This article is an enlightened approach to reducing strokes in patients with atrial fibrillation (AF). It discusses some freely available software called ‘The Auricle’ and shows how this can easily be used to calculate the annual risk of a stroke. GPs and patients are supported in the careful decision about anticoagulation. To this end the programme has an e-consultation option to ask the opinion of a local cardiologist with the flexibility to attach an electrocardiogram (ECG), echo or clinic letter, if desired. All the details and the cardiologist’s opinion can be electronically filed in the patient’s notes to confirm that the pros and cons of warfarin were fully debated.
Introduction
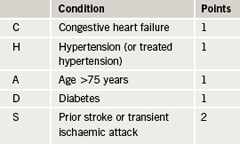
If GPs can be adequately advised and supported in prescribing warfarin to appropriate atrial fibrillation (AF) patients, then we have the potential to save at least 12,500 strokes per year according to the Department of Health. The National Institute for Health and Clinical Excellence (NICE) estimated that 355,000 patients were at high risk of stroke in AF in the UK and that 166,000 of them were not on warfarin (47%). An audit undertaken in Leeds used Read coding queries to apply a CHADS2 score (table 1) to AF patients in participating practices and to identify what thromboprophylaxis was used. The results concorded closely to the NICE estimate. It was found that out of 2,116 patients reviewed with AF, 50% were at high risk of stroke with AF and 46% of those were not on warfarin. Most of these patients were on aspirin. A switch to warfarin therapy for these patients, where possible, would prevent many strokes each year.
The aim is to make a Guidance on Risk Assessment and Stroke Prevention for Atrial Fibrillation (GRASP-AF) audit tool widely available across England to aid GPs in finding patients at risk of stroke and not currently taking warfarin. It has been available via local cardiac and stroke networks from the Heart Improvement Programme website (www.improvement.nhs.uk/heart) since June 2009 (contact: Keith Tyndall, Arrhythmia Nurse on keith.tyndall@nhs.net).
There are many cogent reasons why GPs are reluctant to initiate warfarin. While ignorance among GPs and patients is an obvious possibility, there is disproportionate concern about the prescription and consumption of warfarin. This has to be balanced against an annual stroke risk that can approach 20% in high-risk individuals. Of course prescribing warfarin can indeed rarely be fatal. Every year patients die of bleeds that are iatrogenic but this has an inordinate influence on GPs. It needs to be remembered that the Birmingham Atrial Fibrillation Treatment of the Aged (BAFTA) study showed no significant difference between aspirin and warfarin in both intra-cerebral and extra-cerebral bleeds in elderly patients.
Nevertheless, it is as if Hippocrates is whispering in our ears his law of therapeutics that states: “First do no harm”. We know that the risk of stroke in AF can be reduced by 70% with warfarin and only 20% with aspirin. It is, therefore, surprising how many patients are nonetheless treated with aspirin, potentially leading to thousands of preventable strokes. It is clear that, when prescribing in AF, GPs are between a rock and a hard place. The Quality Outcomes Framework (QOF) incentive scheme does not currently discriminate between warfarin and aspirin in AF, which may lead GPs to think that aspirin is good enough. There are also other significant pressures against warfarin, which include some softer contraindications like risk of falls and, therefore, bleeds.
Professor Greg Lip, Clinical Adviser for the NICE guidelines, quotes the work of Man-Son-Hing et al.1 to calculate that you need 295 falls in a patient to justify not prescribing warfarin! Confusion is another reason offered, if it is felt that accurate compliance with warfarin is at risk.
Methods
‘The Auricle’ has been developed to bring internationally accepted personalised stroke risk information to both patient and GP during the consultation and also to offer consultant cardiologist support electronically, if required. The aim of this project is to reduce the incidence of embolic strokes nationally through the education of both GPs and patients who have AF. ‘The Auricle’ supports complex decision making within the GP consultation in a way that offers novel and effective patient-centred care. One of the Department of Health’s national drivers is the pursuit of greater patient involvement and choice in decision making about their own health. Extending this choice develops patient responsibility through greater awareness of risks and benefits and this will be an immense benefit in AF warfarinisation. GPs often make assumptions about patient preferences and frequently only ask leading questions to determine consent to embark on a particular treatment pathway. Sometimes, undue influence is exerted because of perceived risks – both of the clinical decision itself and an impression of a patient’s attitude to that risk. ‘The Auricle’ method is, therefore, to harness both patients and consultant cardiologists in a drive to increase the prescription of warfarin in AF patients.
