Highlights of the European Society of Cardiology (ESC) 2012 Congress held in Munich, Germany on August 25th–29th included the first ever randomised trial addressing the treatment of patients on anticoagulants who receive a stent, and lots more data on the new percutaneous alternatives to valve surgery – TAVI and MitraClip. More from the congress is featured in our podcast at www.bjcardio.co.uk
WOEST: aspirin not required for stent patients on oral anticoagulants
A strategy of using clopidogrel as a single antiplatelet drug for patients receiving a
drug-eluting stent who are also taking an oral anticoagulant appears safe and can reduce bleeding, the results of the WOEST study suggest.
How to treat patients on anticoagulation when they receive a stent is fraught with difficulty as giving the normal dual antiplatelet therapy with aspirin and clopidogrel means they will be taking three anti-clotting agents which could increase bleeding complications to a dangerous level. But no randomised clinical trials have ever investigated whether alternative strategies may be better.
The WOEST study, presented by Dr Willem Dewilde (TweeSteden Hospital, Tilburg, the Netherlands) investigated whether aspirin could be dropped in such patients. It enrolled 573 patients already treated with oral anticoagulants for atrial fibrillation or mechanical valves and undergoing coronary stenting, who were randomised to two groups: one given additional clopidogrel only (double therapy group), or a second given additional clopidogrel and aspirin (triple therapy group).
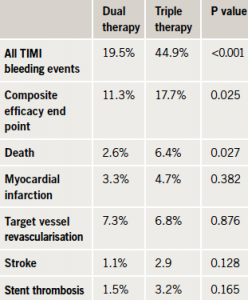
Results (table 1) showed that at one-year follow-up, the dual therapy group had less bleeding (the primary end point) than the triple therapy group. There was a significant reduction in minimal and minor bleeding, and major bleeding was also numerically lower, but this did not reach statistical significance. The trial was not powered to show a difference in ischaemic events, but there did appear to be a reduction in mortality in the dual therapy group, and there was no increase in myocardial infarction or stent thrombosis.
Dr Dewilde commented: “Although the number of patients in the trial is limited, this is an important finding with implications for future treatment and guidelines in this group of patients known to be at high risk of bleeding and thrombotic complications”.
Co-chair of an ESC press conference on the study, Professor Keith Fox (University of Edinburgh) noted that although the trial was small, it was the first randomised data on this issue, and as such could be practice changing. “If we look at the evidence prior to this, there has been very little. So this is a very big step. The community will take this seriously,” he said.
Professor Fox discusses the WOEST study in our ESC podcast
MitraClip looks good for high risk mitral valve patients
Another European registry has shown favourable results for use of the percutaneous MitraClip for mitral valve repair. The clip is delivered by catheter through the femoral vein, and is designed to reduce significant mitral regurgitation by clipping together the leaflets of the mitral valve.
ACCESS-EU, a registry of 567 MitraClip patients from 14 European sites, is the largest group of patients evaluated to date. Patients were elderly (mean age 74) with significant co-morbidities, including coronary artery disease in 63% and moderate to severe renal disease in 42%. At baseline, 85% were in New York Heart Association (NYHA) Class III/IV heart failure, and 53% had left ventricular ejection fraction less than 40%. The majority of patients had functional mitral regurgitation, and were considered at high risk for mitral valve surgery.
Results at one year showed that 82% of patients were still alive, 79% had mitral regurgitation grade 2+ or less, and 94% remained free from mitral valve surgery. The majority of patients showed significant clinical improvements, with 72% now classified in NYHA Class I/II. In addition, results reflected an improved functional capacity, with a median improvement of 60.5 meters for six-minute walk distance, and improvements in quality of life, reported Dr Wolfgang Schillinger (Universitätsmedizin Göttingen, Germany).
He concluded that: “Where the benefits of surgery do not outweigh the risks, the MitraClip treatment is an important alternative for patients with mitral regurgitation.”
The transcatheter aortic-valve implementation (TAVI) and MitraClip percutaneous procedures are both discussed in more detail in the new ESC guidelines on the treatment of valve disease, which were released at the meeting.
TRILOGY ACS: no role for prasugrel in medically treated ACS
The antiplatelet agent, prasugrel, failed to significantly reduce cardiovascular events versus clopidogrel in the TRILOGY ACS trial in high-risk acute coronary syndrome (ACS) patients managed medically without revascularisation.
Study chairman, Dr Magnus Ohman (Duke University Medical Center, Durham, US) noted that TRILOGY was designed to complement the TRITON trial in which prasugrel was associated with significantly lower rates of ischaemic events, versus clopidogrel but with an increased risk of major bleeding in ACS patients undergoing revascularisation. “The aim of TRILOGY was to see if prasugrel was just as effective in ACS patients who weren’t getting stents or bypass surgery,” he said.
