Low-dose aspirin is of value in the long-term management of vascular disease, and the giving of aspirin to patients believed to be experiencing an acute myocardial infarction (AMI) is standard practice for paramedics and doctors in most countries. Given during infarction, aspirin may disaggregate platelet microthrombi and may reduce the size of a developing thrombus. Effects of aspirin other than on platelets have also been suggested and these include an increase in the permeability of a fibrin clot and an enhancement of clot lysis. Animal experiments have also shown a direct effect of aspirin upon the myocardium with a reduction in the incidence of ventricular fibrillation.
Randomised trials have shown that the earlier aspirin is taken by patients with myocardial infarction, the greater the reduction in deaths. We suggest, therefore, that patients known to be at risk of an AMI, including older people, should be advised to carry a few tablets of soluble aspirin at all times, and chew and swallow a tablet immediately, if they experience severe chest pain.
Introduction
 Aspirin, used in vascular disease prophylaxis, is probably the most cost-effective drug available in clinical practice and daily low-dose aspirin is now a standard item in the long-term management of vascular disease. Within a public health context, the provision of aspirin to individuals at increased vascular risk has been judged to be the preventive activity of greatest benefit and at the lowest cost (by far), apart from smoking cessation.1 Patients with known vascular disease are clearly at increased vascular risk, and a recent US Task Force judged that ‘individuals at increased risk’ includes males aged over about 45 and females over about 55 years,2 and the conclusions in two reports based on UK populations are in close agreement.3,4
Aspirin, used in vascular disease prophylaxis, is probably the most cost-effective drug available in clinical practice and daily low-dose aspirin is now a standard item in the long-term management of vascular disease. Within a public health context, the provision of aspirin to individuals at increased vascular risk has been judged to be the preventive activity of greatest benefit and at the lowest cost (by far), apart from smoking cessation.1 Patients with known vascular disease are clearly at increased vascular risk, and a recent US Task Force judged that ‘individuals at increased risk’ includes males aged over about 45 and females over about 55 years,2 and the conclusions in two reports based on UK populations are in close agreement.3,4
In the acute situation, the giving of aspirin to a patient believed to be experiencing an acute myocardial infarction (AMI) is standard practice.5,6 In what follows, the evidence of benefit from early aspirin is examined and we consider the possible additional benefits if patients at increased vascular risk, including older people, were advised to carry their own aspirin, and chew and swallow an ‘adult’ (300 mg) tablet immediately they experience symptoms suggestive of AMI – the aspirin to be taken even as they summon help.
The clinical problem
Evidence on deaths during the very early stage of a vascular event is limited. Goldstein et al.7 examined the records for 270 witnessed cardiovascular deaths in patients involved in a randomised trial. About a quarter of the deaths had been ‘instantaneous’ (collapse without any symptoms) and, in such cases, cardiopulmonary resuscitation (CPR) is the only appropriate intervention. A further 16% of deaths occurred during the first hour after the commencement of symptoms. From details of a number of studies Gersh and Anderson8 estimated that the typical delay between the commencement of symptoms and hospital treatment was around 96 minutes, and, in an intervention study,9 the out-of-hospital delay for over half the patients with acute AMI was found to be up to two hours.
There has been a sustained drive for earlier treatment of patients with a vascular event, and in most countries paramedics now give aspirin immediately on first contact with a patient who is experiencing severe chest pain and is judged to have possibly had a myocardial infarct or ischaemia.5,6 The UK Department of Health have established a target requiring that at least 75% of patients with chest pain should be attended within eight minutes of a call for an ambulance, and most paramedics are now exceeding this target.10 There is, however, relatively little evidence on the time between the onset of symptoms and the first medical contact (FMC). In Finland, a study found that this interval averaged about 60 minutes regardless of whether or not the patient had a pre-existing history of heart disease.11 A cross-European study estimated that the median FMC in the UK is 68 minutes, but in other European countries the median delay was around 150–200 minutes.12 It seems, therefore, that the opportunity is widespread for what could be termed ‘immediate’ aspirin, that is, aspirin taken while medical help is awaited.
