Syphilis is a venereal disease that can also be acquired by exposure to infected blood and body fluids. The organism can cross the placenta and infect the unborn child. Untreated syphilis progresses through four stages: primary, secondary, latent, and tertiary stages. Syphilis is a great imitator; patients with syphilis can be a diagnostic challenge because of their wide-ranging clinical presentations. Although the incidence of syphilis has declined dramatically following the advent of penicillin therapy, it is still prevalent due to unsafe sex, multiple sexual partners and intravenous drug abuse. Primary and secondary syphilis can present with minor symptoms while tertiary syphilis can cause mortality in up to 20% of untreated patients due to neurological and cardiovascular complications.
Case presentation
A 51-year-old woman was referred to our cardiology clinic with palpitations and visible pulsations in her neck. By profession she was a nurse and had been previously fit and well. She moved to Wales from South Africa six years ago. She was a non-smoker with no history of alcohol abuse. She denied any chest pain or shortness of breath and reported excellent exercise tolerance.
Observations showed a blood pressure of 157/66 mmHg, pulse of 86 beats per minute (collapsing in nature), and jugular venous pressure was normal. She had normal first heart sound with an early diastolic murmur. Electrocardiogram (ECG) showed left ventricular (LV) hypertrophy. Echocardiography was performed, which showed moderately reduced LV function with an ejection fraction of 40%, moderate/severe aortic regurgitation with forward gradient across the aortic valve of 35 mmHg. The aortic valve opened well and was not thickened.
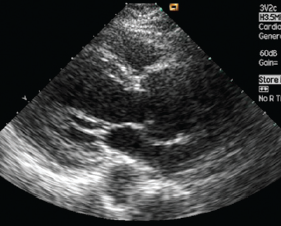
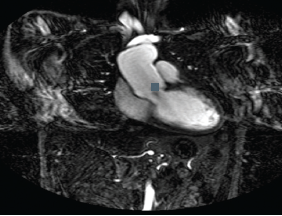
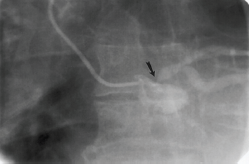
To get more detailed imaging she underwent transoesophageal echocardiography, which showed moderate/severe aortic regurgitation, her aortic root was measured at 4.6 cm with a dilated ascending aorta (figure 1). She also underwent cardiac magnetic resonance imaging (MRI), which showed dilated ascending aorta, maximum diameter of 5.3 cm with normal caliber before the origin of the brachiocephalic trunk (figure 2).
She was started on perindopril and, because of the severe aortic regurgitation and dilated aortic root, it was decided to refer her for surgery. As a work up she had an angiogram, which showed normal coronary arteries. The aortic root was 5.5 cm dilated with severe aortic regurgitation. The LV end systolic diameter was 5.5 cm. All her routine blood tests were essentially normal.
To look into the cause of her aortic regurgitation syphilis serology was performed, which came back positive for syphilis (IgG/M positive on ELISA, negative rapid plasma reagin [RPR]). She was seen by the genito-urinary medicine (GUM) consultant and repeat investigations confirmed IgG/M positive on ELISA, positive Treponema palladium haemagglutination assay (TPHA), and it was advised to start on benzylpenicillin 2.4 g weekly for three weeks with steroid cover prior to the first dose to prevent Jarisch-Herxheimer reaction. This is an inflammatory process that is thought to occur when large quantities of toxins are released into the body, as bacteria die due to antibiotic therapy. Administration of steroids with the first dose is thought to prevent this from happening. The rest of her investigations, including HIV and hepatitis C tests, were negative, although she was positive for hepatitis B virus antibodies due to previous vaccination.
A detailed history was taken for contact tracing. She had multiple sexual partners before marriage in 1982. She was unaware of contracting any kind of sexual disease. Her husband was negative for syphilis. She has four daughters, aged 25, 23, 21 and 18, all healthy. Three of the daughters were born through caesarian section while one was born through normal vaginal delivery. Before each birth she was tested for syphilis, which, according to her, was negative. She could not recall features of primary or secondary syphilis and had never suffered from yaws or pinta.
She underwent surgery and had a mechanical aortic valve and aortic root, ascending aorta and hemi-arch replacement. On follow-up in the cardiology clinic, she seems to have recovered very well from the operation. Histology of the aorta confirmed changes consistent with syphilis.
