He who knows syphilis knows medicine” said Father of Modern Medicine, Sir William Osler, at the turn of the 20th Century. So common was syphilis in days gone by, all physicians were attuned to its myriad clinical presentations. Indeed, the 19th century saw the development of an entire medical subspecialty – syphilology – devoted to the study of the great imitator, Treponema pallidum. But syphilis to many is a disease of old, consigned to the annals of history by infusions of mercury, arsenical magic bullets, and finally dealt a fatal blow by the advent of penicillin. The case report of a contemporary presentation of syphilitic aortitis by Aman et al. (see pages 94−6) presented in this issue is fascinating, but it seems most remarkable as a strange relic, a throwback to an era of medicine past. Or perhaps it is not.
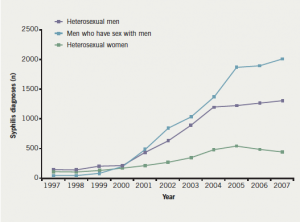
The UK has seen an explosion in venereal syphilis in the first decade of the 21st century. There were 3,762 diagnoses of early stage ‘infectious syphilis’ (comprising primary, secondary and early latent syphilis) made in 2007, more than in any other year since 1950. The trend has continued unabated with a similar figure seen in 2008 (2009 data are awaited). Between 1997 and 2007, annual diagnoses of infectious syphilis rose more than 1,200% (figure 1).(1)
Diagnoses of infectious syphilis declined sharply in the late 1980s and early 1990s, probably as a result of behavioural changes associated with the HIV pandemic. The steady increase in infectious cases since that time has been punctuated by a series of outbreaks, the first of which occurred in 1997 among heterosexuals in Bristol.2 Although outbreaks have occurred in many UK cities, most diagnoses have been reported from Manchester, London and Brighton. The largest outbreak began in London in 2001, and since then infection rates have risen steeply, particularly among men who have sex with men (MSM).
Enhanced surveillance collated by the Health Protection Agency (HPA) since 1999 has demonstrated that the overwhelming majority of diagnoses of infectious syphilis (73%) have occurred in MSM. Among this group, 34% have been HIV co-infected, oral sex has been an important transmission route, and the majority of infections have been acquired within the UK. The heterosexual outbreak was initially confined to imported infections (especially from sub-Saharan and Eastern European countries), commercial sex work and sex parties. In 2008, however, 68% of infections had been acquired within the UK, and patients of white ethnicity are now in the majority
The roots
But where has all this syphilis come from? Undoubtedly, the outbreak observed in MSM (and possibly the heterosexual outbreak) has been influenced by changes in the HIV pandemic in the era of effective antiretroviral therapy. The decline in self-reported condom use observed in the MSM community (‘safer sex fatigue’), increased rates of partner exchange, and the use of new fora (such as the internet) to meet anonymous sex partners have likely fuelled the epidemic. Indeed, the effectiveness of partner notification, a key method of identifying infection within sexual networks, has been compromised because the majority of syphilis cases (76%) have reported mostly anonymous sexual partners. Control and prevention of syphilis to date has been based on increased access to genito-urinary medicine (GUM) services, partner notification, screening initiatives, outreach to at-risk groups, sexual health promotion and antenatal screening. Despite much investment, there has been no marked reduction in incident cases yet observed, and the delivery of effective intervention remains a challenge to be met.
What does this sudden increase of venereal disease mean to the general physician?
Secondary syphilis, a multi-system disorder seen within six months of acquisition of treponemal infection, may persist or recur over weeks or months, and may present to all types of clinician. The number of cases of ‘other acquired syphilis’ reported by GUM clinics to the HPA annually has also risen, albeit less dramatically than that observed in infectious syphilis – from 1,076 cases in 1999, to 1,872 cases in 2007 – constituting a 174% increase (English data only).3 This category comprises cases of late latent syphilis (asymptomatic infections thought to have been acquired more than two years prior to the point of diagnosis) and all cases of tertiary syphilis. This latter subcategory may be subject to under-reporting, as many cases of tertiary syphilis are likely to present to non-GUM physicians and be handled beyond the confines of a GUM service. Data are not available on the clinical types of tertiary syphilis observed.
Data from the pre-antibiotic era (such as the retrospective Oslo Study of Untreated Syphilis of the 1950s) suggests that approximately one-third of all individuals with infectious syphilis will progress towards one or more of the three syndromes of tertiary syphilis, in approximately equal proportions, and after variable incubation periods (typically tens of years).4 Effective antimicrobial chemotherapy with penicillin or tetracyclines will prevent progression towards tertiary syphilis in individuals with latent infection, and may either reverse or prevent progression in established tertiary syndromes (although progression may occur despite therapy). Thus, many individuals with latent disease who are given treponemicidal antimicrobials for coincident reasons may be inadvertently treated for underlying syphilis. One might argue, therefore, that in the antibiotic era, it is unlikely that the general physician will see resurgence in their out-patient clinics of tertiary syphilis, manifest only years after untreated infection. Perhaps not so…
Neurosyphilis refers to any symptomatic infection of the central nervous system (CNS) by Treponema pallidum, and this can occur at any stage of infection – notably during second stage or early latent infection (commonly meningo-vascular disease – strokes, seizures and meningitis – or as brainstem and cranial nerve abnormalities, plus ophthalmic and vestibular involvement), or manifest years later with neurological tertiary syndromes affecting the brain and spinal cord parenchyma (such as tabes dorsalis and general paralysis of the insane). Treponemal invasion of the CNS occurs in up to 25% of individuals during early infection, although this will be self-limiting in the majority.5 An undefined proportion of individuals, however, may present with early neurosyphilis, and it should remain an important differential in young stroke, meningitis, cranial neuropathies, etc., when a sexual risk assessment is undertaken and other clinical features are taken into consideration. There is strong evidence that neurosyphilis at all stages is more common and more symptomatic in HIV-infected individuals, who are disproportionately affected by syphilis infection within the UK, with evidence of increased rates, and persistence of cerebrospinal fluid (CSF) infection after acquisition.6 Progression towards tertiary neurological syndromes appears hyper-accelerated in this group. Syphilis, itself, appears also to have detrimental effects on the natural history of HIV infection. The optimal management of neurosyphilis in the HIV-infected population remains controversial.
