The 15th Annual Autumn Meeting of the British Society for Heart Failure (BSH) entitled ‘Heart failure, a multidisciplinary approach’, was held on 29th–30th November 2012 at the Queen Elizabeth II Conference Centre in London. Over 500 delegates attended the meeting, which was introduced by BSH Chair Dr Suzanna Hardman. Colin Cunnington reports on some of the highlights.

Mineralocorticoid receptor antagonists
Professor Faiez Zannad (Université de Lorraine, Nancy, France), the first of two guest lecturers, who has been an investigator in three major randomised controlled trials (RCT) of mineralocorticoid receptor antagonists (MRA) in heart failure,1-3 opened the first session.
There was a particular focus on the recent EMPHASIS-HF trial,3 which recruited heart failure (HF) patients with left ventricular systolic dysfunction (ejection fraction [EF] ≤30%, or EF 30-35% with QRS duration >130 ms) and mild symptoms (New York Heart Association [NYHA] class II). Eplerenone treatment resulted in a 37% relative risk reduction in the composite primary end point of cardiovascular death or HF hospitalisation compared with placebo.3 This benefit was observed despite high levels of concomitant treatment with angiotensin-converting enzyme (ACE) inhibitors or angiotensin receptor blockers (ARBs), and beta blockers. Furthermore all-cause mortality was significantly reduced by 24%, and HF hospitalisation by 48%. Subsequent analyses have shown that eplerenone reduces repeat HF hospitalisations4 and the incidence of new atrial fibrillation (AF).5
These findings, in combination with the data from RALES1 (NYHA III-IV patients with reduced EF) and EPHESUS2 (reduced EF following myocardial infarction [MI]) are now reflected in the updated 2012 European Society of Cardiology (ESC) HF guidelines,6 with MRAs being given an upgraded 1A recommendation in HF with reduced EF (HF-REF).
Potential mechanisms underlying the clinical benefits of MRAs in HF include antifibrotic mechanisms that slow HF progression and cardiac remodelling, and reduce arrhythmogenesis. Indeed, the benefit of spironolactone was greatest in patients with higher baseline serum markers of cardiac fibrosis,7 raising the future possibility of selectively treating these HF patients.
Clinical benefit of MRAs is the subject of additional studies including TOPCAT, a trial of spironolactone in patients with HF and preserved ejection fraction (HF-PEF, EF ≥45%). This has finished recruiting and should report soon. Two trials (ALBATROSS and REMINDER) are underway investigating early aldosterone blockade in ST-elevation MI (STEMI) and work continues in the development of novel methods to block the deleterious actions of aldosterone.
Cardiac remodelling
Professor Marc Pfeffer (Harvard Medical School, Boston, USA) opened the session on cardiac remodelling with a fascinating historical review of the biology of ventricular remodelling, beginning with animal models, progressing to observations in humans, and finally to large-scale clinical trials of drugs to prevent or reverse the cardiac maladaptation to stress and injury. This inspiring lecture reflected many years of his research with important influences being his late wife, Janice Pfeffer, and Professor Eugene Braunwald. It was intriguing to learn of the many years of ‘bench-to-bedside’ research that culminates in a clinical trial that changes the face of medicine, such as the SAVE trial (captopril following MI).8 Professor Pfeffer (figure 1) concluded on a positive note talking about the potential role of stem cell therapy as a viable treatment option in HF patients.9

Dr Robin Weir (Hairmyres Hospital, Glasgow) spoke on the current state of non-invasive imaging in systolic dysfunction, highlighting the fact that EF measurements by different modalities vary and are not interchangeable. Cardiac magnetic resonance remains the gold standard method for assessing ventricular function, although access is still limited in some areas. Professor Iain Squire (Glenfield Hospital, Leicester) gave an update on the role of biomarkers in HF, particularly the use of B-type natriuretic peptide (BNP) to guide HF therapy.10 There remains significant doubt about the clinical benefit of this approach and it was emphasised that patients should be treated with maximum-tolerated doses of ACE inhibitors/ARBs, beta blockers and MRAs, irrespective of BNP levels.