Discussion
Sir William Osler said “the physician who knows syphilis knows medicine”.1
It is a rare sexually transmitted disease bacterium, Treponema pallidum, but recently its incidence is increasing. Many people do not have any symptoms for years, yet remain at risk for late complications if untreated. Transmission is from persons with sores who are in the primary or secondary stage, however, many of these sores are unrecognised. Thus, most transmission is from persons who are unaware of their infection.
Latent stage can last for 2–20 years, during which patients are asymptomatic. In the tertiary stage there is granuloma formation in the skin, mucosa, joints, bones and rarely viscera (e.g. lung and testes). Cardiovascular manifestations occur 10–30 years after the initial infection. In untreated syphilis, aortitis occurs in 70–80%, which can lead to aortic regurgitation, while coronary ostial stenosis and aortic aneurysms are seen in 10–15% of patients. Aortic regurgitation is rarely caused by syphilis, seen in 20–30% of patients with syphilitic aortitis. Coronary ostial lesions are seen in 20–25% of patients with syphilitic aortitis. It is uncommon for coronary ostial lesions to lead to acute myocardial infarction.
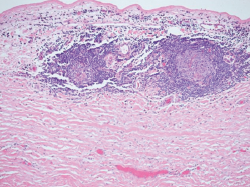
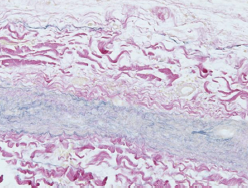
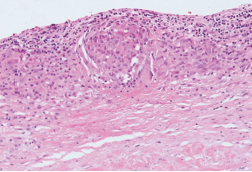
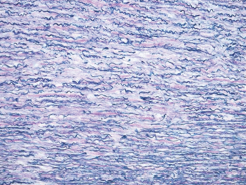
Treponema pallidum invades the vasa vasorum. There are inflammatory changes, perivascular infiltrates of lymphocytes and plasma cells (figure 3). There is endarteritis obliterans, adventitia scarring, and patchy necrosis of media with destruction of elastic fibres (figures 4–6). These changes are common in the proximal and transverse arches, where there is abundant vasa vasorum. There is coronary ostial involvement, which is secondary to scar tissue in the proximal aorta (figure 7).
The duration and route of penicillin therapy is controversial. Penicillin has never been formally evaluated as treatment for cardiovascular syphilis. World Health Organization (WHO), European, UK and US guidelines suggest:1-6
intramuscular benzylpenicillin 2.4 million units once weekly for three weeks. Although definitive evidence of the efficacy of benzathine penicillin is lacking, there is also no evidence to the contrary.
There is little evidence that Jarisch-Herxheimer reactions complicate treatment of cardiovascular syphilis. Alternative regimens are doxycycline or amoxicillin plus probenecid.
Conclusion
Cardiovascular syphilis may occur in patients outside of the usual risk groups for syphilis. Testing for syphilis serology should be considered in patients with aortic regurgitation, and particularly bilateral coronary ostial lesions and/or aortic aneurysms. Long-term sexual partners of patients with late latent or tertiary syphilis should be screened serologically.
Note
There has been a case report published on the same patient in the International Journal of STD and AIDS in March 2010 (Int J STD AIDS 2010;21:222–3) by Gowland P-A, Musleh G, Koukis I and McLaughlin KE, reviewing the case from a different perspective.
Conflict of interest
None declared.
Editors’ note
See also the editorial by Rayment and Sullivan on pages 56−8 of this issue.
References
- Eisenberg H, Brandfonbrener M. Observations on penicillin treated cardiovascular syphilis. I. Uncomplicated aortitis. Am J Syph Gonorrhea Vener Dis 1953;37:439–41.
- Eisenberg H, Brandfonbrener M. Observations on penicillin treated cardiovascular syphilis. II. Complicated aortitis. Am J Syph Gonorrhea Vener Dis 1953;37:442–8.
- World Health Organization Europe. Review of current evidence and comparison of guidelines for effective syphilis treatment in Europe. Geneva: World Health Organization, 2003. Available at: http://www.euro.who.int/document/e81699.pdf [accessed Jan 2006].
- Goh B, van Voorst Vader P. European guideline for the management of syphilis. Int J STD AIDS 2001;12(suppl 3):14–26.
- Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines 2002. M MWR Recomm Rep 2002;51:1–78.
- Mauricio G, Cohen R, Anderson D et al. Syphilitic aortitis. Cathet Cardiovasc Intervent 2001;52:237–9.
