Statins represent the cornerstone of treatment in guidelines for lipid management.1 The clinical benefits have been confirmed by meta-analysis of major prospective studies which showed that statins reduced cardiovascular risk by about one fifth per mmol/L reduction in low-density lipoprotein (LDL) cholesterol, largely irrespective of the initial lipid profile, the presence of diabetes, or other presenting characteristics.2,3 More intensive regimens produced further incremental benefit, compared with conventional-dose statin therapy.4 Among patients at higher risk, such as those with pre-existing coronary heart disease (CHD) or with diabetes, the absolute clinical benefits were greater than in those at lower risk.2 Furthermore, recent long-term follow-up of the Heart Protection Study shows that the cardiovascular benefits of statin therapy accrued as treatment continued and persisted for several years after the trial terminated. These data also provided reassurance that statins are safe, with no increase in cancer incidence or other safety concerns during extended follow-up.5
 Current National Institute for Health and Clinical Excellence (NICE) guidance1 recommends statin treatment for all adults with clinical evidence of cardiovascular disease. In the primary prevention setting, the guidance recommends systematic identification of adults (aged 40–75 years) likely to be at high risk of developing cardiovascular disease. Risk estimation is key to this process. Although preferable to clinical assessment alone, there are some outstanding concerns.
Current National Institute for Health and Clinical Excellence (NICE) guidance1 recommends statin treatment for all adults with clinical evidence of cardiovascular disease. In the primary prevention setting, the guidance recommends systematic identification of adults (aged 40–75 years) likely to be at high risk of developing cardiovascular disease. Risk estimation is key to this process. Although preferable to clinical assessment alone, there are some outstanding concerns.
Improving risk estimation
Framingham-based risk assessment has been widely used and provides reasonable discrimination between individuals at higher or lower risk of cardiovascular disease. However, questions remain regarding its validity in contemporary populations, given differences between the Framingham study population (Caucasian US population) and the UK. For example, studies show that Framingham-based risk estimation can over-predict the absolute risk of cardiovascular disease in lower-risk populations, such as in South-East England.6 Framingham-based risk estimation also does not take account of additional risk factors (table 1) leading to underestimation of risk in certain high-risk groups, such as socioeconomically deprived individuals.7 As a consequence, statin treatment may be less available to those most in need.
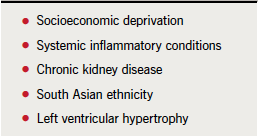
The development of QRISK1 may offer advantages given that it is better validated to the UK population than the Framingham model, and also includes additional variables, which improve risk estimates (such as positive family history of premature cardiovascular disease).8 Therefore, QRISK1 may be a more equitable tool to inform management decisions and help ensure treatments are directed towards those most likely to benefit. Further refinement (QRISK2) offers marginal differences in performance compared with QRISK1.9
One group that has been largely overlooked in risk estimation has been those with severe mental illness. In a recent observational study, such individuals were shown to be at higher risk of cardiovascular death, which is not totally explained by antipsychotic medication, smoking or social deprivation scores. However, it was noted that individuals receiving the highest doses of antipsychotics were at greatest cardiovascular risk.10
Ultimately, it is recognised that there is a continuum for cardiovascular risk, with increasing risk requiring increased intensity of risk factor modification. As a consequence, intervention has been targeted to high-risk groups, in particular those with pre-existing cardiovascular disease and/or diabetes. Building on this concept, implementation of the National Health Service (NHS) Health Checks programme is providing a more comprehensive assessment of individual health as a baseline for deciding the most appropriate actions to reduce cardiovascular risk.11 The programme provides a systematic holistic approach to measuring patients’ risk, rather than assessing individual risk factors.
Evolving recommendations for statin therapy
Current guidance recommendations are based on clinical and cost-effectiveness. In both primary and secondary prevention settings, simvastatin 40 mg is recommended as first-line treatment, although if contraindications or potential drug interactions limit its use, a lower dose or alternative statin, such as pravastatin may be considered.1 People with acute coronary syndromes (ACS) should be treated with a higher-intensity statin.1 Such an approach is supported by evidence from a meta-analysis comparing intensive- and conventional-dose statin therapy in acute ACS patients,12 and evidence that both high-dose simvastatin and atorvastatin were cost-effective.1
Issues arise when considering the best approach in secondary prevention patients (without diabetes) who fail to achieve cholesterol targets (total cholesterol <4 mmol/L or for LDL cholesterol <2 mmol/L) on simvastatin 40 mg monotherapy. Guidelines recommend either titrating the dose of simvastatin to 80 mg or switching to a drug of similar efficacy and acquisition cost.1 Furthermore, in patients with type 2 diabetes, cost-effectiveness analyses indicated that two-step titration (simvastatin 40 mg titrated first to simvastatin 80 mg and then, if indicated, switched to atorvastatin 80 mg) is cost-effective in patients who fail to achieve lipid targets, especially high-risk patients.13 However, it should be borne in mind that these recommendations relate to data available in 2008. New evidence about statins questions this strategy. SEARCH (Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine)14 highlighted an increased risk of myopathy associated with simvastatin 80 mg compared with 20 mg, equating to an excess risk of four per 1,000 person-years during the first year of treatment. As a result, the Medicines and Healthcare products Regulatory Agency (MHRA) issued a warning regarding the use of simvastatin 80 mg.15 Additionally, recommendations for the use of atorvastatin are likely to be revised given that generic atorvastatin will be available in 2012.