Atrial fibrillation
A further session addressed the complex issue of AF in HF. First, Dr Christopher George (Cardiff University) gave an illuminating lecture on the mechanisms underlying arrhythmogenesis in HF, focusing on a shift in thinking away from traditional therapies that target cell-surface ion channels, towards modulation of intracellular drivers of arrhythmogenesis, including ryanodine receptor-dependent calcium signalling.11
Professor John Cleland (University of Hull) emphasised the clinical importance of AF, particularly when it occurs after the onset of HF, when it is associated with worse outcomes.12 A number of drugs including ivabradine appear to be associated with an increased risk of AF. RCT data has not indicated any benefit of rhythm control over rate control in HF, with a tendency towards worse outcomes.13, 14 This is also true where dronedarone is used.15 Ranolazine has been noted to reduce arrhythmias (including AF) following MI16 and, interestingly, is currently being tested in combination with low-dose dronedarone in paroxysmal AF in the HARMONY trial. Vanoxerine has shown promise in animal models of AF.17 Professor Cleland also discussed the importance of anticoagulation of HF patients with AF, even if sinus rhythm is restored, with warfarin or possibly one of the new oral anticoagulant drugs (dabigatran, rivaroxaban and apixaban).
Dr Stephen Furniss (East Sussex Healthcare NHS Trust, Hastings) summarised the evidence for catheter ablation for AF in HF. Registry data18, 19 and small non-randomised studies20 have suggested a possible benefit of ablation over medical therapy, while a recent small RCT indicated an improvement in certain measures of cardiac function with ablation,19 although EF is especially subject to error during AF. Larger RCTs of ablation are needed to establish the efficacy of AF ablation in HF. Dr Rakesh Sharma (Royal Brompton Hospital, London) discussed the controversial topic of cardiac resynchronisation therapy (CRT) in patients with AF. Again, non-randomised studies have indicated a significant benefit of CRT in AF.21 However, RCT data remain sparse. The two trials (MUSTIC-AF22 and RAFT23), which included limited patients with AF did support CRT use in AF. Notwithstanding the lack of trial data, CRT devices are frequently implanted in AF patients in Europe.24 As with AF ablation, larger RCTs are warranted.
Acute heart failure
Acute HF has seen relatively few advances in recent years compared with chronic HF. Dr Simon Williams (University Hospital of South Manchester) reviewed a selection of recent studies in acute HF from a medical perspective. Serelaxin infusion reduced dyspnoea but there was no effect on early prognosis compared to placebo (RELAX-AHF25); there was, however, a reduction in death at six months. Nesiritide, which has been used clinically in acute HF in the USA, failed to show any benefit in ASCEND-HF, a large RCT.26 Furthermore, there was no difference in continuous or bolus intravenous diuretic regimes in the DOSE trial.27 Dr Robyn Smith (Golden Jubilee National Hospital, Glasgow) gave a practical lecture on management of acute HF from an intensive care perspective, and Mr Steve Tsui (Papworth Hospital, Cambridge) discussed surgical interventions in acute HF, with a particular reference to his algorithm for mechanical circulatory support in those awaiting urgent transplantation.
Young Investigators’ Award
Three abstracts of outstanding quality were presented at this year’s Young Investigators’ Award session.
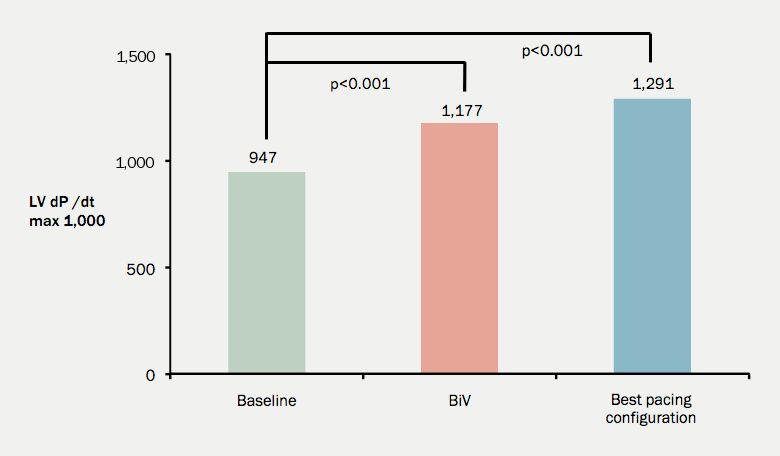
Dr Syed Ahsan (The Heart Hospital, London) studied the effects of multiple biventricular pacing configurations using a novel octapolar LV pacing electrode in an acute physiological study of patients referred for CRT. He showed that selection of pacing configuration on an individualised basis could improve LV haemodynamics, as measured invasively by LV dP/dtmax.