Evidence of benefit
Unfortunately, the reports of randomised trials give no evidence on the effect of aspirin during the first few minutes after symptoms of infarction commence. In the Second International Study of Infarct Survival (ISIS-2), the reduction in deaths by aspirin during the first four hours after the onset of symptoms was 53 ± 8%, compared with 32 ± 9% during the period five to eight hours.13 In the Chinese Acute Stroke Trial (CAST) study of stroke reduction by aspirin, the reduction in deaths by aspirin given within three hours was 36 ± 18%, while in those given aspirin later the reduction was at most 15%.14
Indirect evidence of possible benefit from early aspirin comes from a reduction in the severity of infarction in patients who had developed an infarct while taking aspirin. Col et al.15 found that after adjustment for possible confounding by age, gender, coronary history and medication, “prior aspirin consumption remained independently associated with … non-Q wave and smaller infarct size”. In a series of hospital admissions Garcia-Dorado et al.16 judged that “aspirin … converts 50% of potential AMIs to unstable angina and 20% of Q-wave infarctions to non-Q-wave lesions”. On the other hand, Ridker et al.17 failed to confirm this in the US Physicians study, but conceded that “aspirin therapy may result in a shift of fatal events to severe non-fatal events, severe events to mild events and mild events to no events”.
Possible benefit during infarction
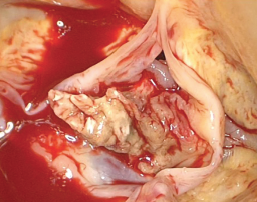
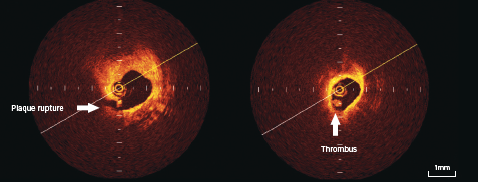
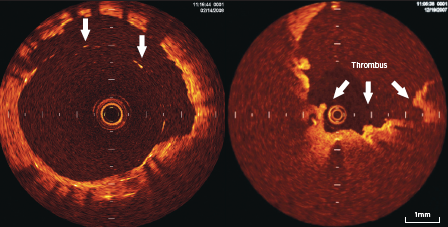
A number of authors have reported finding platelet microemboli within the coronary microcirculation in persons whose death had been ‘sudden’.18,19 In some cases no thrombus could be found in a major coronary vessel, suggesting that microthrombi had developed spontaneously, while in others, microthrombi were additional to a thrombus in a major vessel,20,21 suggesting that fragments from a developing thrombus may have become embolic, or a release action by platelets within a major thrombus may have induced platelet activity within peripheral vessels in the myocardium.21 Platelet aggregates are transient before fibrin is incorporated and early aspirin could, therefore, cause disaggregation of these microemboli, in addition to decreasing thrombus growth and clot volume.22,23
The main mode of action of prophylactic aspirin in vascular disease appears to be through a reduction in platelet aggregation inhibiting the development of a stable thrombus. Measures of platelet aggregation, however, appear to have no predictive power for ischaemic heart disease events.24-26 Effects of aspirin on mechanisms other than platelet aggregation are, therefore, of interest and an action of aspirin on some of them could be of particular importance during the very early processes of thrombosis and infarction.
Aspirin has been shown to acetylate lysine residues in fibrinogen, thus increasing fibrin clot permeability and enhancing clot lysis.27 It also reduces the fibrin mass in a thrombus and leads to a shorter lysis time.28,29 Blood from cigarette smokers has been shown to generate in vitro thrombi that are twice the volume of those in blood from non-smokers, while the ingestion of aspirin by smokers reduced the subsequent thrombus volume to a substantially greater degree (by 62%) compared with the reduction (38%) caused in non-smokers.30 Clearly, the earlier aspirin is taken during thrombosis, and particularly by smokers, the more important these non-platelet effects are likely to be.
A direct effect of aspirin on the myocardium and an anti-arrhythmic effect independent of any action on platelets have also been suggested.31 Moschos et al.32 describe how the occlusion of a coronary artery of a dog by mechanical means can lead to ventricular fibrillation without evidence of any platelet involvement. Fibrillation in these dogs is prevented by aspirin, leading the authors to postulate a direct effect of aspirin upon the myocardium.
