Postural orthostatic tachycardia syndrome (POTS) is a condition that results from orthostatic intolerance. Patients, frequently young females, present with tachycardia, headache, palpitation, sweating, nausea and near syncope, on changing their posture from lying to standing. It is frequently misdiagnosed as panic attacks or anxiety neurosis. Tilt-table testing is diagnostic. Treatment depends on the type, whether primary or secondary, and there are non-pharmacological and pharmacological options.
Introduction
 Over the last few years, attention has been focused on a relatively new subgroup of disorders referred to as the postural orthostatic tachycardia syndrome (POTS). This syndrome includes a heterogeneous group of disorders that share the same characteristics.1 POTS is characterised by orthostatic symptoms and dramatic increase in heart rate on standing, but does not involve orthostatic hypotension. Tilt-table testing has become the ‘gold standard’ for diagnosing this disorder. In primary care, many patients with POTS may be misdiagnosed as anxiety neurosis, and potential therapeutic opportunities may be missed. In this article, we present and discuss a case with POTS.
Over the last few years, attention has been focused on a relatively new subgroup of disorders referred to as the postural orthostatic tachycardia syndrome (POTS). This syndrome includes a heterogeneous group of disorders that share the same characteristics.1 POTS is characterised by orthostatic symptoms and dramatic increase in heart rate on standing, but does not involve orthostatic hypotension. Tilt-table testing has become the ‘gold standard’ for diagnosing this disorder. In primary care, many patients with POTS may be misdiagnosed as anxiety neurosis, and potential therapeutic opportunities may be missed. In this article, we present and discuss a case with POTS.
History
A 46-year-old woman was referred with a five-year history of episodic headache, palpitation, giddiness, sweating and near syncope. She also complained of intermittent paraesthesia, with or without headache, affecting the four distal limbs. The symptoms were related mainly to standing. There was no vertigo or tinnitus. Six months prior to presentation her symptoms had become intrusive and had led to her losing time from work. Her past medical history includes migraine and pancreatic dysfunction diagnosed a few years ago. One of her sisters has anxiety disorder. She has been using pancreatin, co-dydramol, pantoprazole and diazepam on an as-required basis.
Examination
Supine blood pressure was 120/70 mmHg, with pulse 79 beats per minute, rising to 130/80 mmHg, pulse 84 beats per minute after one minute standing. Cardiovascular, respiratory, abdominal and neurological examinations were all normal. It was felt that this woman’s main symptoms are repeated episodes of palpitation and pre-syncope. The differential diagnoses include arrhythmias, neurocardiogenic syncope, thyrotoxicosis, phaeochromocytoma and carcinoid syndrome.
Investigations
Full blood count (FBC), erythrocyte sedimentation rate (ESR), C-reactive protein (CRP), urea and electrolytes (U&Es), liver function, blood glucose, and thyroid function were all normal. Urinary 5-hydroxyindoleacteic acid (5-HIAA), noradrenaline, adrenaline, metanephrine and dopamine excretion were normal. A 24-hour tape, an echocardiogram and 24-hour blood pressure monitoring were all within normal limits.
An electroencephalograph (EEG), with and without sleep, showed no abnormality. Chest X-ray was normal. Head magnetic resonance imaging (MRI) was also normal. On tilt-table testing the supine blood pressure was 100/88 mmHg with heart rate 88 beats per minute, at 10 minutes of 70 degree up-tilt blood pressure was 104/70 mmHg with heart rate 120 beats per minute. The patient at this moment had palpitations and headache, felt giddy and was sweaty. There was no evidence of cardio-inhibitory or vasodepressor response.
These tilt-table results are diagnostic of POTS, and in her case it is the primary type. She was initially started on conservative measures. There was some improvement and, eventually, she was started on fludrocortisone. Her symptoms were well controlled and she resumed her full-time work.
