Diabetes Trial) – were reassuring in that they did not show such a hazard in their intensive groups, although neither ADVANCE nor VADT showed any cardiovascular benefits for intensive lowering of blood glucose, the main goal of the studies.
Microvascular results have only been made available from the ADVANCE trial, and showed a benefit on diabetic renal complications with intensive glucose lowering.
The ACCORD and ADVANCE papers were published together in the June 12 issue of the New England Journal of Medicine. The VADT trial has not yet been published.
The ADVANCE trial enrolled 11,140 patients with type 2 diabetes, who were at least 55 years old, and had a history of, or at least one risk factor for heart disease. They were randomised to intensive glucose control (aiming for HbA1c levels of 6.5% or less), starting with modified release gliclazide with other agents added, or to standard treatment with the aim of reaching the current guidelines target for HbA1c of 7.0%. After the four years’ treatment time, patients in the intensive group reached a mean HbA1c of 6.5% and those in the standard group achieved 7.3%. The major benefit shown in the intensive group was a 21% relative reduction in new or worsening diabetic nephropathy compared with the standard-treatment group. There was also a 9% reduction in new microalbuminuria. No significant difference was found between the treatment groups for major cardiovascular events.
The ADVANCE investigators pointed out that their trial was actually quite different from ACCORD in that the ACCORD intensive group had their glucose levels lowered more aggressively and more quickly than in ADVANCE, which adopted a more pragmatic approach to trying to achieve tight glucose control. In addition, 28% of the intensive-treatment group gained 10 kg or more in ACCORD, whereas in ADVANCE there was no change in body weight in the intensive group.
The VADT trial involved 1,791 patients with type 2 diabetes who were a higher-risk population than those enrolled in either ACCORD or ADVANCE, with mean baseline HbA1c levels of 9.5%, which was reduced to 6.9% in the VADT intensive group and 8.4% in the standard group. Main results showed that the better glycaemic control in the intensive group was not associated with any reduction in cardiovascular events, with a total of 263 such events in the standard-treatment group and 231 in the intensive-treatment group, a non-significant difference.
No change to guidelines?
The lack of cardiovascular benefit seen in any of these trials has led many experts to predict that guidelines will probably not change to recommend lower HbA1c levels than those currently advised.
Dr Rury Holman (Professor of Diabetic Medicine at Oxford University) said he thought current guidelines should remain unchanged. “We should continue to strive to prevent HbA1c values rising as people’s diabetes progresses to avoid microvascular complications but exercise caution about reducing blood glucose aggressively in those with longstanding diabetes and cardiovascular disease in the expectation that this will reduce cardiovascular disease risk,” he said.
But ADVANCE study director Dr Anushka Patel (George Institute, Sydney, Australia) said that ADVANCE shows that going down to HbA1c levels of 6.5% can be achieved safety, and results in a one-fifth reduction in renal complications. “Diabetes is the most common cause of renal failure worldwide, and developing renal complications puts you at increased risk of developing future cardiovascular events as well as death from any cause. So reducing renal complications is very worthwhile,” she commented.
Two editorials accompanying the publications suggest that a target HbA1c level of approximately 7% remains an appropriate target. But they point out that all the current studies involved patients with or at high risk of cardiovascular disease and that whether achieving glycaemic targets below 7% will be beneficial to diabetes patients with a low risk of cardiovascular disease remains unknown.
Aliskiren reduces proteinuria in patients with diabetic nephropathy
The direct renin inhibitor aliskiren (Rasilez®) significantly reduced proteinuria in patients with diabetic nephropathy when added to conventional treatment in the AVOID trial.
The trial, reported in the June 5 issue of the New England Journal of Medicine, was conducted by a team led by Dr Hans-Henrik Parving (Rigshospitalet, Copenhagen, Denmark).
In the study, 599 patients with type 2 diabetes and nephropathy were randomised to six months’ treatment with aliskiren or placebo. All patients also received the maximum recommended dose of losartan.
Results showed that the aliskiren group had a 20% reduction in proteinuria compared to those receiving losartan alone (p<0.001). In addition, significantly more patients given aliskiren had a 50% reduction in albuminuria than those given losartan alone. There was little difference in blood pressures between the two groups, suggesting the benefits seen were not related to blood pressure reductions.
But an accompanying editorial points out that this was a surrogate end point trial, and whether this treatment would actually result in sustained renoprotection and a reduction in clinical events has yet to be shown.
This is, however, being investigated in the a large randomised trial, ALTITUDE, which is examining whether aliskiren, when added to conventional therapy, delays heart and kidney complications in around 8,600 patients with type 2 diabetes at high risk for cardiovascular and renal events. The study began in late 2007, with completion anticipated by 2012.
ALTITUDE is part of the ASPIRE HIGHER clinical trial programme, which includes two other large-scale outcome trials with aliskiren. These are:
- the ATMOSPHERE trial, evaluating the effects of the drug on cardiovascular morbidity and mortality in patients with heart failure
- the APOLLO study, which will assess the effectiveness of aliskiren in preventing cardiovascular morbidity and mortality in elderly patients with or without hypertension and other risk factors.
