In this regular series ‘ECGs for the fainthearted’ Dr Heather Wetherell will be interpreting ECGs in a non-threatening and simple way. In this issue, we look at the digitalis effect on ECGs
This issue, we have a little teaser for GPs, who may reasonably come across this kind of electrocardiogram (ECG) any day of the week.
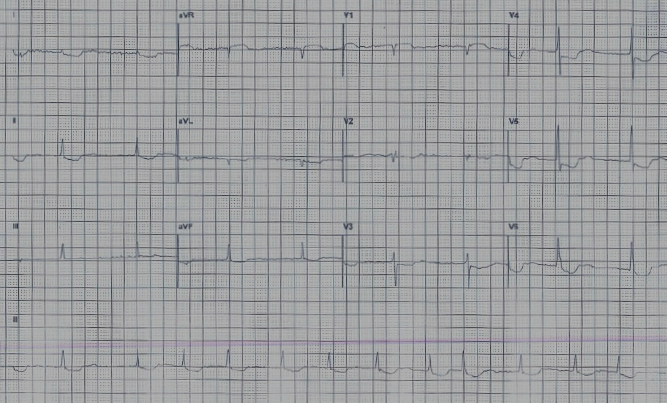
Figure 1 shows the ECG of a well, 83-year-old woman, who attended her GP’s surgery for her ‘annual review’. As part of this review, the practice nurse carried out a routine ECG.
Believe or not, it’s possible to answer the following three questions from this ECG:
Q1: What chronic condition was being monitored at her annual review?
Q2: What is she taking for this condition?
Q3: What action should the GP take now?
Let’s go through the ECG together.
For the time being, just ignore the funny shaped ST segments.
Start as always, by checking the background rhythm:
- are there P waves present?
- are the QRS complexes regular?
I’m sure you will agree that the answer to both questions is ‘no’.
This ECG shows an underlying rhythm of atrial fibrillation (AF) with a good rate control (around 80 bpm ventricular response).
The ‘quick’ way to measure rate on an irregular rhythm is by counting the number of complexes in six seconds (30 large squares) and multiplying by 10. In this ECG, for example, taking the long lead II strip, there are eight complexes in 30 large squares. So: 8 x 10 = 80 bpm.
Answer 1
We can assume that this lady was attending the surgery for her annual AF review. As AF is a precursor to many other cardiac conditions, an annual ECG is helpful, but arguable. An annual pulse rate check is a bare minimum.
Answer 2

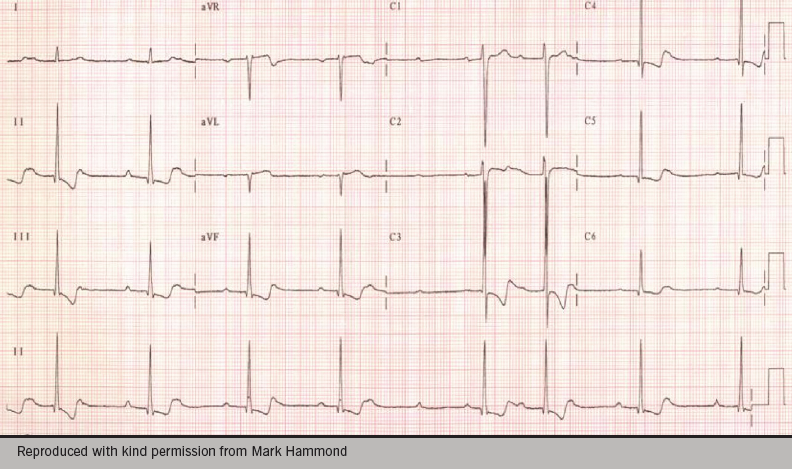
This lady is taking digoxin. The ST-T complexes here are ‘scooping’ – consistent with a digitalis ‘effect’. In the digitalis effect, the ST segments are often likened to a ‘reverse tick’ or to the shape of Dali’s moustache (see figure 2).
The important learning point here is that the digitalis ‘effect’ does not necessarily mean toxicity. These ECG features can often be seen when digoxin levels are within the therapeutic range.
In other words, ECG changes with digoxin can be either:
Therapeutic (also known as the digitalis ‘effect’)
- ST-segment depression resembling a ‘reverse tick’
- Reduced T wave
- Shortening of the QT interval.
Or
Toxic
- T-wave inversion
- Arrhythmias.
Answer 3
This lady appears clinically well and denies any untoward symptoms. Given the changes seen on her ECG, we can probably assume that this is simply a digitalis ‘effect’ and no treatment or adjustment to her medication is necessary. It wouldn’t hurt to check her digoxin levels for reassurance (and while you’re at it, her serum potassium too, just in case) but this isn’t necessarily essential.
In summary: Treat the patient, not the ECG.
No action necessary.
Digoxin
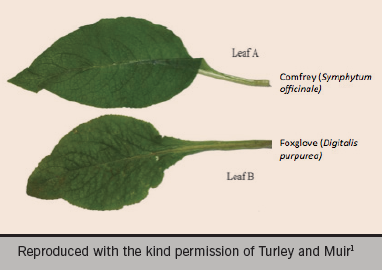
The common foxglove species is Digitalis purpurea. Digoxin is derived from the species Digitalis lanata and was first described by William Withering in 1785. It is sometimes used to increase cardiac contractility (positive inotrope) and as an anti-arrhythmic agent to control heart rate (e.g. in fast AF). Superior rate-limiting agents, such as beta blockers, have now superseded digoxin as a first-line agent but its role remains important in AF associated with heart failure.
Symptoms of digoxin toxicity
These include:
- lethargy
- nausea and vomiting
- diarrhoea
- abdominal pain
- visual disturbances
- hallucinations and delirium
- severe headache.
Almost any dysrrhythmia may occur except sinus tachycardia, superventricular tachycardia (SVT) and rapid AF.
Figure 3 shows an example of an ECG after a digitalis overdose in a very unwell patient with all the above symptoms and digoxin levels of 4.7 ug/L (therapeutic range 1–2 ug/L). Note the irregular bradycardia, atrioventricular block and T-wave inversion.
This ECG was recorded on a young farm worker who was admitted after eating foxglove leaves, having mistaken them for edible comfrey (see figure 4). Hopefully, the history and examination would have been clues here!
Editors’ note
This is the last article in our ECGs for the fainthearted series. We would like to thank Heather Wetherell for her hugely popular contributions and hope she will be writing for us again soon.
References
1. Turley AJ, Muir DF. ECG for physicians. A potentially fatal case of mistaken identity. Resuscitation 2008;76;323–4. http://dx.doi.org/10.1016/j.resuscitation.2007.09.001
Our very entertaining columnist, Michael Norell, will be returning in our next issue with his ‘The oblique view’ column