In a large prospective study of more than 1,000 patients, Dr Colette Jackson (University of Glasgow) investigated the prognostic significance of microvolt T-wave alternans (MTWA) testing in HF. This showed no difference in mortality if patients were stratified according to MTWA (either positive, negative or indeterminate), and concluded that MTWA testing is not a useful strategy to identify HF patients who may benefit from an implantable cardioverter-defibrillator (ICD).
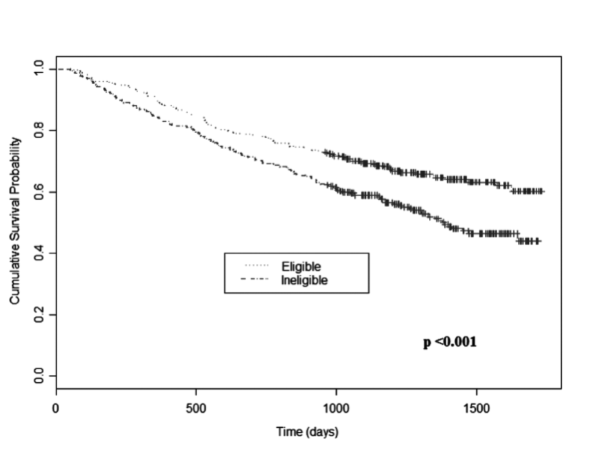
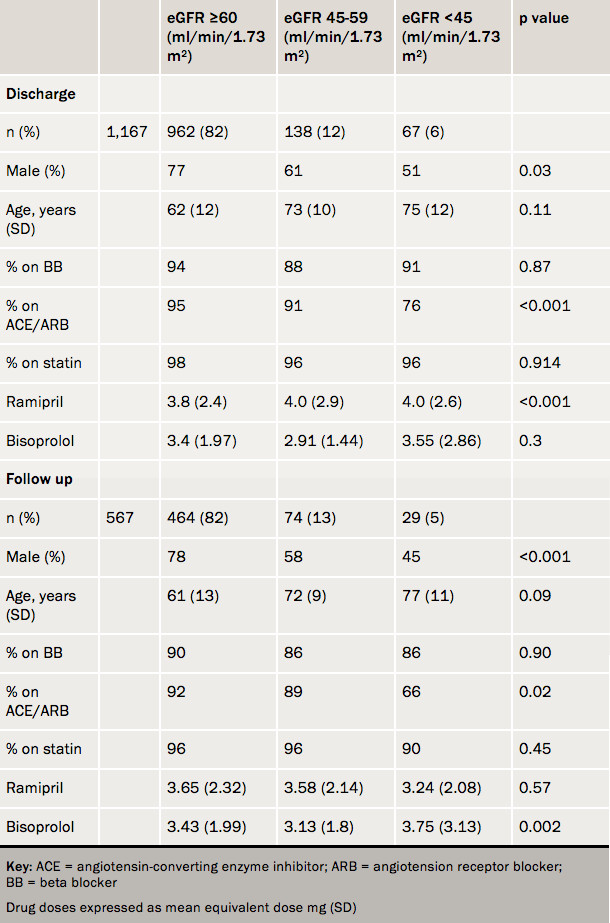
Finally, Dr Donah Zachariah (Portsmouth Hospitals NHS Trust) investigated the impact of chronic kidney disease (CKD) on secondary prevention therapy following primary percutaneous coronary intervention. In a retrospective, multicentre UK study, she demonstrated that current prescribing rates of secondary prevention medication are high compared to historical data, however ACE inhibitor usage was significantly lower in patients with CKD.