New anti-arrhythmic reduces death/hospitalisation in AF patients
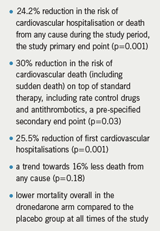
A new anti-arrhythmic agent, dronedarone, significantly reduced the incidence of cardiovascular hospitalisation or death in patients with atrial fibrillation (AF) in the ATHENA trial.
The trial was presented by Stefan Hohnloser (JW Goethe University, Frankfurt, Germany) at the Heart Rhythm 2008 meeting held in San Francisco, USA, in May. He stated: “ATHENA is the first large trial that measures if an anti-arrhythmic drug can reduce the composite outcome of the time to first cardiovascular hospitalisation or death from any cause in an AF population. The positive effects of dronedarone on the AF population are significant and extremely important to the field of cardiology”.
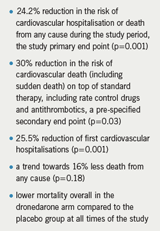
The trial randomised 4,628 patients with AF or atrial flutter, or with a history of the disorder to receive dronedarone or placebo with a minimum follow-up of one year. The primary study outcome was time to first cardiovascular hospitalisation or death from any cause and secondary outcomes were total death, cardiovascular death and cardiovascular hospitalisation. Study findings are summarised in table 1.
In addition, unusually for an anti-arrhythmic agent, dronedarone seemed to have a good safety profile, raising hopes that it could be a less toxic replacement for amiodarone. Adverse event rates in ATHENA were not significantly greater with dronedarone (72%) than with placebo (69%), and serious adverse events were reported by 20% of dronedarone patients and 21% of those on placebo.
While the ATHENA trial compared dronedarone against placebo, which is necessary for approval, doctors are eager to judge the efficacy of the new agent in relation to amiodarone. The DIONYSUS trial is now underway to look at this issue, comparing the two drugs for maintenance of sinus rhythm in AF patients.
Arrhythmias remaining undiagnosed
Patients with potentially fatal cardiac arrhythmias are not being diagnosed or treated, according to a new survey of GPs.
The survey, sponsored by Medtronic, found that over 80% of GPs questioned believed that cardiac arrhythmia is under-recognised and just a quarter felt confident in reading electrocardiograms (ECGs), an essential part of arrhythmia diagnosis.
The research also indicated that there is high demand among GPs for clarity and accuracy of patient referral pathways, for those patients experiencing key symptoms of cardiac arrhythmia, such as blackouts. Although blackouts are more likely to be the result of a cardiovascular condition, it is estimated that up to 150,000 UK patients, predominantly children, have been misdiagnosed as having epilepsy.
According to the survey, only one in four GPs would refer a patient with blackouts to a cardiologist or a GP with a special interest in cardiology. Instead patients are referred to neurologists or age-specific physicians such as paediatricians.
A new online module, supported by the Arrhythmia Alliance, is now available at www.doctors.net.uk, to try to improve understanding, diagnosis and treatment of cardiac arrhythmias.
New NICE guidance issued on lipid modification…
The National Institute for Health and Clinical Excellence (NICE) and the National Collaborating Centre for Primary Care (NCC-PC) have issued a new clinical guideline on lipid modification (Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease). Key recommendations in this guidance are summarised in table 1.
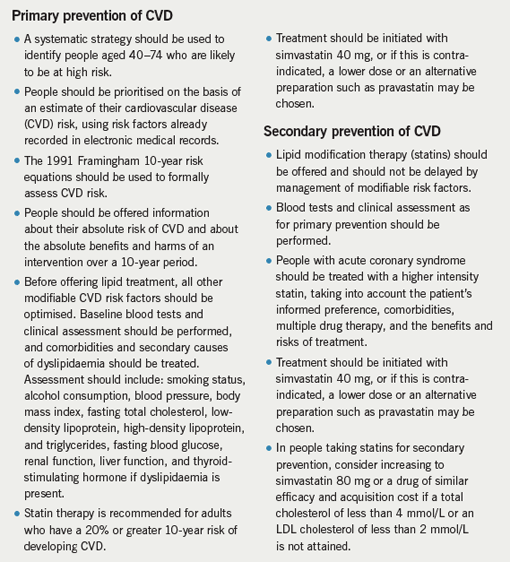
The cholesterol charity H.E.A.R.T UK, while welcoming much of the guidance, such as the case identification and risk screening recommended, has said it was a missed opportunity. It points out that cholesterol targets are omitted from the guidance and that the treatment strategy adopted in the guideline is not optimal.
The guideline, together with a version for patients, is available from the NICE website at www.nice.org.uk/CG067.
…and diabetes
NICE and the National Collaborating Centre for Chronic Conditions (NCC-CC) have also issued updated guidance on type 2 diabetes management. It replaces four sets of 2002 NICE clinical guidelines (blood glucose, renal disease, retinopathy, blood pressure/blood lipids) and three NICE technology appraisals on long-acting insulin analogues (2002), glitazones (2003) and patient education models (2003).