Finally, myocardial ischaemia causes a marked increase in catecholamine release and this in turn leads to an increase in free fatty acids,32 a rise which is abolished by aspirin.33 Aspirin may also reduce the vasoconstriction caused by catecholamines34 and by thromboxane A2,35-37 and it reduces catecholamine-induced myocardial necrosis.38 The inhibitory action of aspirin on catecholamines within the myocardium may be the basis for the reduction of arrhythmia during ischaemia.32
The absorption of aspirin
 The absorption of aspirin has been studied extensively. The drug in soluble and dispersible tablets is absorbed much more rapidly than from the standard tablet. Muir et al.39 reported that five minutes after ingestion of a soluble form, the levels of aspirin in the plasma were about 15 times the level after ingestion of the same dose in a plain tablet. Feldman40 found a 50% inhibition of thromboxane A2 within five minutes after a 325 mg tablet is chewed and swallowed.
The absorption of aspirin has been studied extensively. The drug in soluble and dispersible tablets is absorbed much more rapidly than from the standard tablet. Muir et al.39 reported that five minutes after ingestion of a soluble form, the levels of aspirin in the plasma were about 15 times the level after ingestion of the same dose in a plain tablet. Feldman40 found a 50% inhibition of thromboxane A2 within five minutes after a 325 mg tablet is chewed and swallowed.
There is uncertainty about the dose of aspirin that is appropriate if the drug is taken during infarction. Dabaghi et al.36 reported almost complete (97%) inhibition of aggregation to arachidonic acid 15 minutes after ingesting an 81 mg soluble tablet of aspirin and others have reported similar rapid inhibition of plasma thromboxane,35-37 and platelet thromboxane A240 after small doses of aspirin. There is evidence, however, that absorption can be impaired during the acute phase of infarction41 and a relatively high dose may be advisable.42 Yet in an examination of data from recent randomised trials, there was no difference in the very early mortality following initial doses of 162 mg and 325 mg aspirin, but there was a slightly greater incidence of bleeding after the larger dose.43
Further to all this, most patients with an infarct are likely to receive thrombolytic therapy. There is a marked heightening of platelet activity after thrombolysis,39,44 and prior treatment with aspirin abolishes the excess in re-infarction that otherwise follows fibrinolysis.13 In order to achieve fibrinolysis as early as possible, treatment has been delegated to paramedics, although increasingly where percutaneous coronary intervention (PCI) is available in a timely manner, this has become the preferred intervention. Self-administration of aspirin by a subject at the time of calling an ambulance would, however, be appropriate whatever the subsequent interventions.
Strategy
The administration of aspirin as early as possible during the process of thrombosis and infarction, and, hence, the effectiveness of the drug would be enhanced if patients judged to be at risk carried a few ‘adult’ (300 mg) tablets of aspirin at all times, and were instructed to chew and swallow a tablet immediately they experience symptoms suggestive of infarction. Patients to whom this is recommended should include all those known to be at increased vascular risk, and this should include older persons – perhaps those over the age of about 45 or 50 years.2-4
The peak incidence of AMI is in the early morning45 and patients may be more hesitant about calling for help in those early hours. Platelets appear to be most sensitive to aggregating agents in the early morning,46 and in the US Physicians Health Study it was found that the reduction in AMI by aspirin was significantly greater for the events that occurred in the early morning (59%), than for those that occurred later in the day (34%).45 The taking of aspirin by persons themselves could, therefore, be particularly appropriate at these times.
Areas of uncertainty
Around 30% of patients presenting with an AMI are known to already have coronary disease,47 and these are likely to be on daily low-dose aspirin. Others, such as patients on a statin or an antihypertensive agent, are known to be at high risk of a thrombotic event and a high proportion of these are also likely to be on aspirin. There is evidence, however, that many of these, perhaps even around half such patients, are not actually taking the drug.48 In any case, the half-life of aspirin in the circulation is only 15–20 minutes,49 and it would seem reasonable to surmise that if a thrombus develops despite daily exposure to aspirin, some fresh sensitive platelets are likely to have entered the circulation. If this is the case, an extra dose, say 300 or 600 mg of aspirin, taken in addition to the small daily dose, could be life saving.50
Aspirin has undesirable side effects, and persons advised about the benefits of aspirin should also be told the risks. These include increased risks of gastric haemorrhage and cerebral haemorrhage. Estimates of these extra risks have been derived from randomised trials in which patients take aspirin daily over long periods of time. The risk of death attributable to aspirin in trial patients is at most 4% per year,51,52 and the risk of death from a single dose of aspirin is likely to be very considerably lower than this.