All presentations were of a very high standard with Dr Colette Jackson gaining the Young Investigators’ award. The abstracts from these three winning entries are published at https://bjcardio.co.uk/2013/02/british-society-of-heart-failure-young-investigators-award/
Other sessions in brief
Professor Theresa McDonagh (King’s College Hospital, London) summarised the 2012 ESC guidelines on the management of acute and chronic HF.6 These guidelines incorporate 19 new RCTs (mainly HF-REF). The main changes since 2008 relate to:
- an expansion in the role of MRAs (as described above)
- a new indication to consider ivabradine treatment (based on the SHIFT trial28)
- expanded indications for CRT
- the role of coronary revascularisation in HF (based on the STICH trial29)
- recognition of the growing use of ventricular assist devices, and
- the emergence of transcatheter valve interventions, including transcatheter aortic valve implantation and percutaneous mitral valve repair, in patients with unacceptably high surgical risk.
Professor Henry Dargie (University of Glasgow) gave important insights from the 2012 National Heart Failure Audit (available to download from www.bsh.org.uk). Disappointingly, mortality remains high following admission with decompensated HF (11.1% in-patient mortality; 37.3% at 12 months) with limited numbers gaining earlier access to the specialist cardiology services associated with improved outcomes. Following this, Sir Mike Richards (Department of Health) detailed forthcoming national strategies to reduce the burden of cardiovascular disease in the modern NHS. It is to be hoped that this will include acute hospital HF care.
In a thought-provoking session on palliative care, Dr Karen Hogg (Glasgow Royal Infirmary) Dr Nigel Rowell (Endeavour Practice, Middlesbrough), Mrs Annie MacCallum (NHS Gloucestershire), Dr John Baxter (Sunderland Royal Hospital) and Mr Michael Connelly (University Hospital of South Manchester) covered the multidisciplinary approach to end-of-life care. Topics included Anticipatory Care Pathways, practical advice on symptom control at end-of-life and in the elderly, ICD deactivation discussions, and holistic support of the HF patient and their carers.
The importance of heart rate was discussed in a dedicated session. Professor Andrew Clark (Castle Hill Hospital, Hull) demonstrated the epidemiological evidence that underpins the association between lower heart rate and longer life. Professor Dargie discussed the robust evidence to support beta-blockade, and Dr Suzanna Hardman (Whittington Hospital, London) explored the mechanisms of action of ivabradine, and possible recommended usage in light of SHIFT,28 its recent license in HF, and publication of the NICE STA guidance. Dr Roy Gardner (Golden Jubilee National Hospital, Glasgow) finished with optimisation of complex devices, including the recent MADIT-RIT study.30
Dr Alison Duncan (Royal Brompton Hospital, London) presented a case of HF secondary to ischaemic cardiomyopathy with concomitant severe mitral regurgitation. An expert panel of Dr Alison Seed (Blackpool Victoria Hospital), Mr Ben Bridgewater (University Hospital of South Manchester) and Dr Jonathan Byrne (King’s College Hospital, London) discussed the possible medical, surgical, and interventional therapeutic interventions respectively. Dr Steve Shaw (University Hospital of South Manchester), Dr Jim Moore (Gloucestershire Heart Failure Service) and Mrs Jayne Masters (University Hospital Southampton NHS Trust) presented a series of HF cases provoking animated and informative discussions.
Acknowledgement
The meeting was supported through educational grants from Friends of the BSH: Alere, Edwards Lifesciences, HeartWare, Medtronic, Novartis, Pfizer, Servier Laboratories, St Jude Medical and Thoratec.
