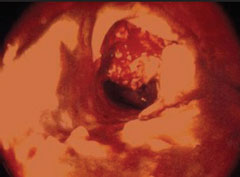
Antithrombotic drugs act principally by inhibiting platelet function directly (for example, aspirin, clopidogrel and dipyridamole) or, via thrombin inhibition, by inhibiting platelet activation and fibrin formation (for example, heparins, warfarin and direct inhibitors of thrombin or factor Xa). Aspirin and other antiplatelet drugs reduce the risk of cardiovascular events such as thrombus formation (figure 1) by approximately 25 per cent in both primary and secondary prevention.(1) Inhibiting more than one pathway at a time significantly increases efficacy: dual antiplatelet therapy with aspirin plus clopidogrel is more effective than aspirin monotherapy in patients with acute coronary syndrome (ACS)(2) and aspirin plus dipyridamole is more effective than aspirin for secondary prevention of stroke.(3) All antiplatelet therapies are associated with an increased risk of bleeding; whereas the balance of benefit and the increased risk of bleeding is clear for secondary prevention, it is less certain for primary prevention.
Mechanisms
The mechanism of action of aspirin differs from that of other antiplatelet agents. Aspirin irreversibly acetylates platelet cyclooxygenase-1 (COX-1), completely inhibiting COX-1- dependent synthesis of thromboxane A2 (TXA2), a substance which is a potent vasoconstrictor and promoter of platelet aggregation. Whether low-dose aspirin also exerts a significant anti-inflammatory effect is uncertain: a retrospective sub-analysis suggested that it was more effective in primary prevention in individuals who had high levels of C-reactive protein (CRP) at baseline4 but it is not known whether low-dose aspirin reduces plasma CRP or other markers of inflammation. A current analysis of the Aspirin in Asymptomatic Atherosclerosis (AAA) study, which serially collected measurements of CRP and other biomarkers in 3,300 participants, should provide more evidence on this question within the next year.
The mechanism of action of dipyridamole is complex but, in summary, it appears to decrease platelet exposure to adenosine diphosphate (ADP) by inhibition of phosphodiesterase in red cells and reduction of ADP release.
Other antiplatelet agents inhibit the interaction between platelets and ADP by blocking the P2Y12 receptor. This membrane G-protein is involved not only in ADP-induced platelet aggregation but also in platelet secretion of pro-thrombotic factors independent of TXA2 (providing a mechanism for synergy with aspirin), stabilisation of platelet aggregates induced by thrombin, and inhibition of shear-induced aggregation. Ticlopidine, the first agent in this thienopyridine class, is associated with bone marrow toxicity and has been replaced by clopidogrel. Both are prodrugs, requiring biotransformation to metabolites that block P2Y12 receptors irreversibly. Clinical limitations include a delayed onset of action (though this is reduced by a loading dose of clopidogrel in patients with ACS) and a variable clinical response due to interindividual differences in metabolism of the prodrugs. Further, prolonged inhibition of platelet function increases the risk of bleeding in patients who subsequently undergo coronary intervention or peripheral arterial bypass grafting.
Newer agents have been developed to overcome these limitations. Prasugrel, another thienopyridine, has a faster onset of action than clopidogrel. The Trial to assess improvement in therapeutic outcomes by optimizing platelet inhibition with prasugrel—thrombolysis in myocardial infarction (TRITON-TIMI 38), which included high-risk patients with ACS requiring percutaneous coronary intervention, showed that prasugrel reduced ischaemic events, though at the cost of a higher risk of major and fatal bleeding complications.5 A further study is now underway which may identify a patient group at lower risk of bleeding: Targeted platelet inhibition to clarify the optimal strategy to medically manage acute coronary syndromes (TRILOGY-ACS) involves patients with ACS for whom no revascularisation is planned (www.trilogyacstrial.org).
New ADP antagonists include direct antagonists of the P2Y12 receptor such as cangrelor (administered intravenously) and ticagrelor (orally). These agents are now undergoing clinical trials to compare them with clopidogrel in patients with ACS. Other newer antiplatelet agents include glycoprotein GP IIb/IIIa antagonists such as the monoclonal antibody abciximab, currently used to treat high-risk patients with ACS. Abciximab is administered intravenously; oral GP IIb/IIIa antagonists have not proved clinically useful.
Anticoagulants
These agents are usually considered to act by inhibiting fibrin formation but, because they primarily inhibit thrombin formation, they also reduce platelet activation. Heparins act indirectly by catalysing the actions of antithrombin: this is a natural coagulation inhibitor that inhibits not only thrombin but also factors Xa, IXa and XIa. Orally active vitamin K antagonists such as warfarin also act indirectly, by reducing hepatic synthesis of factors II, VII, IX and X. These agents have been in clinical use for many years; they remain valuable therapies for the prevention and treatment of venous thromboembolism, and low molecular weight heparins have an established role in the management of ACS. In acute stroke the benefit of heparins is outweighed by the risk of major bleeding episodes except in patients who are at high risk due, for example, to a history of deep vein thrombosis or pulmonary embolism. The commonest indication for oral anticoagulants is reduction of stroke risk in high-risk patients with atrial fibrillation.
The clinical limitations of heparin and warfarin include inter-individual variability in coagulation inhibition (caused by genes, age, weight, diet, and interactions with other drugs) and intra-individual variability arising from pregnancy, impaired renal function and changes in diet and medication. As a result, it is necessary to monitor coagulation during warfarin therapy and sometimes to monitor renal function during treatment with heparin. Both agents cause increased bleeding, and much clinical time is devoted to manipulating anticoagulant therapy to reduce the risk of bleeding during surgery.
Fondaparinux, a parenteral direct factor Xa inhibitor introduced a few years ago, is used for the prevention of venous thrombosis and has shown encouraging results in the management of patients with ACS. There is great interest in new orally active agents such as the direct thrombin inhibitor dabigatran and the factor Xa inhibitor rivaroxaban. These are, by contrast with warfarin, effective in fixed doses and their anticoagulant effects do not need to be monitored. In the UK, they are licensed for prophylaxis of deep vein thrombosis in patients undergoing orthopaedic surgery and they are currently being evaluated in patients with atrial fibrillation. The recent Randomized evaluation of long-term anticoagulation therapy (RE-LY) study showed that dabigatran was non-inferior to warfarin in patients with atrial fibrillation, with greater safety at low doses.6
Conflict of interest
GL currently holds a University of Glasgow contract with Bayer as a member of a Drug Safety and Monitoring Committee for the MAGELLAN trial.
References
- Antithrombotic Trialists’ (ATT) Collaboration. Aspirin in the primary and secondary prevention of vascular disease: collaborative meta-analysis of individual participant data from randomised trials. Lancet 2009;373:1849–60.
- The CURE Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med 2001;345:494–502.
- Diener HC, Cunha L, Forbes C et al. European Stroke Prevention Study. 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. Neurol Sci 1996;143:1–13.
- Ridker PM, Cushman M, Stampfer MJ et al. Inflammation, aspirin, and the risk of cardiovascular disease in apparently healthy men. N Engl J Med 1997;336:973–9.
- Wiviott SD, Braunwald E, McCabe CH et al; TRITON-TIMI 38 Investigators. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med 2007;357:2001–15.
- Connolly SJ, Ezekowitz MD, Yusuf S et al; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med 2009;361:1139–51.