The trial randomised 7,243 ACS patients not undergoing revascularisation to prasugrel (10 mg daily reduced to 5 mg for patients under 60 kg) or clopidogrel (75 mg daily) for up to 30 months of treatment. The primary end point – cardiovascular death, myocardial infarction, or stroke through a median follow-up period of 17 months – was not significantly different between the two groups (table 1).
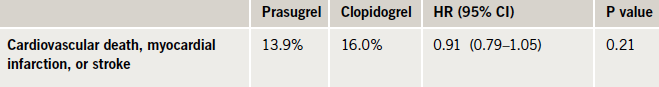
An additional analysis including an additional 2,083 patients aged 75 years or older in whom a reduced 5 mg dose of prasugrel was compared to the regular clopidogrel dose showed similar results.
Some good news
Unlike the TRITON trial, TRILOGY did not show an increase in severe bleeding complications with prasugrel, possibly because of the dose reductions in low body weight and elderly patients. Dr Ohman said this gave reassurance on concerns about the prolonged safety of the drug.
In addition, there was a surprising, time-dependent effect seen, with a trend towards a lower risk of ischaemic events with prasugrel after 12 months. “While there was no difference in the rate of the primary composite end point or its separate components between the two groups in the first year of the study, the curves began to diverge after the one year mark. This is an unexpected finding, and means that the trial raises more questions than it answers and is going to require a lot more analysis,” Dr Ohman said.
The implications of TRILOGY for practice are discussed in our ESC podcast
More encouraging results with TAVI
New data on use of transcatheter aortic-valve implantation (TAVI) from a German registry are reassuring for high-risk patients, with in-hospital mortality was “just as good, if not better” than with conventional aortic-valve surgery, reported Dr Christian Hamm (Kerckhoff Heart and Thorax Centre, Bad Nauheim, Germany). “Patients in high risk groups benefit at least as much from TAVI procedures, particularly when performed transfemorally, as from conventional surgery,” he added.
The German Aortic Valve Registry (GARY) was started in July 2010 and is the only registry so far to include both the new transcatheter procedure and conventional aortic valve replacements and repair. By July 2012 more than 26,000 patients were included from
92 centres, of whom 23% received TAVI.
Data were reported on 15,252 patients treated in 2011. This showed that TAVI is being used mainly in line with current guidelines, with 85% of all patients undergoing the trancatheter procedure being over 75 years (average 81 years versus 68 for surgery), and the TAVI patients also having a higher perioperative risk of mortality.
The reported in-hospital mortality for elective patients was 2.1% for conventional surgery, 5.1% for the transfemoral TAVI and 7.7% for the transapical approach. Stratification of the patients into risk groups revealed a particular benefit for people with high- and very high-risk when treated transfemorally, with mortality rates of 4.7% and 7.7%, respectively.
The overall number of cerebrovascular events during hospital stay was 2.2% in the conventionally treated group versus 3.7% for transfemoral TAVI and 3.5% for transapical TAVI. Vascular complications occurred in 11.9% for the transfemoral, 2.5% for the transapical and 1.0% for the conventional group. The number of patients who needed more than two units of packed red blood cells was 29.4% in conventional surgery and 25.4% with the transapical, versus 11.5% with the transfemoral approach.
Professor Friedrich-Wilhelm Mohr (Leipzig Heart Centre, Germant) commented: “Post-procedural rates of cerebrovascular events, vascular complications, renal failure and blood transfusions have decreased but need further attention. The high number of patients in the register will allow for thorough risk factor analysis for these complications. With the help of subgroup analyses and stratification for risk factors, we also expect to detect which treatment is best for which patient.”
Designated discussant of the results, Dr Olaf Wendler (King’s College Hospital, London), noted that around half of aortic valve patients more than 75 years of age are receiving the TAVI procedure which he said was “impressive” and far higher than anywhere else worldwide.
But he pointed out that the in-hospital mortality for the registry’s lower-risk TAVI patients was higher than that predicted, questioning if this is the right treatment for this group of patients.
Renal denervation benefits persist to 18 months
Long term results from the SYMPLICITY HTN 2 trial suggest that the blood pressure benefits of renal sympathetic denervation persist for at least 18 months.
Earlier results from the trial showed that ablation of the renal nerves led to average blood pressure reductions of 32/12 mmHg at six months in patients with drug-resistant hypertension.
After the six month point, patients in the control group were also offered the renal denervation treatment. The 18-month results showed that patients in the original ablation group continued at the blood pressure level demonstrated at six months (an average reduction of 32/12 mmHg from baseline) while those in the control group who had also now had the procedure also showed similar reductions (28/13 mmHg) from baseline.
Dr Murray Esler (Baker IDI Heart and Diabetes Institute, Melbourne, Australia) reported that pulse pressure improved and heart rates were stable or lower following the procedure. Also, no device-related serious adverse effects and no detrimental effects on the renal vasculature have been reported.