Colin Cunnington
Specialty Registrar in Cardiology
Royal Albert Edward Infirmary, Wigan, WN1 2NN
Correspondence to:
([email protected])
References
1. Pitt B, Zannad F, Remme WJ et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med 1999;341:709–17. http://dx.doi.org/10.1056/NEJM199909023411001
2. Pitt B, Remme W, Zannad F et al. Eplerenone, a selective aldosterone blocker, in patients with left ventricular dysfunction after myocardial infarction. N Engl J Med 2003;348:1309–21. http://dx.doi.org/10.1056/NEJMoa030207
3. Zannad F, McMurray JJ, Krum H et al. Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med 2011;364:11–21. http://dx.doi.org/10.1056/NEJMoa1009492
4. Rogers JK, McMurray JJ, Pocock SJ et al. Eplerenone in patients with systolic heart failure and mild symptoms: analysis of repeat hospitalizations. Circulation 2012;126:2317–23. http://dx.doi.org/10.1161/CIRCULATIONAHA.112.110536
5. Swedberg K, Zannad F, McMurray JJ et al. Eplerenone and atrial fibrillation in mild systolic heart failure: results from the EMPHASIS-HF (Eplerenone in Mild Patients Hospitalization And SurvIval Study in Heart Failure) study. J Am Coll Cardiol 2012;59:1598–603. http://dx.doi.org/10.1016/j.jacc.2011.11.063
6. McMurray JJ, Adamopoulos S, Anker SD et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 2012;33: 1787–847. http://dx.doi.org/10.1093/eurheartj/ehs104
7. Zannad F, Alla F, Dousset B, Perez A, Pitt B. Limitation of excessive extracellular matrix turnover may contribute to survival benefit of spironolactone therapy in patients with congestive heart failure: insights from the randomized aldactone evaluation study (RALES). Rales Investigators. Circulation 2000;102:2700–6. http://dx.doi.org/10.1161/01.CIR.102.22.2700
8. Pfeffer MA, Braunwald E, Moye LA et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med 1992;327:669–77. http://dx.doi.org/10.1056/NEJM199209033271001
9. Chugh AR, Beache GM, Loughran JH et al. Administration of cardiac stem cells in patients with ischemic cardiomyopathy: the SCIPIO trial: surgical aspects and interim analysis of myocardial function and viability by magnetic resonance. Circulation 2012;126:S54–64. http://dx.doi.org/10.1161/CIRCULATIONAHA.112.092627
10. Porapakkham P, Porapakkham P, Zimmet H, Billah B, Krum H. B-type natriuretic peptide-guided heart failure therapy: a meta-analysis. Arch Intern Med 2010;170:507–14. http://dx.doi.org/10.1001/archinternmed.2010.35
11. Yano M, Yamamoto T, Ikeda Y, Matsuzaki M. Mechanisms of disease: ryanodine receptor defects in heart failure and fatal arrhythmia. Nat Clin Pract Cardiovasc Med 2006;3:43–52. http://dx.doi.org/10.1038/ncpcardio0419
12. Swedberg K, Olsson LG, Charlesworth A et al. Prognostic relevance of atrial fibrillation in patients with chronic heart failure on long-term treatment with beta-blockers: results from COMET. Eur Heart J 2005;26:1303–8. http://dx.doi.org/10.1093/eurheartj/ehi166
13. Freudenberger RS, Wilson AC, Kostis JB. Comparison of rate versus rhythm control for atrial fibrillation in patients with left ventricular dysfunction (from the AFFIRM Study). Am J Cardiol 2007;100:247–52. http://dx.doi.org/10.1016/j.amjcard.2007.02.101
14. Talajic M, Khairy P, Levesque S et al. Maintenance of sinus rhythm and survival in patients with heart failure and atrial fibrillation. J Am Coll Cardiol 2010;55:1796–802. http://dx.doi.org/10.1016/j.jacc.2010.01.023
15. Connolly SJ, Camm AJ, Halperin JL et al. Dronedarone in high-risk permanent atrial fibrillation. N Engl J Med 2011;365:2268–76. http://dx.doi.org/10.1056/NEJMoa1109867
