Vascular surgery is associated with a substantial risk of cardiovascular events and death. Cardiac troponin I (cTnI) is a contractile protein that is a highly sensitive and specific marker of myocardial necrosis. This case series examines the clinical course of 10 patients who had an asymptomatic pre-operative elevation in cTnI and underwent a vascular surgical procedure.
A prospective, two-year, observational, single-centre cohort study of all patients undergoing a vascular procedure with an expected cardiac event rate of >5% was performed. Pre-operative cTnI was carried out (cTnI >0.02 ng/ml positive). Post-operative screening for cardiac events at post-operative days two and five was performed.
Two-hundred and thirteen patients were recruited, of whom 11 (5.2%) had an asymptomatic elevated pre-operative cTnI. Ten patients in whom the pre-operative cTnI was not known prior to surgery, or in whom a procedure could not be delayed proceeded with the operation. One patient had surgery deferred. Four patients suffered a post-operative cardiac event and five died.
The outcome in this case series was poor with death in 50% of those taken to theatre and cardiac events in 40%. An elevated pre-operative cTnI in an otherwise asymptomatic patient identifies a very high-risk group of patients.
Introduction
Vascular disease is a systemic disorder, with 50–60% of patients undergoing peripheral vascular procedures having co-existent severe coronary artery disease and only 10% having normal coronary arteries.1,2 It is unsurprising, therefore, that vascular surgery is associated with a substantial risk of major adverse cardiovascular events (MACE) and death.2,3
Cardiac troponin I (cTnI) is a contractile protein that is released into the circulation after myocardial cell injury. Unlike other cardiac-related enzymes, cTnI is not found in skeletal muscle and is therefore a highly sensitive and specific marker of myocardial necrosis,4,5 and a specific marker of myocardial infarction following surgery.5 Elevated cTnI after major vascular surgery is associated with an increased risk of short-term mortality and morbidity,6 and is an independent predictor of intermediate and long-term outcomes.6-11 It is widely recognised that pre-operative determination of impaired cardiac function correlates with MACE. The impact of adverse cardiac function on post-operative outcome is well established and has been refined since Goldman’s first risk stratification.12 The sophistication of cardiac testing has changed dramatically since then with both functional and stress testing with radioisotope scanning, biochemical tests, electrocardiogram (ECG), echocardiographic and angiographic studies. However, 50% of cardiac events post-operatively and 29% in the general population are asymptomatic and detected principally through cTnI analysis.13 While the cause of asymptomatic elevations in cTnI has been widely correlated with angiographic findings and outcome in patients presenting to cardiology,13 other than a case report and a series of amputation patients,14,15 there are no studies that have systematically aimed to determine the incidence of elevated pre-operative cTnI and the impact on MACE post-operatively.
The aim of this case series is to report the incidence and outcome of asymptomatic elevated pre-operative cTnI in 213 consecutive patients undergoing major vascular surgery.
Patients and methods
Patients
A prospective, observational, single-centre cohort study was performed over a two-year period (April 2004 to April 2006) in Glasgow, with the aim of studying cardiac risk stratification and novel markers in non-cardiac surgery. Inclusion criteria for participation included an estimated procedure-related cardiac event rate of 5% (lower limb revascularisation, aneurysm repair, major amputation). In addition to pre-operative tests done at the discretion of anaesthetic and surgical teams, each patient had a pre-operative measurement of cTnI and an ECG performed on the day before surgery. The cTnI was available to the anaesthetic teams if requested, but was not routinely sought. Basic demographic data and factors relating to the risk of surgery were prospectively gathered for each patient. Patients were excluded if there was evidence of unstable coronary artery disease pre-operatively (cardiac chest pain or ischaemic ECG changes), if the surgery was emergency (<24 hours) or if they were unable to provide informed consent. Central Office for Research Ethics Committee (COREC) and local research and development committee approval was obtained for the study.
Sample collection and analysis
Pre-operative venous blood samples were collected the evening before surgery in sterile lithium heparin tubes. Serum cTnI was measured using the ARCHITECT STAT troponin I immunoassay (Abbot Diagnostics), which had an assay range of 0.02–50 ng/ml with a sensitivity of ≤0.01 ng/ml. Assay precision was ≤10% of the concentration value (CV) for samples ≥0.20 ng/ml. The lowest assay value exhibiting a 10% CV on the precision profile was 0.032 ng/ml. A positive result was taken as a cTnI >0.02 ng/ml.