AF and its attributable costs consume 1% of the NHS budget (£1 billion). Research quoted above in Leeds led by Dr Campbell Cowan (Consultant Cardiologist and National Clinical Lead for the Heart Improvement Programme) has revealed suboptimal AF management in primary care particularly with regard to the warfarinisation of appropriate cases. Both NICE and CHADS2 are clear about the patients that need warfarin, but successive researchers have found that the proportion of patients that should be warfarinised is lamentably low. Understanding the reasons for this has been illuminating and yet also shone the light on a strategy to radically improve performance and prevent thousands of avoidable strokes. While it is true that there are some real contraindications to warfarin, these are few and far between. Managing risk by informing both GPs and patients about the relative risks of warfarin decisions is the strategy behind ‘The Auricle’. It was vital that the programme should be supportive and not adversarial or dictatorial.

The weighing up of relative contraindications is a delicate matter and it is crucial to have the support of both GP and patient in the evaluation of risk. This is why the electronic link with the local consultant cardiologist was developed. The first dozen cases came from the author’s practice and were emailed to Dr Roger Chatoor, a former cardiologist at Ipswich, who gave invaluable support at the outset. In many cases, GPs need the support of specialists but not necessarily an out-patient appointment. The link to the cardiologist sends the CHADS2 score along with some free text entered by the GP in which relative contraindications can be discussed. The GP can also attach an electrocardiogram (ECG), echo or even a recent clinic letter to this e-consultation. The cardiologist has the option of recommending warfarin, recommending aspirin, suggesting further investigations, e.g. echo, or suggesting an out-patient assessment. Usually the cardiologist recommends warfarin, which is the answer expected. This is not to minimise the importance of this step. At review with the patient after a day or two it can be said that the case has been discussed with a ‘local heart specialist’ and it was agreed that warfarin is appropriate. In the ensuing discussion, the personal risk factors for stroke can be considered and due regard given to the risks of bleeding. The ultimate decision is made by the patient once he or she is fully cognisant of the risks and benefits. The CHADS2 page from ‘The Auricle’ along with the report from the cardiologist is filed electronically in the notes, so it can always be proven that a full and fair discussion took place prior to the patient’s informed decision (figure 1).
Once the idea and clinical needs had been thought through, it was necessary to develop the software. National Health Service (NHS) Innovations East of the East of England Strategic Health Authority (SHA) were approached and supported the software development. It was crucial to launch this strategy for stroke reduction in AF in a blame-free way. The reasons for GP ‘under performance’ needed to be addressed in an understanding and constructive approach. The main reasons are the risk of causing harm with warfarin, as well as not realising just how high the annual stroke risk is. Another significant factor is the difficulty of regular International Normalised Ratio (INR) blood testing along with the risk of patients not taking warfarin as prescribed. Steps to tackle these issues would facilitate appropriate treatment. Near-patient testing is an advance that makes testing easier and convenient, and it can be done at any time of day. It is also a way of reinforcing compliance with treatment and addressing patient concerns at the time of sampling.
Trained warfarin healthcare assistants can operate a home service for the elderly who may find travel to primary care facilities challenging. The subtle benefit of this service is that it makes warfarin much more feasible and appropriate than it was perceived as before. The ‘warfarin service’ is simply set up to be more attractive to both GPs and patients. It was imperative to make the website appealing as well as technically competent. With this in mind, the services of a professional graphic designer (Thumbprint from Luton: art.thumbprint@btconnect.com) were employed to improve the prototype. It was also crucial to both make it easy to use and demonstrate this at the outset. A ‘tutorial’ element was, therefore, prepared, which is a 45 second demonstration showing exactly how to use ‘The Auricle’ that is accessible to all. This was then publicised in the general, as well as professional, media. The tutorial is temporarily hosted on the author’s practice website at www.saxquax.co.uk as well as at www.theauricle.co.uk
Results
Since presentations at Heart and Stroke networks and the AF Consensus Group chaired by Professor Roger Boyle, the National Director for Stroke and Coronary Heart Disease, ‘The Auricle’ has started to be used nationally. While the interest of both cardiologists and GPs is patchy, it is increasing. A trial is ongoing in Bradford with Matt Fay (GP and National Clinical Lead for the Heart Improvement Programme), in which 20 practices are using ‘The Auricle’ and 20 are not, to see if it can make an impact. Various commissioning groups are allocating funding to re-examine their AF patient lists and put these patients through ‘The Auricle’. Further opportunities are provided by this year’s flu clinics. Pulse taking of each patient over 65 can be funded, and confirmed cases of AF can be put through ‘The Auricle’. Work in the author’s practice has resulted in warfarin prescribing increasing by 32%.