Cardiovascular syphilis
What of cardiovascular syphilis? We would anticipate 10% or more of infected individuals to progress to cardiovascular involvement in the pre-antibiotic era. Cardiovascular syphilis almost certainly still exists in the 21st century. In their recent case series, Roberts et al. demonstrated histological evidence of syphilitic aortitis in 90 adults who died between 1966 and 2000, all of whom had morphological features suggestive of syphilitic aortitis at diagnostic autopsy.7 All 90 had extensive involvement of the tubular portion of the ascending aorta by the syphilitic process. The aortic arch was also involved in 49 (91%) of 54 patients and the descending thoracic aorta in 47 (90%) of 52 patients. Syphilitic aortitis was the likely cause of death in 23 (26%) of the 90 patients. The authors argue that this series provides evidence of the ongoing existence of cardiovascular syphilis in the antibiotic era.
Aman et al. provide an in vivo case – with typical clinical features of dilatation of the ascending aorta, aortic root dilatation and aortic valve regurgitation. This case likely reflects an infection acquired in an area of higher endemicity, but the previous negative antenatal testing history suggests an infection of less than 18 years duration, unaffected by intercurrent antibiotic use.
One may suspect that the natural history of cardiovascular syphilis may be accelerated in HIV-positive individuals, given the clinical experience of neurosyphilis to date. There is no published evidence to date to support this, but we suppose this may be due to the relative immaturity of the syphilis epidemic in this population. In the coming years, might we expect an increase in cases of cardiovascular syphilis mirroring that which we are seeing of early stage disease now?
Guidelines
In GUM services, UK guidelines recommend the routine performance of a chest radiograph in all individuals diagnosed with late latent syphilis, with or without evidence of aortic disease.8 Any individual with a radiograph suggestive of aortic disease ought to be referred to a cardiologist for evaluation prior to antimicrobial therapy. Steroid therapy is recommended in cardiovascular syphilis to prevent potential consequences of the Jarisch–Herxheimer reaction. Conversely, UK guidelines for the management of aortic regurgitant valves9 and newly published US guidelines for the management of thoracic aorta disease10 place little (if any) emphasis on the routine testing for syphilis infection in adults presenting with these conditions. In light of the changing epidemiology of this condition, we would strongly argue that serological screening ought to be undertaken in all patients with dilated ascending aortas, with or without aortic regurgitation, and in those with coronary ostial lesions. Screening is sensitive and widely available, and referral to GUM services should be made in all cases with positive serology, for antimicrobial therapy and contact tracing to be undertaken.
Of course, as I hope we have exemplified, the syphilitic may present to any number of healthcare professionals throughout the course of their illness. To that we say: “Physician, beware the great imitator”. And, rightfully, be wary more so now than at any other time in the past 50 years.
Conflict of interest
None declared.
Editors’ note
See also the case report by Aman et al. on pages 94−6 of this issue.
References
- Health Protection Agency. Syphilis and lymphogranuloma venereum: resurgent sexually transmitted infections in the UK. London: HPA, 2009. Available from: http://www.hpa.nhs.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1245581513121 [accessed 30 April 2010].
- Simms I, Fenton KA, Ashton M et al. The re-emergence of syphilis in the UK: the new epidemic phases. Sex Transm Dis 2005;32:220–6.
- Health Protection Agency. STI annual data tables. London: HPA, 2009. Available from: http://www.hpa.nhs.uk/Topics/InfectiousDiseases/InfectionsAZ/STIs/STIsAnnualData/ [accessed 30 April 2010].
- Clark EG, Danbolt N. The Oslo study of the natural history of untreated syphilis; an epidemiologic investigation based on a restudy of the Boeck-Bruusgaard material; a review and appraisal. J Chronic Dis 1955;2:311–44.
- Lukehart SA, Hook EW, Baker-Zander SA et al. Invasion of the central nervous system by
Treponema pallidum: implications
for diagnosis and treatment.
Ann Intern Med 1988;109:855–62. - Zetola NM, Klausner JD. Syphilis and HIV infection: an update. Clin Infect Dis 2007;44:1222–8.
- Roberts WC, Ko JM, Vowels TJ. Natural history of syphilitic aortitis. Am J Cardiol 2009;104:1578–87.
- Kingston M, French P, Goh B et al. UK national guidelines on the management of syphilis 2008. Int J STD & AIDS 2008;19:729–40.
- The Task Force on the Management of Valvular Heart Disease of the European Society of Cardiology. Guidelines on the management of valvular heart disease. Eur Heart J 2007;28:230–68.
- 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guidelines for the diagnosis and management of patients with thoracic aortic disease: executive summary. Circulation 2010;121:1544–79.