Post-operative follow-up
Post-operative screening for cardiac events consisted of daily clinical assessment, and serial ECGs and cTnI measurement at post-operative days two and five. These test results were made available to the treating clinicians. Other investigations were performed as indicated. Clinical follow-up continued to six-weeks after recruitment. A cardiologist blinded to the study data compared the paired pre- and post-operative ECGs at the end of the study. End points were non-fatal myocardial infarction (MI) and cardiac death. MI was defined by the presence of a typical rise and fall of plasma cTnI with either ischaemic symptoms +/- development of Q-waves on ECG +/- ischaemic changes noted on ECG +/- coronary artery intervention. Cardiac death was determined by review of all post-operative data by two cardiologists blinded to pre-operative cTnI levels.
Statistical analysis
Statistical analysis was conducted using SPSS® statistical software package. All analyses were performed between groups using a two-tailed Fisher’s exact test.
Results
Population
During the two-year study, a total of 222 patients underwent an elective major vascular procedure of which 213 (144 male, 69 female) were included in the study. Nine patients were excluded (five unable to give informed consent, three with unstable cardiac disease and one missing pre-operative cTnI sample). Seventy-four (35%) patients underwent a major lower extremity amputation, 72 (34%) abdominal aortic surgery, 37 (17%) infrainguinal bypass and 30 (14%) extra-anatomical bypass. Co-morbidity included 84 (39%) patients with ischaemic heart disease, 44 (21%) congestive cardiac failure, 23 (11%) renal impairment and 60 (28%) with diabetes mellitus. Sixty (28%) patients were prescribed a pre-operative statin and 28 (13%) a beta blocker. All patients were on antiplatelet therapy.
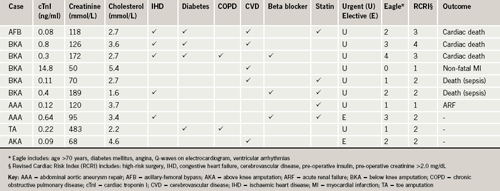
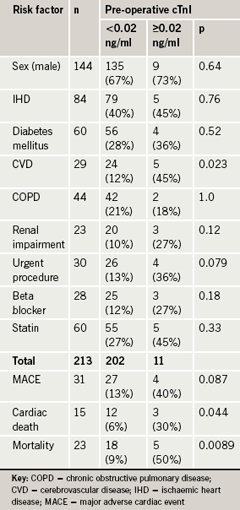
Eleven (5.2%) of the 213 patients had an asymptomatic raised pre-operative cTnI (median cTnI 0.22 ng/ml, range 0.08–14.8 ng/ml). All 11 patients had significant co-morbidity: five patients had known ischaemic heart disease, five had cerebrovascular disease, four had diabetes mellitus and three had renal impairment. Eight out of the 11 patients had multiple risk factors (table 1). Patients with an elevated cTnI had a significantly higher risk of cerebrovascular disease (p=0.023). Although there were no other significant risk factors, the proportions of elevated asymptomatic cTnI patients with renal impairment (24% vs. 12%), who were prescribed beta blockers (27% vs. 12%) or had an urgent procedure (36% vs. 13%) were more than double compared to the normal cTnI patients (table 2).
Outcome
Patients identified with an asymptomatic elevated pre-operative cTnI were more likely to have undergone major lower extremity amputation (7/11 [64%]), with nearly double the proportion compared with the normal cTnI group (67/202 [33%]), although this difference was not significant (p=0.262). Other procedures included two for open abdominal aortic aneurysm (AAA) repair and an axillary-femoral bypass. The management of patients with an elevated cTnI varied with eight of the 11 patients initially having no change in their routine peri-operative course. This was subsequently reviewed due to the poor outcome of those that proceeded to theatre. As a consequence, pre-operative cTnI was made available to both anaesthetist and surgeon. Of the remaining patients with elevated pre-operative cTnI, one was started on a peri-operative beta blocker, and one of the lower extremity amputations was delayed to re-measure cTnI and was taken to theatre uneventfully with a persistently elevated cTnI. One final patient scheduled to undergo an aorto-bifemoral bypass was delayed for cardiac investigation and subsequently underwent triple coronary artery bypass grafting. This patient consequently had an aorto-bifemoral graft without complication.
The incidence of MACE overall, though not significant, was three times more common in the asymptomatic elevated cTnI patients (4/10 (40%) vs. 27/202 (13%), p=0.087). Of the 10 patients who proceeded to theatre with a pre-operative elevated cTnI, four suffered a post-operative MACE: three cardiac deaths (30%) and one non-fatal MI (10%). There were a total of five deaths (50%) with two further deaths secondary to sepsis. The number of post-operative MACE in the ‘normal’ cTnI group was 27 (13%) with 12 cardiac deaths (6%) and 15 non-fatal MIs (7%). There were a total of 18 deaths (9%) in the ‘normal’ cTnI group. There was a statistically significant difference in cardiac death (p=0.044) and in all-cause mortality (p=0.0089) between those with a normal pre-operative cTnI and those with an asymptomatic elevation of cTnI, with poorer outcome in the elevated cTnI group.