Discussion
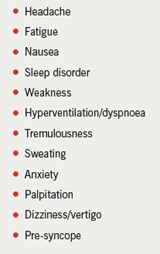
POTS is defined as orthostatic intolerance associated with tachycardia exceeding 120 beats per minute or an increase in the heart rate of 30 beats per minute from baseline within 10 minutes of changing the posture from a lying to standing position, in the absence of long-term chronic diseases and medications that affect the autonomic or vascular tone. There is no drop in blood pressure; it may even rise in the upright posture. Patients experience symptoms such as headache, nausea, tremors, sweating, palpitation and near syncope. Symptoms always occur in the upright posture and disappear on lying down (table 1). POTS was first described in 1940, and it is considered one of the common conditions in young females.2 It occurs most commonly between the ages of 12 and 50 years with a male to female ratio of one:five. Patients with POTS are frequently labelled as having anxiety/neurosis or panic attacks.3 The underlying pathophysiological mechanism is assumed to be failure of peripheral vascular resistance to increase sufficiently in response to orthostatic stress, and, consequently, venous pooling occurs in the legs resulting in decreased venous return to the heart.4,5 This is compensated for by an increase in heart rate and inotropy. POTS is classified as either being primary or secondary (table 2).6 The most common primary form of POTS is called the ‘partial dysautonomic’ form.3,7
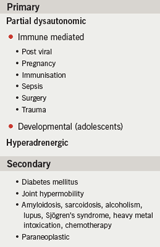
These patients seem to suffer from a mild type of autonomic neuropathy; the peripheral vessels cannot constrict when there is orthostatic stress. In many patients symptoms start abruptly following viral infections, trauma, surgery and after pregnancy. Serum auto-antibodies to alpha-3-acetylcholine receptors of the peripheral ganglia have been detected in some patients with a post-viral presentation. In some cases, there is a hyperadrenergic state8 leading to increased noradrenaline due to impaired clearance or decreased uptake of noradrenaline by the synaptic cleft. These patients suffer from profuse sweating, anxiety, tremulousness, tachycardia and high blood pressure. This variety usually runs in families and is thought to be due to an underlying genetic disorder. The secondary form of the disorder is seen in conditions associated with autonomic neuropathy, e.g. diabetes mellitus or amyloidosis, and in conditions that may be associated with intrinsic abnormalities in capacitance vessels, e.g. hypermobility syndromes. In other conditions the underlying pathogenesis is less clear, e.g. Sjögren’s syndrome.
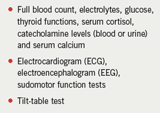
For diagnosis (table 3) FBC, U&Es, glucose, thyroid function tests, serum calcium and electrocardiogram (ECG) should be done for every patient. Serum catecholamines should be checked, in the supine and upright positions, particularly in patients suspected to have the hyperadrenergic form: 24-hour urinary catecholamines is an alternative. Sudomotor function can be checked. Head-up tilt-table study has become the standard provocative test for POTS. In a control population the heart rate increases only 15 beats per minute in the first minute of standing and a further increase for nine minutes. In POTS, supine heart rate is greater than the normal control population and an increase of more than 30 beats per minute or a heart rate >130 beats per minute takes place between 1–10 minutes at 70 degree head uplift.9,10
The differential diagnosis is mainly inappropriate tachycardia syndrome. In this condition, the heart rate increases out of proportion to physical needs due to increased automaticity of the sinus node and blunted cardiac parasympathetic tone, but the symptoms are not related to posture. Chronic fatigue syndrome is another condition that needs to be differentiated from POTS. The US Centers for Disease Control and Prevention (CDC) criteria for diagnosis of this disorder include chronic debilitating fatigue lasting for six months or more, associated with cognitive impairment, pharyngitis, muscle pain, joint pains, headache, sleep disturbance and post-exercise malaise unexplained by any other illness. These patients might have findings similar to POTS during tilt-table testing,11,12 but POTS fails to satisfy the above CDC criteria. POTS may also be wrongly diagnosed as anxiety neurosis because of the similarity of symptoms, but in anxiety neurosis, symptoms are unrelated to posture and tilt-table test is negative as well. Also, in orthostatic hypotension, patients might have symptoms similar to POTS, but in contrast to POTS, symptoms are associated with hypotension. Phaeochromocytoma, another condition that may mimic POTS, can be excluded by measuring plasma or urinary catecholamines.
