Diabetic nephropathy is estimated to affect up to 40% of patients with type 2 diabetes. Diabetic nephropathy is characterised by proteinuria, hypertension, progressive decline in renal function and increased mortality (up to 12% per year in patients with increased creatinine levels).
Renal disease and diabetes
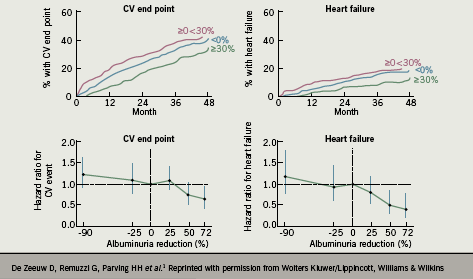
Microalbuminuria is known to be a marker of increased cardiovascular (CV) risk. It is not clear whether reducing microalbuminuria on its own is associated with an improved cardiovascular prognosis, but in secondary analyses from studies of angiotensin receptor blockers (ARBs) in people with type 2 diabetes, reduction in albuminuria was associated with a decreased risk of a CV event. Observational analyses from the RENAAL trial found that the magnitude of albuminuria reduction predicted the reduced risk of CV events (figure 1).1
Generally, treatment of risk factors such as hypertension will also reduce albuminuria.2 A strategy of targeting treatment specifically to albuminuria has not been tested prospectively in patients with diabetes, but interventions that reduce albuminuria or delay its increase (such as use of ARBs, even in conventionally normotensive patients) may prove to be a useful therapy for diabetic kidney disease.
RAAS inhibition and diabetic nephropathy
Many studies have documented the beneficial effects of both angiotensin-converting enzyme inhibitors (ACE inhibitors)3, 4 and ARBs5–7 on renal function, showing benefits beyond those of simply blood pressure control. Most studies of ARBs have used either irbesartan or losartan. In a comparison of the calcium channel blocker (CCB) amlodipine versus irbesartan, results from Lewis et al. showed that irbesartan was associated with a risk of the primary composite end point (defined as a doubling of the baseline serum creatinine concentration, the onset of end-stage renal disease, or death from any cause) 20% lower than that in the placebo group (p=0.02) and 23% lower than that in the amlodipine group (p=0.006), with this effect considered to be independent of effect on blood pressure lowering.7 Mogensen et al. also compared the effects of an ACE inhibitor and an ARB, by assessing the efficacy of lisinopril, candesartan or both on blood pressure and urinary albumin excretion in 199 patients with hypertension, microalbuminuria and type 2 diabetes. The study found that candesartan 16 mg once daily was as effective as lisinopril 20 mg once daily in reducing blood pressure and microalbuminuria in hypertensive patients with type 2 diabetes. Combination treatment was well tolerated and more effective in reducing blood pressure than either drug alone and it also reduced the urinary albumin:creatinine ratio to a greater extent than either drug alone.8 In a direct comparison of the ARBs telmisartan and losartan in the AMADEO study,9 telmisartan was shown to be superior to losartan in reducing proteinuria in hypertensive patients with diabetic nephropathy, despite a similar reduction in blood pressure.
In an attempt to consolidate the individual study results, a meta-analysis by Kunz et al. analysed 49 studies involving 6,181 participants, which reported the results of 72 comparisons comprising ARBs versus placebo, ACE inhibitors, CCBs, or the combination of ARBs and ACE inhibitors in patients with microalbuminuria or proteinuria (from whatever cause) with or without diabetes. The ARBs and ACE inhibitors were found to reduce proteinuria to a similar degree, with the combination of ARBs and ACE inhibitors reducing proteinuria more than either agent alone. However, the limitations to this research were that most studies were small, varied in quality, and did not provide reliable data on adverse drug reactions so the effect of combination therapy on the adverse event profile could not be evaluated.10
Conclusions
In conclusion, there are numerous agents available to block the RAAS and improve the outcome for patients with diabetic nephropathy. Multiple studies have examined the effect of different ACE inhibitors and ARBs, either as monotherapy or in combination, and have demonstrated the effectiveness of both classes of agents in lowering blood pressure and reducing both cardiovascular mortality and morbidity in various at-risk patient populations, including patients with type 2 diabetes. Current UK guidelines recommend treatment with an ACE inhibitor, or with an ARB if the ACE inhibitor is not tolerated.11 In general, the randomised clinical trials in patients with diabetic nephropathy have used losartan or irbesartan: both are licensed for use in patients with hypertension and type 2 diabetic nephropathy. However, the recent AMADEO study has also shown telmisartan to have efficacy in this area.