Discussion
This is the first inclusive study to report the incidence and outcome of asymptomatic elevated pre-operative cTnI. Of the 213 patients included, 5.2% had an asymptomatic elevated cTnI. Such patients have a significantly higher risk of cardiac death and all-cause mortality, with a trend towards an increased proportion of MACE, therefore predicting poor outcome.
The outcome in these patients was poor with death in five of 10 patients. A total of four patients had a MACE of which three were cardiac death. All of the patients who suffered an event were urgent cases, most of whom required a lower extremity amputation for critical ischaemia. The pre-operative Eagle16 and revised cardiac risk index (RCRI)17 scores for these patients was two or greater, predictive of poor cardiac outcome in patients undergoing vascular surgery.17,18 In addition, asymptomatic elevations have been shown to identify patients who are at increased risk of first cardiac events and who have increased mortality over 10 years irrespective of surgery, with potential contributing subclinical silent myocardial damage.19,20 This implies that pre-operative asymptomatic elevations in cTnI identify a subset of patients from an already high-risk population in whom the outcome is likely to be considerably worse.
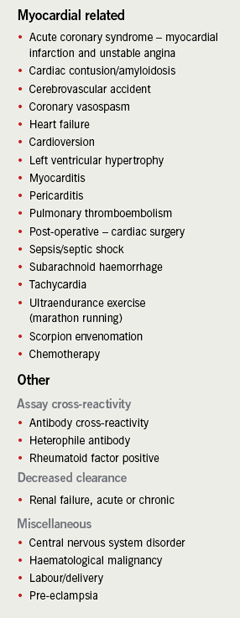
Evidence for a potential cause of the elevated cTnI was present in the majority of cases such as sepsis in the amputation patients,21 and renal impairment22-24 (table 3). Co-morbidity was common in patients who had elevated cTnI, with a significantly greater incidence of cerebrovascular disease in the elevated cTnI group. There was a high incidence of cardiac risk determinants such as diabetes mellitus, chronic kidney disease and ischaemic heart disease, known to be associated with asymptomatic elevations in cardiac troponin.25 The most concerning alternative reason for such an elevation, however, includes acute coronary syndrome and pulmonary embolism. Further investigation may therefore be of benefit and could involve investigating the cause of elevated cTnI and obtaining a cardiology opinion. A pragmatic approach may be to delay operative stress where feasible, and await a fall in levels, such as that seen in a cardiac event. This could allow further patient optimisation or cardiac intervention.26 Where delay and intervention is not practicable, other options could involve change in anaesthetic choice, closer peri-operative monitoring or modification of surgical procedure.
In summary, this case series presents 11 patients with an asymptomatic elevated pre-operative cTnI. Although the numbers are limited, this is the largest case series of patients with a pre-operative elevation of cTnI in the literature and is associated with a poor prognosis. This case series could be taken forward to commence routine pre-operative cTnI measurement in those patients thought to be high risk.
Acknowledgement
This was presented to Vascular Society GB and I, Edinburgh 2006.
Conflict of interest
This study was funded through Research Funds of the Cardiology and Vascular Surgical Units of Gartnavel General Hospital, Glasgow and the Western Infirmary, Glasgow.
Key messages
- Approximately 5% of asymptomatic patients scheduled for elective major vascular surgery have an elevated pre-operative cardiac troponin I (cTnI)
- Elevated pre-operative cTnI identifies patients at high peri-operative risk
- The outcome in these patients is poor with 40% suffering a major adverse cardiac event and death in 50%
- Consideration and reassessment of further management should be given to ensure the safest peri-operative course in these patients
References
- Eagle KA, Brundage BH, Chaitman BR et al. Guidelines for perioperative cardiovascular evaluation for noncardiac surgery: report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines: Committee on Perioperative Cardiovascular Evaluation for Noncardiac Surgery. Circulation 2007;116:418–99.
- Hertzer NR, Beven EG, Young JR et al. Coronary artery disease in peripheral vascular patients: a classification of 1000 coronary angiograms and results of surgical management. Ann Surg 1984;199:223–33.
- Mangano DT. Perioperative cardiac morbidity. Anaesthesiology 1990;72:153–84.
- Adams JE III, Bodor GS, Davila-Roman VG et al. Cardiac troponin I. A marker with high specificity for cardiac injury. Circulation 1993;88:101–06.