It would be unfortunate, however, if the taking of a tablet by a subject in whom a thrombus is developing, led to delay in the calling of an ambulance, and a consequent delay in the commencement of fibrinolytic treatment.53 Persons informed about aspirin should, therefore, be clearly warned that if rapidly increasing severe chest pain is experienced an ambulance should be called first, and then, without further delay, an aspirin tablet should be chewed and swallowed.
Severe chest pain may arise from a non-cardiac cause. If it is from the voluntary muscles, then aspirin is of course appropriate. The relationship of pleuritic pain to breathing should enable a pulmonary embolus to be readily distinguished. Pain from a bleeding gastric lesion should not be a concern as patients known to have a peptic ulcer, or with current indigestion, should have been warned against taking aspirin at any time, even in an emergency.
Pain from angina on exercise should be easily recognised and not confused with the more severe and unremitting pain of infarction. The most important cardiac causes of chest pain that could cause confusion arise from acute aortic syndromes,54 and in particular dissecting thoracic aorta. These lesions are rare, are usually associated with severe hypertension and the pain has an immediate onset, usually with maximum intensity at the time of onset.55
The question naturally arises as to the advisability of ‘immediate’ aspirin if symptoms suggestive of a stroke are experienced. The two major stroke trials, CAST14 and International Stroke Trial (IST),56 gave evidence suggesting that if aspirin is given early during the acute phase of a stroke, there is an additional reduction in the number of deaths and disabling strokes that is “modest but worthwhile”.57 Nevertheless, if aspirin were taken at the very commencement of symptoms suggestive of a stroke, and if the stroke were a haemorrhagic lesion, then the cerebral bleeding might be increased. Immediate aspirin should not, therefore, be advised if symptoms suggest a stroke.
Guidelines from professional societies
The giving of aspirin by a doctor or a paramedic immediately they have contact with a patient believed to be experiencing an acute AMI, is established practice and is recommended by all the relevant professional bodies. Self-medication in this situation has already been recommended,40,58-61 but appears never to have been actively promoted.
Conclusions and recommendations
About 35% of all deaths are attributed to coronary heart disease each year, that is 36,000 in the UK and almost 900,000 in the USA, and younger patients among these are proportionately more likely to die before reaching hospital.62 The earlier aspirin is taken by these patients, the greater the proportionate survival is likely to be.
Aspirin taken while a thrombosis is growing may limit the size of the thrombus and may enhance thrombolysis, thus limiting the damage to the myocardium and the likelihood of a fatal outcome. Effects of aspirin, other than on platelets, indicate that it may help to preserve myocardial tissue and may also reduce the risk of ventricular fibrillation.
People judged to be at increased vascular risk, including older persons, should, therefore, be advised to carry a few tablets of soluble aspirin at all times, and chew and swallow a tablet immediately they experience sudden severe chest pain. Consideration should also be given to the inclusion of instruction on the risks and benefits of early aspirin to persons trained in CPR.
Aspirin is freely available to the public, but advice of varying quality is being given to the public in newspapers and magazines. In a challenging editorial, Kassirer63 states: “…it [is] essential to identify decisions in which it is especially important to consider patient’s values and to protect such decisions from intrusive external decision making”. We believe that the taking of ‘immediate’ aspirin, as we describe it, is such a decision – provided those advised have been adequately informed of the likely risks and benefits.
Conflict of interest
None declared. The authors declare no vested interest and no special funding for the work described.