Conflict of interest
MTK received an honorarium from Takeda for his contribution to this supplement.
Key messages
- Increased proteinuria is associated with increased cardiovascular mortality and morbidity, and therefore identifies patients at high risk who should be targeted for effective reduction of cardiovascular risk factors
- Treatment of cardiovascular risk factors such as hypertension and hypercholesterolaemia has a positive effect on the development and progression of renal dysfunction
- Losartan and irbesartan have been shown to slow the progression of renal disease
References
- de Zeeuw D, Remuzzi G, Parving HH et al. Albuminuria, a therapeutic target for cardiovascular protection in type 2 diabetic patients with nephropathy. Circulation 2004;110(8):921–7.
- de Zeeuw D, Remuzzi G, Parving HH et al. Proteinuria, a target for renoprotection in patients with type 2 diabetic nephropathy: lessons from RENAAL. Kidney Internat 2004;65(6):2309–20.
- Lewis EJ, Hunsicker LG, Bain RP, Rohde RD. The effect of angiotensin-converting-enzyme inhibition on diabetic nephropathy. The Collaborative Study Group. N Engl J Med 1993;329(20):1456–62.
- The GISEN Group (Gruppo Italiano di Studi Epidemiologici in Nefrologia) [No authors listed]. Randomised placebo-controlled trial of effect of ramipril on decline in glomerular filtration rate and risk of terminal renal failure in proteinuric, non-diabetic nephropathy. Lancet 1997;349(9069):1857–63.
- Parving HH, Lehnert H, Bröchner-Mortensen J, Gomis R, Andersen S, Arner P (Irbesartan in Patients with Type 2 Diabetes and Microalbuminuria Study Group). The effect of irbesartan on the development of diabetic nephropathy in patients with type 2 diabetes. N Engl J Med 2001;345(12):870–8.
- Brenner BM, Cooper ME, de Zeeuw D et al. (RENAAL Study Investigators). Effects of losartan on renal and cardiovascular outcomes in patients with type 2 diabetes and nephropathy. N Engl J Med 2001;345(12):861–9.
- Lewis EJ, Hunsicker LG, Clarke WR et al. (Collaborative Study Group). Renoprotective effect of the angiotensin-receptor antagonist irbesartan in patients with nephropathy due to type 2 diabetes. N Engl J Med 2001;345(12):851–60.
- Mogensen CE, Neldam S, Tikkanen I et al. Randomised controlled trial of dual blockade of renin-angiotensin system in patients with hypertension, microalbuminuria, and non-insulin dependent diabetes: the candesartan and lisinopril microalbuminuria (CALM) study. BMJ 2000;321(7274):1440–4.
- Bakris G, Burgess E, Weir M, Davidai G, Koval S on behalf of the AMADEO Study Investigators. Telmisartan is more effective than losartan in reducing proteinuria in patients with diabetic nephropathy. Kidney Internat 2008; 74:364–9; doi:10.1038/ki.2008.204; published online 21 May 2008.
- Kunz R, Friedrich C, Wolbers M, Mann JF. Meta-analysis: effect of monotherapy and combination therapy with inhibitors of the renin angiotensin system on proteinuria in renal disease. Ann Intern Med 2008;148(1):30–48.
- NICE clinical guideline 73. Chronic kidney disease: early identification and management of chronic kidney disease in adults in primary and secondary care. September 2008.