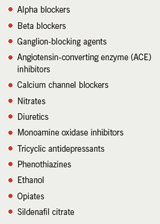
The first step in treating POTS is reviewing and stopping the medications that are known to aggravate the symptoms of POTS (table 4). Non-pharmacological measures should be tried first. Dehydration and excess alcohol should be avoided. Patients are advised to increase their fluid (at least two litres a day) and salt (3–5 grams/day) intake, except those patients diagnosed with the hyperadrenergic form.13 Aerobic exercise of the lower extremities to augment the skeletal muscle pumps may be helpful.14 Patients with dysautonomia may benefit from using compression hose extending up to the waist. If the above measures are not enough, drugs can be used (table 5). Pharmacotherapy depends on the pathophysiology of the syndrome. Patients with dysautonomia may benefit from fludrocortisone, which has been tried with success.15 It causes salt and water retention and sensitises the alpha-adrenergic receptors. The average dose is 50–100 µg/day and the maximum dose is 400 µg/day. If the patient continues to be symptomatic, a serotonin reuptake inhibitor (SSRI),14 or a serotonin and noradrenaline reuptake inhibitor (SNRI) can be added.16 These agents stimulate the standing vasoconstrictor reflex.16 The most commonly used SSRI is fluoxetine 10–20 mg once daily. Of the SNRIs, bupropion 150–300 mg/day is usually used. Venlafaxine 75–150 mg/day also can be useful.
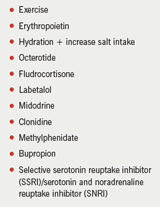
Pyridostigmine, an acetylcholine esterase inhibitor that facilitates neural transmission at the ganglionic level of the sympathetic and parasympathetic nerves, gave good results in POTS secondary to viral infection and autoimmune disorders.17,18 The usual dose is 60 mg orally once daily, either alone or in combination with low-dose propranolol. Pyridostigmine can cause diarrhoea and abdominal cramps.18 If all the above are not effective, erythropoietin is worth trying,19 provided that the haematocrite is less than 50. It causes volume expansion and has a potent direct vasoconstrictor effect. However, it is an expensive medicine and needs continuous monitoring of the haematocrite.19 The dose used in POTS is 800 IU subcutaneously once weekly. It might predispose to stroke. Another option in these cases is octreotide; a potent vasoconstrictor which is given subcutaneously at a dose of 25 µg twice daily, titrated to 100–200 µg three times daily.14 Some patients, particularly, those with partial dysautonomic POTS, improve on small doses of beta blockers (e.g. metoprolol 25–50 mg once or twice daily), but the majority feel worse on beta blockers.20 The hyperadrenergic form of POTS can be treated with sympatholytic agents. One option is clonidine, an alpha2-agonist that acts centrally to decrease sympathetic nervous system tone. The dose is 0.1 mg/day, which can be increased up to 0.2 mg twice daily. It is also available in a ‘patch form’. Unfortunately, it can cause bradycardia, hypotension and mental clouding in some patients.6 The combined alpha1/beta blocker labetalol is useful in some patients, as beta-blockade alone may worsen symptoms due to unopposed alpha-receptor stimulation. A starting dose of 100–200 mg twice daily is used, and the maximum dose is 400 mg twice daily.20 Methyldopa, a false neurotransmitter, may be effective in a dose of 125 mg to 250 mg three times daily.21 SSRIs or SNRIs are also useful in controlling patients’ symptoms. In the secondary forms of POTS, the main aim is to treat the underlying disorder; some patients may improve. Patients with diabetes or joint hypermobility syndrome tend to respond to treatment as do those with the partial dysautonomic form. Those with paraneoplastic POTS may respond to therapy with pyridostigmine, and symptoms often abate with treatment of the malignancy.20
The prognosis of POTS depends on the underlying aetiology. About 50% of patients with post-viral POTS will have partial or complete recovery within two to five years.20 Occasionally, some patients experience deterioration in their daily life activity over time to such an extent that they are unable to continue normal employment or educational activities, and many will become depressed. They often need the help of social workers and psychologists, and legal aid to address the scope of problems brought on by their illness.20 Prognosis is generally better in younger people.20 Ninety per cent of patients will respond to a combination of physical and pharmacotherapy. Patients with hyperadrenergic POTS usually need life-long treatment.22 The prognosis of secondary POTS is related to the prognosis of the underlying disorder.
In conclusion, POTS is a heterogeneous group of disorders with similar clinical
picture. It is underdiagnosed because symptoms mimic vasovagal syndrome and
anxiety neurosis. The tilt-table test is the gold standard for diagnosis, and
treatment depends on identifying the subtype. Patients with severe disabling
symptoms will need a multi-disciplinary approach.
Conflict of interest
None declared.