Key messages
- Aspirin, used in vascular disease protection, is probably the most cost-effective drug available in clinical practice
- The earlier aspirin is given in coronary thrombosis, the greater the reduction in deaths
- It is also likely that early aspirin will reduce the size and severity of a myocardial infarction and it may reduce the risk of ventricular fibrillation
- It is accepted practice for paramedics to give aspirin to patients for whom an emergency call has been received because of chest pain
- It is suggested that patients at increased vascular risk, including older people, should carry tablets of soluble aspirin at all times, and chew and swallow a tablet immediately they experience severe chest pain
References
1. Kahn R, Robertson RM, Smith R et al. The impact of prevention on reducing the burden of cardiovascular disease. Circulation 2008;118:576–85.
2. Preventive Services Task Force. Aspirin for the prevention of cardiovascular disease: US Preventive Services Task Force Recommendation Statement. Ann Intern Med 2009;150:396–404.
3. Bulugahapitiya U, Siyambalapitiya S, Sithole J et al. Age threshold for vascular prophylaxis by aspirin in patients without diabetes. Heart 2008;94:1429–32.
4. Elwood P, Morgan G, Brown G et al. Aspirin for everyone over 50? BMJ 2005;330:1440–1.
5. McVaney KE, Macht M, Colwell CB, Pons PT. Treatment of suspected cardiac ischemia with aspirin by paramedics in an urban emergency medical services system. Prehosp Emerg Care 2005;9:282–4.
6. Fisher JD, Brown SN, Cooke MW. UK Ambulance Service Clinical Practice Guidelines (2006). Joint Royal Colleges Ambulance Liaison Committee, 2006. Available from: http://www2.warwick.ac.uk/fac/med/research/hsri/emergencycare/prehospitalcare/jrcalcstakeholderwebsite/guidelines [accessed 22 February 2009].
7. Goldstein S, Friedman L, Hutchinson R et al. Timing, mechanism and clinical setting of witnessed deaths in postmyocardial infarction patients. J Am Coll Cardiol 1984;3:1111–17.
8. Gersh BJ, Anderson JL. Thrombolysis and myocardial salvage. Circulation 1993;88:296–306.
9. Hedges JR, Feldman HA, Bittner V et al. Impact of community intervention to reduce patient delay time on use of reperfusion therapy for acute myocardial infarction: rapid action for coronary treatment (REACT) trial. Academic Emergency Medicine 2000;7:862–72.
10. The NHS Information Centre. Ambulance Services England 2007–2008. The Information Centre, June 2008. Available from: http://www.ic.nhs.uk/webfiles/publications/Ambulance%
2007-08/Ambulance%20Bulletin%202007-08%20final%20with%20data%20quality
%20note%2015-12-08.pdf [accessed 12 February 2009].
11. Hirvonen TP, Halinen MO, Kala RA, Olkinuora JT. Delays in thrombolytic therapy for acute myocardial infarction in Finland. Results of a national thrombolytic therapy delay study. Finnish Hospitals’ Thrombolysis Survey Group. Eur Heart J 1998;19:885–92.
12. Widimsky P, Wijns W, Fajadet J et al. Reperfusion therapy for ST elevation acute myocardial infarction in Europe: description of the current situation in 30 countries. Eur Heart J 2010;31:943–57.
13. ISIS-2. Second International Study of Infarct Survival Collaborative Group. Randomised trial of intravenous streptokinase, oral aspirin, both or neither among 17,187 cases of suspected acute myocardial infarction. Lancet 1988;2:349–60.
14. CAST (Chinese Acute Stroke Trial) Collaborative Group. CAST: randomized placebo-controlled trial of early aspirin use in 20,000 patients with acute ischaemic stroke. Lancet 1997;349:1641–9.
15. Col NF, Yasrzbski J, Gore JM et al. Does aspirin consumption affect the presentation or severity of acute myocardial infarction? Arch Int Med 1995;155:1386–9.
16. Garcia-Dorado D, Therous P, Tornos P et al. Previous aspirin use may attenuate the severity of the manifestations of acute ischaemic syndromes. Circulation 1995;92:1743–8.
17. Ridker PM, Manson JE, Buring JE et al. Clinical characteristics of non-fatal myocardial infarction among individuals on prophylactic low-dose aspirin therapy. Circulation 1991;84:708–11.