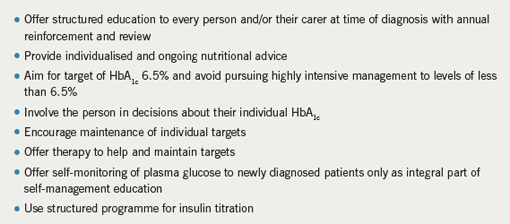
Key points from the guidance are summarised in table 2. The guidelines also provide key recommendations and management algorithms for: patient education, dietary advice, blood glucose control, blood pressure management, kidney damage, eye screening, neuropathic pain management and other neuropathic complications. The full guidance and a quick reference guide can be downloaded from www.nice.org.uk/CG66.
A rapid update on newer oral agents covering incretin mimetics and incretin enhancers is to be published next February. This will also address safety concerns, specifically in relation to rosiglitazone regarding the risk of cardiovascular adverse events. The current recommendations give little guidance in this area.
Dr Roger Gadsby, a general practitioner and member of the NICE guideline development group, explained that the cut-off date for evidence for review was prior to the May 2007 Nissen publication. “Evidence that emerged subsequently and new regulatory guidance was not part of the current remit but will be taken into consideration for the update.” The European Medicines Agency recommended in January that rosiglitazone-containing medicines include a warning against using in patients with ischaemic heart disease and/or peripheral arterial disease. This warning did not apply to pioglitazone.
The new guideline recommends glitazones second-line if a sulphonylurea results in hypoglycaemia or if metformin is not tolerated and third-line as an alternative to insulin.
…and on rimonabant
NICE has issued a new guidance on the use of the obesity drug, rimonabant. It states that rimonabant is recommended as a possible treatment for adults who are obese (a body mass index [BMI] of 30 kg/m2 or more) or who are overweight (BMI of 27 kg/m2 or more) and have risk factors, such as type 2 diabetes or high levels of cholesterol.
Rimonabant should be used at the same time as a calorie-controlled diet and exercise in people who have tried the weight-loss medicines orlistat and sibutramine, but when they haven’t worked or cannot be taken because side effects have occurred or are expected. Treatment with rimonabant should continue for longer than six months only if the person has lost at least 5% of their body weight since starting treatment. If the person returns to their original body weight, rimonabant treatment should be stopped. Treatment should only continue for longer than two years after a medical assessment and a discussion of the risks and benefits.
PROFESS: aspirin/dipyridamole vs. clopidogrel for prevention of recurrent stroke
The largest clinical trial for secondary stroke prevention ever conducted has shown similar results for the combination of aspirin and extended-release dipyridamole versus clopidogrel, although the trial did not meet its primary end point of non-inferiority of the combination versus clopidogrel.
The PROFESS (Prevention Regimen For Effectively avoiding Second Strokes) trial, presented at the European Stroke Conference, held in Nice, France, in May, enrolled 20,332 patients who had suffered a non-cardioembolic ischaemic stroke within the previous 120 days. They were randomised to aspirin (25 mg) plus extended-release dipyridamole 200 mg twice daily, or clopidogrel 75 mg once daily.
The primary outcome – recurrent stroke – was not statistically significantly different between the groups, but the investigators noted that they were not able to conclude that the combination was non-inferior to clopidogrel as the upper boundary of the 95% confidence intervals crossed the non-inferiority margin of 1.075 (see table 1).
In a further exploratory analysis of the main secondary end point of the composite of stroke, myocardial infarction or vascular death, the two treatments had similar outcomes (13.1% in each group) . The aspirin/dipyridamole group had a higher number of haemorrhagic strokes compared to clopidogrel (0.8% and 0.4%, respectively) while ischaemic stroke recurrences were less frequent in the combination group (7.7% and 7.9%, respectively).
A post-hoc analysis showed comparable numbers of death and disabling strokes and a similar neurological outcome as measured by the modified Rankin Scale at three months after the recurrent stroke and at the end of the trial in the two treatment arms.
Major haemorrhagic events were observed more frequently in the aspirin/dipyridamole group compared with clopidogrel (4.1% versus 3.6%), and headache was also more frequent with the combination, but the benefit-risk ratio expressed as the combination of recurrent stroke and major haemorrhage was not significantly different between the two groups – 11.7% for aspirin/dipyridamole vs. 11.4% for clopidogrel. “Given the high prevalence of stroke and recurrent stroke in ageing societies, physicians need a range of treatment options so they can offer patients a regimen tailored to their individual needs,” said Professor Hans-Christoph Diener (University of Essen, Germany), one of the three principal investigators of the study. “Landmark trials like PRoFESS will help clinicians make evidence-based treatment choices and ensure that patients receive optimal therapy for their condition,” he added.
In a factorial design, patients were also randomised to telmisartan 80 mg/day or placebo. At the end of the study, 8.7% of patients experienced recurrent stroke in the telmisartan arm versus 9.2% in the placebo arm, a difference that was not statistically significant. Thus, the primary end point of superiority of telmisartan versus placebo could not be demonstrated. The mean follow-up period was 2.5 years, and it is unclear whether a longer follow-up period would have yielded statistical significance, the investigators said.