Local implementation
From a local perspective, agreeing guidelines for lipid management should involve a partnership between primary and secondary care. To achieve this there needs to be a realistic reconciliation of national guidelines and any new evidence to develop one local guideline, providing a consistent management approach that will benefit patients. Practical barriers to implementation need to be recognised and addressed. Finally, partnership also implies ownership, which is clearly essential to implementation. Local clinical ‘champions’ may assist in this process.
Healthcare systems face a major challenge in achieving cost-effective use of resources to prevent cardiovascular disease. As indicated by guidelines,1 lifestyle modification is an important component of lipid management. Statins are the mainstay of pharmacotherapy; however, in the light of new evidence relating to the efficacy and cost-effectiveness of different statins, revisions of current guidelines are likely. Moreover, statins should not be considered in isolation, as other treatments may offer benefit in managing abnormal lipids associated with the metabolic syndrome (elevated triglycerides and low plasma levels of high-density lipoprotein [HDL] cholesterol). Partnership between secondary and primary care is essential for ensuring successful implementation at the local level.
Key messages
- Emerging evidence highlights the need for timely review of guidelines, taking into account new data on the efficacy, safety and cost-effectiveness of statins in different settings
- Statin therapy should not be recommended in isolation; clinicians also need to take account of lifestyle intervention and other preventive drug treatments
- At the local level, partnership between primary and secondary care ensures successful implementation
References
- National Institute for Health and Clinical Excellence. Lipid modification. Cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease. NICE Clinical guideline 67. London: NICE, May 2008. Available from: http://www.nice.org.uk/nicemedia/pdf/CG67NICEguideline.pdf [accessed 10 January 2012].
- Baigent C, Keech A, Kearney PM et al. Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90 056 participants in 14 randomised trials of statins. Lancet 2005;366:1267–78. http://dx.doi.org/10.1016/S0140-6736(05)67394-1
- Cholesterol Treatment Trialists’ (CTT) Collaborators, Kearney PM, Blackwell L, Collins R et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet 2008;371:117–25. http://dx.doi.org/10.1016/S0140-6736(08)60104-X
- Cholesterol Treatment Trialists’ (CTT) Collaboration, Baigent C, Blackwell L, Emberson J et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet 2010;376:1670–81. http://dx.doi.org/10.1016/S0140-6736(10)61350-5
- Heart Protection Study Collaborative Group, Bulbulia R, Bowman L, Wallendszus K et al. Effects on 11-year mortality and morbidity of lowering LDL cholesterol with simvastatin for about 5 years in 20 536 high-risk individuals: a randomised controlled trial. Lancet 2011;378:2013–20.
- Brindle P, Emberson J, Lampe F et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ 2003;327:1267. http://dx.doi.org/10.1136/bmj.327.7426.1267
- Brindle PM, McConnachie A, Upton MN et al. The accuracy of the Framingham risk-score in different socioeconomic groups: a prospective study. Br J Gen Pract 2005;55:838–45.
- Hippisley-Cox J, Coupland C, Vinogradova Y, Robson J, May M, Brindle P. Derivation and validation of QRISK, a new cardiovascular disease risk score for the United Kingdom: prospective open cohort study. BMJ 2007;335:136. http://dx.doi.org/10.1136/bmj.39261.471806.55
- Collins GS, Altman DG. An independent and external validation of QRISK2 cardiovascular disease risk score: a prospective open cohort study. BMJ 2010;340:c2442. http://dx.doi.org/10.1136/bmj.c2442
- Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom’s General Practice Research Database. Arch Gen Psychiatry 2007;64:242–9. http://dx.doi.org/10.1001/archpsyc.64.2.242
- NHS Health Check identity guidelines. March 2010. Available from: http://www.healthcheck.nhs.uk/Library/292803_HC_guidelines_acc_Mar10.pdf [accessed 24 January 2012].
- Cannon CP, Steinberg BA, Murphy SA, Mega JL, Braunwald E. Meta-analysis of cardiovascular outcomes trials comparing intensive versus moderate statin therapy. J Am Coll Cardiol 2006;48:438–45. http://dx.doi.org/10.1016/j.jacc.2006.04.070
- National Institute for Health and Clinical Excellence. Type 2 diabetes – national clinical guideline for management in primary and secondary care (update). Clinical guidelines CG66. London: NICE, May 2008. Available from: http://www.nice.org.uk/nicemedia/pdf/CG66NICEGuideline.pdf [accessed 4 January 2012].
- Study of the Effectiveness of Additional Reductions in Cholesterol and Homocysteine Collaborative Group. Intensive lowering of LDL cholesterol with 80 mg versus 20 mg simvastatin daily in 12 064 survivors of myocardial infarction: a double-blind randomised trial. Lancet 2010;376:1658–69. http://dx.doi.org/10.1016/S0140-6736(10)60310-8
- Medicines and Healthcare products Regulatory Agency. Simvastatin: increased risk of myopathy at high dose (80 mg). Drug Safety Update 2010;3:7–8.