18. Haerem JW. Platelet aggregates and mural micro-thrombi in the early stages of acute fatal coronary disease. Thromb Res 1974;5:243–9.
19. El-Maraghi N, Genton E. The relevance of platelet and fibrin thromboembolism of the coronary microcirculation with special reference to sudden cardiac death. Circulation 1980;62:936.
20. Frink RJ, Trowbridge JO, Rooney PA. Non-obstructive coronary thrombosis in sudden cardiac death. Am J Cardiol 1978;42:48.
21. Gelman JS, Mehta J. Platelets and prostaglandins in sudden death. Cardiovascular Clinics 1985;15:65–80.
22. Roald HE, Sakariassen KS. Axial dependence of collagen-induced thrombus formation in flowing non-anticoagulated human blood. Anti-platelet drugs impair thrombus growth and increase platelet-collagen adhesion. Thromb Haemostas 1995;73:126–31.
23. Stewart JH, Farrell PC, Dixon M. Reduction of platelet/fibrin deposition in haemodialysers by aspirin administration. Austr and New Zealand J Medicine 1975;5:117–22.
24. Elwood PC, Beswick A, Pickering J et al. Platelet tests in the prediction of myocardial infarction and stroke: evidence from the Caerphilly study. Br J Haematol 2001;113:514–20.
25. Elwood PC, Pickering J, Yarnell J, O’Brien JR, Ben-Shlomo Y, Bath P. Bleeding time, stroke and myocardial infarction: the Caerphilly prospective study. Platelets 2003;14:139–41.
26. Sharp DS, Ben-Shlomo Y, Beswick AD, Andrew ME, Elwood PC. Platelet aggregation in whole blood is a paradoxical predictor of ischaemic stroke: Caerphilly Prospective Study revisited. Platelets 2005;16:320–8.
27. Undas A, Brummel-Ziedins KE, Mann KE et al. Antithrombotic properties of aspirin and resistance to aspirin: beyond strictly antiplatelet actions. Blood 2007;109:2285–92.
28. Williams S, Fatah K, Ivert T et al. The effect of acetylsalicylic on fibrin gel lysis by tissue plasminogen activator. Blood Coagulation and Fibrinolysis 1995;7:718–25.
29. Bjornsson TD, Schneider DE, Berger H. Aspirin acetylates fibrinogen and enhances fibrinolysis. Fibrinolytic effect is independent of changes in plasminogen activator levels. J Pharm Exper Ther 1989;250:154–61.
30. Roald HE, Orvim U, Bakken IJ et al. Modulation of thrombotic responses in moderately stenosed arteries by cigarette smoking and aspirin injestion. Arterioscler Thromb 1994;14:617–21.
31. Hirsh J. Antiplatelet agents: their role in the prevention of sudden death. Ann NY Acad Sci 1982;382:289–304.
32. Moschos CB, Haider B, de la Cruz C et al. Anti-arrhythmic effects of aspirin during non-thrombotic coronary occlusion. Circulation 1978;57:681.
33. Oliver MF. Metabolic causes and prevention of ventricular fibrillation during acute coronary syndromes. Am J Med 2002;112:305–11.
34. Strom EA, Coffman JD. Effect of aspirin on circulatory responses to catecholamines. Arthr Rheumatol 1963;6:689–97.
35. Clarke RJ, Mayo G, Price P, Fitzgerald GA. Suppression of thromboxane A2 but not of systemic prostacyclin by controlled release aspirin. N Engl J Med 1991;325:1137–41.
36. Dabaghi SF, Kamat SG, Payne J et al. Effects of low-dose aspirin on in-vitro platelet aggregation in the early minutes after injestion in normal subjects. Am J Cardiol 1994;74:720–3.
37. Jakubowski JA, Stampfer MJ, Vaillancourt R et al. Cumulative antiplatelet effect of low dose enteric-coated aspirin. Br J Haematol 1985;60:635–42.
38. Hart Gershengorn K. Protection against epinephrine-induced myocardial necrosis by drugs that inhibit platelet aggregation. Am J Cardiol 1972;30:838.