- Apple FS, Falahati A, Paulsen PR, Miller EA, Sharkey SW. Improved detection of minor ischaemic myocardial injury with measurement of serum cardiac troponin I. Clin Chem 1997;43:2047–51.
- Kim IJ, Martinez FA, Faraday N et al. Cardiac troponin I predicts short-term mortality in vascular surgery patients. Circulation 2002;106:2366–71.
- Landesberg G, Shatz V, Akopnik I et al. Association of cardiac troponin, CK-MB and postoperative myocardial ischaemia with long-term survival after major vascular surgery. J Am Coll Cardiol 2003;42:1547–54.
- Filipovic M, Jeger R, Probst C et al. Heart rate variability and cardiac troponin I are incremental and independent predictors of one-year all-cause mortality after major non-cardiac surgery in patient at risk of coronary artery disease. J Am Coll Cardiol 2003;42:1767–76.
- Oscarsson A, Eintrei C, Anskar S et al. Troponin T-values provide long-term prognosis in elderly patients undergoing non-cardiac surgery. Acta Anaesthesiol Scand 2004;48:1071–9.
- Lopez-Jimenez F, Goldman L, Sacks DB et al. Prognostic value of cardiac troponin T after noncardiac surgery: 6-month follow-up data. J Am Coll Cardiol 1997;29:1241–5.
- Kertai MD, Boersma E, Klein J, Van Urk H, Bax JJ, Poldermans D. Long-term prognostic value of asymptomatic cardiac troponin T elevations in patients after major vascular surgery. Eur J Vasc Endovasc Surg2004;28:59–66.
- Goldman L, Caldera DL, Nussbaum SR et al. Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 1977;297:845–50.
- Devereaux PJ, Goldman L, Yusuf S, Gilbert K, Leslie K, Guyatt GH. Surveillance and prevention of major perioperative ischaemia cardiac events in patients undergoing noncardiac surgery: a review. CMAJ2005;173:779–88.
- Hobbs SD, Yapanis M, Burns PJ, Wilmink AB, Bradbury AW, Adam DJ. Peri-operative myocardial injury in patients undergoing surgery for critical limb ischaemia. Eur J Vasc Endovasc Surg 2005;29:301–04.
- Gibson SC, Marsh A, Berry C et al. Should pre-operative troponin be a standard requirement in patients undergoing major lower extremity amputation? Eur J Vasc Endovasc Surg 2006;31:637–41.
- Eagle KA, Coley CM, Newell JB et al. Combining clinical and thallium data optimizes preoperative assessment of cardiac risk before major vascular surgery. Ann Intern Med 1989;110:859–66.
- Lee TH, Marcantonio ER, Mangione CM et al. Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 1999;100:1043–9.
- Back MR, Schmacht DC, Bowser AN et al. Critical appraisal of cardiac risk stratification before elective vascular surgery. Vasc Endovasc Surg 2003;37:387–97.
- Zethelius B, Johnston N, Venge P. Troponin I as a predictor of coronary heart disease and mortality in 70-year-old men: a community-based cohort study. Circulation 2006;113:1071–8.
- Kavsak PA, Newman AM, Lustig V et al. Long-term health outcomes associated with detectable troponin I concentrations. Clin Chem 2007;53:220–7.
- Ammann P, Fehr T, Minder EI, Gunter C, Bertel O. Elevation of Troponin I in sepsis and septic shock. Intensive Care Medicine 2001;27:965–9.
- Fehr T, Knoflach A, Ammann P, Pei P, Binswanger U. Differential use of cardiac troponin T versus I in haemodialysis patients. Clin Nephrol 2003;59:35–9.
- Musso P, Cox I, Vidano E, Zambon D, Panteghini M. Cardiac troponin elevations in chronic renal failure: prevalence and clinical significance. Clin Biochem 1999;32:125–30.
- Lang K, Schindler S, Forberger C, Stein G, Figulla HR. Cardiac troponins have no prognostic value for acute and chronic cardiac events in asymptomatic patients with end-stage renal failure. Clin Nephrol2001;56:44–51.
- Wallace TW, Abdullah SM, Drazner MH et al. Prevalence and determinants of troponin T elevation in the general population. Circulation 2006;113:1958–65.
- Kertai MD, Boersma E, Westerhout CM et al. A combination of statins and beta-blockers is independently associated with a reduction in the incidence of perioperative mortality and nonfatal myocardial infarction in patients undergoing abdominal aortic aneurysm surgery. Eur J Vasc Endovasc Surg 2004;28:343–52.