Analysis
It is currently too early to analyse the impact of ‘The Auricle’, but it is one of several methods to try to reduce the number of thromboembolic strokes in AF patients. Clearly the first step is to increase appropriate warfarin prescription and then stroke reduction should follow. Raising awareness among both patients and GPs is a complementary strategy achieved through the general accessibility of ‘The Auricle’ both on the dedicated site and YouTube.
Discussion

‘The Auricle’ needs to be promoted and kept up to date. As new research is done the software can be changed, if it is appropriate, without going back to the software designers. One can see that a more sophisticated CHADS2 points system would be easy to accommodate electronically, which might say give 2.3 points for previous stroke and maybe 0.9 for treated hypertension. Public health campaigns to try to identify more asymptomatic patients with AF who are still five times more likely to have strokes are proving effective. This ‘Check your pulse’ poster (figure 2) has been displayed throughout the Commissioning Ideals Alliance group of practices and also in luncheon clubs and residential homes. Nationally, the Arrhythmia Alliance planned a ‘Know your pulse’ campaign during Arrhythmia Awareness Week 8–14 June, and this is the sixth year. In Suffolk Coastal our constituent practices have been supplied with a ‘Heartscan’ machine each, which is a much faster way of making a provisional diagnosis of AF than a formal ECG. Research has shown that intermittent AF occurs in two to three times as many strokes as those admitted with permanent AF. It, therefore, follows that 12,500 strokes a year are the tip of the iceberg since the patients with intermittent AF may currently be classed as sinus rhythm at presentation in hospital and, therefore, be buried within the annual total of strokes with other cardiovascular causes. Another prong to the attack of identifying asymptomatic AF patients is at the sharp end of emergency care, namely the local Ambulance Trust. Incidental diagnoses of AF by front-line staff must not be lost in dealing with the acute problem leading to the emergency. The CHADS2 scoring page from ‘The Auricle’ could be loaded onto ambulance crew laptops so that if a score over 2 is determined then this is emailed directly to the GP. It is then for the GP to confirm the AF and discuss the possibility of warfarin therapy at a subsequent appointment.
The 12,500 Department of Health figure for the number of preventable strokes is difficult to ‘grasp’ in context. However, they also estimate the lives that could be saved by the current multi-million pound national primary percutaneous coronary intervention (PCI) programme to be up to 250. The socio-economic argument may well run that myocardial infarction (MI) patients tend to be younger and more productive, but we need to remember both the absolute numbers and the cost to the country of stroke victim survivors’ ongoing care. As the population gets older the incidence of AF will increase and so, therefore, will the number of attributable strokes unless we change our management nationally.
The real effectiveness of ‘The Auricle’ in stroke prevention will take years to determine. The support of NHS Improvement (under the National Director for Heart and Stroke at the Department of Health, Professor Roger Boyle) bodes well for the future as did winning the NHS Alliance 2008 Acorn Award for Practice-Based Commissioning.
Conflict of interest
None declared.
Key messages
- The Quality Outcomes Framework incentive scheme does not discriminate between aspirin and warfarin in atrial fibrillation
- Warfarin has risks, but these are relatively minimal when compared with the risk of thromboembolic stroke
- Highlighting the annual risk of stroke is a useful way to redress the balance
- ‘The Auricle’ does this while also giving both GPs and their patients the support of a local cardiologist in management decisions
Reference
- Man-Son-Hing M, Nichol G, Lau A, Laupacis A. Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med 1999;159:677–85.