39. Muir N, Nichols JD, Clifford JM, Stillings MR, Hoare RC. The influence of dosing form on aspirin kinetics: implications for acute cardiovascular use. Curr Med Opinion 1997;13:547–53.
40. Feldman M, Cryer B. Aspirin absorption rates and platelet inhibition times with 325mg buffered aspirin tablets chewed or swallowed intact and with buffered aspirin solution. Am J Cardiol 1999;84:404–09.
41. Zhang CL, Wilson KM, Stafford I, Bocher F, Horowitz JD. Absorption kinetics of low-dose aspirin in patients with evolving acute myocardial infarction. Drug Invest 1994;1:169–74.
42. Berglund U, Wallentin L. Persistent inhibition of platelet function during long-term treatment with 75mg acetylsalicylic acid daily in men with unstable coronary artery disease. Eur Heart J 1991;12:428–33.
43. Berger JS, Stebbins A, Granger CB et al. Initial aspirin dose and outcome amongst ST-elevation myocardial infarction patients treated with fibrinolytic therapy. Circulation 2008;117:192–9.
44. Fitzgerald DJ, Catella F, Roy L et al. Marked platelet activation in vivo after intravenous streptokinase in patients with acute myocardial infarction. Circulation 1988;77:142–50.
45. Muller JE, Tofler GH, Stone PH. Circadian variation and triggers of onset of acute cardiovascular disease. Circulation 1989;79:733–43.
46. Ridker PM, Manson JE, Buring JE, Muller JE, Hennekens CH. Circadian variation of acute myocardial infarction and the effect of low-dose aspirin in a randomised trial of physicians. Circulation 1990;82:897–902.
47. Weston CFM, Penny WJ, Julian DG. Guidelines for the early management of patients with myocardial infarction. BMJ 1994;308:767–71.
48. Elwood P, Hughes J, Morgan G, Brown G, Longley M. A survey of aspirin use for vascular prophylaxis in Wales. Quality in Primary Care 2005;13:201–04.
49. Patrono C, Baignet C, Hirsh J et al. Antiplatelet drugs: American College of Chest Physicians evidence-based clinical practice guidelines (8th ed.). Chest 2008;133:199S–233S.
50. Prasad N, Srikanthan VS, Wright A, Dunn FG. Management of suspected myocardial infarction before admission. BMJ 1994;316:353.
51. Pirmohamed M, James S, Meakin S et al. Adverse drug reactions as a cause of admission to hospital: retrospective analysis of 18,820 patients. BMJ 2004;329:15–19.
52. Guise J-M, Mahon SM, Aicken M et al. Aspirin for the prevention of cardiovascular events: a summary of the evidence. Ann Intern Med 2002;136:161–72.
53. Rathmore SS, Curtis JP, Chen J et al. Association of door-to-balloon time and mortality in patients admitted to hospital with ST elevation myocardial infarction: national cohort study. BMJ 2009;338:b1807.
54. Vilacosta I, Aragoncillo P, Canadas V et al. Acute aortic syndromes: a new look at an old conundrum. Heart 2009;95:1130–9.
55. Wooley CF, Sparkes EH, Boudoulas H. Aortic pain. Prog Cardiovascular Dis 1998;40:563–89.
56. IST International Stroke Trial Collaborative Group. A randomised trial of aspirin, subcutaneous heparin, both, or neither among 19,435 patients with acute ischaemic stroke. Lancet 1997;349:1569–81.
57. Kmietowicz Z. Aspirin benefits patients with stroke – but only just. BMJ 1997;314:1646.
58. Brecker SJD. Early aspirin in myocardial infarction. Lancet 1990;335:923.
59. Carpenter AL, Caravalho J. Early public use of aspirin in the face of probable ischaemic chest pain. Lancet 1990;335:486.
60. Norfolk Health. Guidelines for practice procedure with a suspected heart attack. East Norfolk Health Commission, 1996.
61. NHS Executive. The health of the nation: assessing the options: CHD/Stroke. Target effectiveness and cost-effectiveness of interventions to reduce coronary heart disease and stroke mortality. London: Department of Health, 1995.