16. Scirica BM, Morrow DA, Hod H et al. Effect of ranolazine, an antianginal agent with novel electrophysiological properties, on the incidence of arrhythmias in patients with non ST-segment elevation acute coronary syndrome: results from the Metabolic Efficiency With Ranolazine for Less Ischemia in Non ST-Elevation Acute Coronary Syndrome Thrombolysis in Myocardial Infarction 36 (MERLIN-TIMI 36) randomized controlled trial. Circulation 2007;116:1647–52. http://dx.doi.org/10.1161/CIRCULATIONAHA.107.724880
17. Cakulev I, Lacerda AE, Khrestian CM, Ryu K, Brown AM, Waldo AL. Oral vanoxerine prevents reinduction of atrial tachyarrhythmias: preliminary results. J Cardiovasc Electrophysiol 2011;22:1266–73. http://dx.doi.org/10.1111/j.1540-8167.2011.02098.x
18. Bunch TJ, Crandall BG, Weiss JP et al. Patients treated with catheter ablation for atrial fibrillation have long-term rates of death, stroke, and dementia similar to patients without atrial fibrillation. J Cardiovasc Electrophysiol 2011; 22:839–45. http://dx.doi.org/10.1111/j.1540-8167.2011.02035.x
19. Hunter RJ, McCready J, Diab I et al. Maintenance of sinus rhythm with an ablation strategy in patients with atrial fibrillation is associated with a lower risk of stroke and death. Heart 2012;98:48–53. http://dx.doi.org/10.1136/heartjnl-2011-300720
20. Hsu LF, Jais P, Sanders P et al. Catheter ablation for atrial fibrillation in congestive heart failure. N Engl J Med 2004;351:2373–83. http://dx.doi.org/10.1056/NEJMoa041018
21. Upadhyay GA, Choudhry NK, Auricchio A, Ruskin J, Singh JP. Cardiac resynchronization in patients with atrial fibrillation: a meta-analysis of prospective cohort studies. J Am Coll Cardiol 2008;52:1239–46. http://dx.doi.org/10.1016/j.jacc.2008.06.043
22. Linde C, Leclercq C, Rex S et al. Long-term benefits of biventricular pacing in congestive heart failure: results from the MUltisite STimulation in cardiomyopathy (MUSTIC) study. J Am Coll Cardiol 2002;40:111–18. http://dx.doi.org/10.1016/S0735-1097(02)01932-0
23. Healey JS, Hohnloser SH, Exner DV et al. Cardiac resynchronization therapy in patients with permanent atrial fibrillation: results from the Resynchronization for Ambulatory Heart Failure Trial (RAFT). Circ Heart Fail 2012;5:566–70. http://dx.doi.org/10.1161/CIRCHEARTFAILURE.112.968867
24. Dobreanu D, Dagres N, Svendsen JH, Marinskis G, Bongiorni MG, Blomstrom-Lundqvist C: Approach to cardiac resyncronization therapy. Europace 2012;14:1359–62. http://dx.doi.org/10.1093/europace/eus260
25. Teerlink JR, Cotter G, Davison BA et al. Serelaxin, recombinant human relaxin-2, for treatment of acute heart failure (RELAX-AHF): a randomised, placebo-controlled trial. Lancet 2012;381:29–39. http://dx.doi.org/10.1016/S0140-6736(12)61855-8
26. O’Connor CM, Starling RC, Hernandez AF et al. Effect of nesiritide in patients with acute decompensated heart failure. N Engl J Med 2011;365:32–43. http://dx.doi.org/10.1056/NEJMoa1100171
27. Felker GM, Lee KL, Bull DA et al. Diuretic strategies in patients with acute decompensated heart failure. N Engl J Med 2011;364: 797–805. http://dx.doi.org/10.1056/NEJMoa1005419
28. Swedberg K, Komajda M, Bohm M et al. Ivabradine and outcomes in chronic heart failure (SHIFT): a randomised placebo-controlled study. Lancet 2010;376:875–85. http://dx.doi.org/10.1016/S0140-6736(10)61198-1
29. Velazquez EJ, Lee KL, Deja MA et al. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med 2011;364:1607–16. http://dx.doi.org/10.1056/NEJMoa1100356
30. Moss AJ, Schuger C, Beck CA et al. Reduction in inappropriate therapy and mortality through ICD programming. N Engl J Med 2012;367:2275–83. http://dx.doi.org/10.1056/NEJMoa1211107