The renal denervation procedure also seems to have beneficial effects on psychological measures, according to a 173-patients study presented by Dr Denise Fischer (Universitätsklinikum des Saarlandes, Homburg, Germany). This showed that three months after ablation, blood pressure had decreased by an average of 17/7 mmHg, and the patients showed significant improvement on a multitasking test designed to assess their ability to respond to stress. Quality of life, anxiety, and depression, headache intensity and sleep problems also improved significantly.
Positive results with renal denervation were also reported from a French registry of 35 consecutive patients. Dr Darren Mylotte (Institut Cardiovasulaire de Paris Sud, France) noted that the average baseline blood pressure was 181/100 mmHg despite an average of 4.6 medications per patient and, at six-months after the procedure, this had been reduced by an average of 30.3/14.6 mmHg.
Dr Sarah Jarvis discusses the relevance of renal denervation studies for primary care in our ESC podcast
FAME II results show benefits of FFR-guided cardiac stenting
Patients with fractional flow reserve (FFR) guided stenting plus the best available medical therapy had superior outcomes to those treated with medical therapy alone, according to results from the FAME II Trial presented during a Hot Line session.
For patients found to have a significant stenosis with FFR, the primary endpoint (a composite of death, myocardial infarction, or urgent revascularisation) occurred in 4.3% of those in the percutaneous coronary intervention (PCI) plus medical therapy group versus 12.7% of those in the medical therapy group. The difference was driven by lower rates of urgent revascularisation in the PCI group than in the medical therapy only group (0.7% vs. 9.5%, p<0.001).
The new findings build upon data from the original FAME trial, which demonstrated improved outcomes and cost-savings when FFR is utilised to guide cardiac treatment procedures.
Learn more about the FAME study in our ESC podcast
New drug class may provide clinical benefits in patients with HF-pEF
The investigational compound LCZ696, an angiotensin receptor neprilysin inhibitor, is the first-in-class therapy to significantly reduce a key predictor of morbidity and mortality in patients with heart failure with preserved ejection fraction (HF-pEF).
Results from the Phase II PARAMOUNT study presented showed that after 12 weeks, LCZ696 met its primary end point by reducing N-terminal pro-B-type natriuretic peptide significantly more than valsartan. The data also suggest that LCZ696 may reverse some structural changes to the heart that occur in patients with heart failure.
“LCZ696 is unique in simultaneously blocking the renin angiotensin system while augmenting the body’s intrinsic natriuretic peptide system through neprilysin inhibition,” said Professor Scott Solomon (Harvard Medical School, Boston, US). “These dual effects may be important in the treatment of HFpEF.”
More on this new agent is discussed in our ESC podcast
ESC selects London for 2015 Congress
The 2015 Congress of the European Society of Cardiology (ESC) will be held in London. The Congress is the largest cardiology meeting in the world, with roughly 35,000 medical professionals expected to attend the five-day event from 29 August – 2 September 2015.
Professor Kim Fox (Royal Brompton Hospital, London), Past President of the ESC, said: “The UK has been a pioneer in cardiovascular research and treatment and it is fitting to bring the congress back to London for the first time in 63 years. Venues for events of this size are difficult to find and we are overjoyed that London now has the structure to host the ESC Congress. The eyes of the medical world will be focused on London as a leader in science and education”.
Younger women – a new risk group for MI
While better treatment does seem to be translating into a lower overall mortality rate after myocardial infarction (MI), there is a worrying trend of more heart attacks occurring in younger people, particularly women, according to the results of a new French study.
The FAST-MI study reported data from four one-month French nationwide registries, conducted five years apart (1995 to 2010), including a total of 6,707 patients with ST elevation MI.
During the study period, 30-day mortality decreased from 13.7% to 4.4% in STEMI patients; mortality decreased from 9.8% to 2.6% in men and from 23.7% to 9.8% in women. However, the average age of those with STEMI decreased from 66.2 years to 63.3 years over the study period, which appeared to be due to an increase in the proportion of younger women with STEMI.
Presenting the data, Dr Nicholas Danchin (Hôpital Européen Georges Pompidou, Paris, France), noted that two different trends seem to be occurring. The mortality rate in the older “traditional MI candidate” is falling, probably because of better primary-prevention efforts, and better treatment when the MI occurs. However, some of this progress is being countered by an increase in MI in younger people – particularly younger women (under 60 years) who smoke.
He reported that younger women still represent a small proportion of all MI patients (about 7% to 8%), but this is up from about 2% to 3% 15 years ago. Danchin suggested that the most likely explanation for this is the increased prevalence of smoking in younger women.
Data from the FAST-MI study show that smoking rates in younger women who have had an MI dramatically increased from 37% in 1995 to 73% in 2010. Obesity rates also increased in this group – up from 18% in 1995 to 27% in 2010.
Dr Sarah Jarvis discusses this study in our ESC podcast