62. Norris RM on behalf of the UK Heart Attack Study investigators. Sudden cardiac death and acute myocardial infarction in three British health districts: the UK heart attack study. London: British Heart Foundation, 1999.
63. Kassirer JP. Incorporating patients’ preferences into medical decisions. N Engl J Med 1994;330:1895–6.
 The study, published online in the British Medical Journal on June 8, 2010, found that, after accounting for a pre-existing decline in admissions, trends in population size, and seasonal variation in admissions, there was a 2.4% drop in the number of emergency admissions for MI after the smoking ban legislation came into force on July 1, 2007. This equates to 1,200 fewer emergency admissions in the first year after the law came into effect (1,600 including readmissions).
The study, published online in the British Medical Journal on June 8, 2010, found that, after accounting for a pre-existing decline in admissions, trends in population size, and seasonal variation in admissions, there was a 2.4% drop in the number of emergency admissions for MI after the smoking ban legislation came into force on July 1, 2007. This equates to 1,200 fewer emergency admissions in the first year after the law came into effect (1,600 including readmissions). Roche has announced that its new troponin T high sensitive assay (Elecsys®) is the first commercially available troponin T assay to meet recent European Society of Cardiology, American College of Cardiology Foundation, American Heart Association and World Heart Federation recommendations.
Roche has announced that its new troponin T high sensitive assay (Elecsys®) is the first commercially available troponin T assay to meet recent European Society of Cardiology, American College of Cardiology Foundation, American Heart Association and World Heart Federation recommendations.
 Aspirin, used in vascular disease prophylaxis, is probably the most cost-effective drug available in clinical practice and daily low-dose aspirin is now a standard item in the long-term management of vascular disease. Within a public health context, the provision of aspirin to individuals at increased vascular risk has been judged to be the preventive activity of greatest benefit and at the lowest cost (by far), apart from smoking cessation.1 Patients with known vascular disease are clearly at increased vascular risk, and a recent US Task Force judged that ‘individuals at increased risk’ includes males aged over about 45 and females over about 55 years,2 and the conclusions in two reports based on UK populations are in close agreement.3,4
Aspirin, used in vascular disease prophylaxis, is probably the most cost-effective drug available in clinical practice and daily low-dose aspirin is now a standard item in the long-term management of vascular disease. Within a public health context, the provision of aspirin to individuals at increased vascular risk has been judged to be the preventive activity of greatest benefit and at the lowest cost (by far), apart from smoking cessation.1 Patients with known vascular disease are clearly at increased vascular risk, and a recent US Task Force judged that ‘individuals at increased risk’ includes males aged over about 45 and females over about 55 years,2 and the conclusions in two reports based on UK populations are in close agreement.3,4 The absorption of aspirin has been studied extensively. The drug in soluble and dispersible tablets is absorbed much more rapidly than from the standard tablet. Muir et al.39 reported that five minutes after ingestion of a soluble form, the levels of aspirin in the plasma were about 15 times the level after ingestion of the same dose in a plain tablet. Feldman40 found a 50% inhibition of thromboxane A2 within five minutes after a 325 mg tablet is chewed and swallowed.
The absorption of aspirin has been studied extensively. The drug in soluble and dispersible tablets is absorbed much more rapidly than from the standard tablet. Muir et al.39 reported that five minutes after ingestion of a soluble form, the levels of aspirin in the plasma were about 15 times the level after ingestion of the same dose in a plain tablet. Feldman40 found a 50% inhibition of thromboxane A2 within five minutes after a 325 mg tablet is chewed and swallowed.
 The book begins with an understanding of evidence-based decision making. Diagnostic screening and testing are evaluated, and the fundamentals of statistical analyses are explained. The success of this section is the use of examples from within cardiovascular medicine, which even the most casual observer would have familiarity with. Health economics and implementation are also explored, and serve to further contextualise the translation from clinical trial to real world medicine.
The book begins with an understanding of evidence-based decision making. Diagnostic screening and testing are evaluated, and the fundamentals of statistical analyses are explained. The success of this section is the use of examples from within cardiovascular medicine, which even the most casual observer would have familiarity with. Health economics and implementation are also explored, and serve to further contextualise the translation from clinical trial to real world medicine.