Key messages
- Postural orthostatic tachycardia syndrome (POTS) is a heterogeneous group of disorders with similar clinical picture
- POTS is underdiagnosed because symptoms mimic vasovagal syndrome and anxiety neurosis
- The tilt-table test is the gold standard for diagnosis
- Treatment depends on identifying the subtype
- Patients with severe disabling symptoms require a multi-disciplinary approach
References
- Grubb BP, Kosinski D, Boehm K, Kip K. The postural tachycardia syndrome: a neuro cardiogenic variant identified during head up tilt table testing. Pacing Clin Electrophysiol 1997;20:2205–12.
- Robertson D, Shannon JR, Biggioni I et al. Orthostatic intolerance and postural tachycardia syndrome: genetic and environmental pathophysiologies. Pflungers Arch 2000;441(2–3 suppl):R48–R51.
- Kanjawal Y, Kosinski D, Grubb BP. The postural tachycardia syndrome: definitions, diagnosis and management. Pacing Clin Electrophysiol 2003;26:1747–57.
- Low PA, Caskey PE, Tuck RR, Fealey RD, Dyckn PJ. Quantitative sundomotor axon reflex test in normal and neuropathic subjects. Ann Neurol 1983;14:573–80.
- Schondorf R, Low PA. Idiopathic postural orthostatic tachycardia syndrome: an attenuated form of acute pandysautonomia. Neurology 1993;43:132–7.
- Grubb BP, Kosinski DJ, Kanjwal Y. Orthostatic hypotension: causes, classification and treatment. Pacing Clin Electrophysiol 2003;26:892–901.
- Karas B, Grubb BP, Boehn K. The postural tachycardia syndrome: a potentially treatable cause of chronic fatigue, exercise intolerance and cognitive impairment. Pacing Clin Electrophysiol 2000;23:344–51.
- Goldstein DS, Eldadah B, Holmes C, Pechnïk S, Moak J, Sharabi Y. Neurocirculatory
abnormalities in chronic orthostatic intolerance. Circulation 2005;111:839–45. - Jacob G, Robertson D, Mosqueda-Garcia R, Ertl AC, Robertson RM, Biaggioni I. Hypovolaemia in syncope and orthostatic intolerance, role of the renin-angiotensin system. Am J Med 1997;103:128–33.
- Furlan R, Jaccob G, Snell M, Robertson D, Porta A, Harris P. Chronic orthostatic intolerance: a disorder with discordant cardiac and vascular sympathetic control. Circulation 1998;98:2154–9.
- Rowe PC, Bon-Holaigah I, Kan JS, Calkins H. Is neurally medicated hypotension an unrecognised cause of chronic fatigue? Lancet 1995;345:623–4.
- Stewart JM, Gewitz MH, Weldon A, Arlievsky N, Li K, Munoz J. Orthostatic intolerance in adolescent chronic fatigue syndrome. Paediatrics 1999;103:116–21.
- Shannon JR, Diedrich A, Biaggioni I, Tank J. Water drinking as a treatment for orthostatic syndromes. Am J Med 2002;112:355–60.
- Grubb BP. Neurocardiogenic syncope and related disorders of orthostatic intolerance. Circulation 2005;111:2997–3006.
- Freitas J, Santos R, Azevedo E, Costa O, Carvalho M, De Freitas A. Clinical improvement in patients with orthostatic intolerance after treatment with bisoprolol and fludrocortisones. Clin Auton Res 2000;10:293–9.
- Schroeder C, Tank J, Boschmann M et al. Selective norepinepherine reuptake inhibition as a human model of orthostatic intolerance. Circulation 2002;105:347–53.
- Raj SR, Black BK, Biaggioni I, Harris PA, Robertson D. Acetylcholinesterase inhibition improves tachycardia in postural tachycardia syndrome. Circulation 2005;111:2734–40.
- Raj SR. The postural tachycardia syndrome (POTS): pathophysiology, diagnosis and management. Indian Pacing Electrophysiol J 2006;6:84–99.
- Grubb BP, Karas B. Preliminary observation on the use of erythropoietin in the treatment of refractory postural tachycardia syndrome. Clin Auton Res 1999;9:228.
- Grubb BP, Kanjwal Y, Kosinski DJ. The postural tachycardia syndrome: a concise guide to diagnosis and management. J Cardiovas Electrophysiol 2006;17:108–12.
- Jacob G, Biaggioni I. Idiopathic orthostatic intolerance and postural tachycardia syndromes. Am J Med Sci 1999;317:88–101.
- Agarwal AK, Garg R, Ritch A, Sarkar P. Postural orthostatic tachycardia syndrome. Postgrad Med J 2007;83:478–80.
