Previous research estimates that up to 40% of palpitation presentations to the emergency department (ED) have cardiac aetiology. This study was performed to determine the proportion of patients referred on for cardiology investigations that consequentially had new significant pathology diagnosed; and the effect of follow-up investigation on patient re-attendance to the ED with the complaint of palpitations.
Patients referred to a community cardiology centre in 2016 for investigation into palpitations following an ED presentation were included. The diagnosis that each patient received from these investigations was analysed to see whether: (a) new underlying cardiac abnormality was identified and (b) that abnormality was significant, requiring follow-up.
There were 93 patients meeting criteria for analysis: 28% had a cardiac cause for their palpitations elicited, including 11% with new significant pathology identified. Rate of re-attendance to the ED was reduced once cardiology investigations were completed (0.11 presentations/patient; 95% confidence interval [CI] 0.04 to 0.18) compared with the investigation period (0.75 presentations/patient; 95%CI 0.3 to 1.2).
In conclusion, although only one tenth of patients referred for investigations had new significant cardiac pathology identified, completing cardiology investigations reduced ED re-attendance.
Introduction
Palpitations are a common reason for presentation to the emergency department (ED),1,2 and can be extremely concerning to the patient and doctor. In the ED, clinical history, examination and basic investigations (including an electrocardiogram [ECG]) at the time of presentation often cannot elicit the cause for the symptoms. After ensuring that there is no acute rhythm disturbance necessitating a hospital admission, patients are routinely discharged back to their primary care doctor with advice for referral to a cardiology outpatient service for prolonged ECG recording and echocardiogram, as per National Institute for Health and Care Excellence (NICE) guidance.3 Either a hospital or community cardiology centre subsequently carries out these outpatient tests.
In 1996, Weber and Kapoor published a study that found that around 40% of patients presenting to the ED with palpitations had a cardiac aetiology.2,4 This study supports referral to cardiology investigative follow-up for those who present to the ED with symptomatic palpitations.5 However, no subsequent investigation has examined the proportion of these patients undergoing such follow-up who have cardiac pathology identified as a consequence.
Anecdotally, patients referred to community cardiology services for assessment after a presentation to the ED with palpitations are frequently not found to have a significant underlying cardiac rhythm disturbance, especially in the younger patient groups without history of cardiovascular disease. With the increasing demands on community and secondary care cardiology services, reducing referrals for a patient group with a low likelihood of significant pathology is attractive. Therefore, more research on the outcomes of these patients is warranted.
This study was designed to investigate the outcomes of patients referred to a community cardiology centre for investigation having presented to their local hospital’s ED with palpitations.
Methods
The study took place in Milton Keynes, a large English town with a population of 270,000 people. The local ED is located at Milton Keynes University Hospital Foundation Trust and sees around 220 patients per day. Whaddon Medical Centre is a GP practice within Milton Keynes and provides a community cardiology service. This accepts and sees approximately 80% of all primary care referrals to cardiology in Milton Keynes and was, therefore, used as the site for this study.
The study included all patients who were referred to community cardiology at Whaddon Medical Centre by their GP for investigations for palpitations between 1 January 2016 and 31 December 2016. Using the electronic patient record programme ‘Systmone’, a list of patients who had been referred to Whaddon Medical Centre in 2016 with the word ‘palpitations’ used in the referral was generated. The ‘Systmone’ record of each patient on this list was then accessed and analysed to find evidence of an ED presentation within a 12-month period prior to the referral. This evidence was in the form of an ED discharge letter with a presenting complaint marked as either ‘palpitations’ or ‘fast heart rate’. The medical records of this subpopulation of patients were analysed in detail.
The age and sex of each patient was recorded, along with the date of first presentation to the ED with palpitations; the date and nature of the first cardiac test that was performed and the subsequent result; the date and nature of the second cardiac test performed and the result; the date a final report of the investigation results was sent to the patient’s GP and the conclusion of the investigations (in terms of final diagnosis, need for further investigation and need for medication adjustment); and the number of repeat visits the patient made to the ED with the complaint of palpitations (both during the investigation period and after the conclusion of the investigation was reported). Data were recorded in an Excel spreadsheet. Once collated, one clinician from the community cardiology centre reviewed the findings from the tests performed and recorded for each patient whether cardiac pathology was definitively identified or not.
The paired sample t-test was used to determine whether there was a difference between the mean number of patient re-presentations to ED with palpitations during the investigation period compared with once the investigations had been concluded. The investigation period was classified as the number of days between the date of the initial ED presentation to the date of the final letter being sent to the GP with the investigation conclusion. The post-investigation period was classified as the number of days between the date that the final investigation conclusion letter was sent out and the date that the data were collected for this study. The total number of repeat presentations made to ED with palpitations by the studied patients during their investigation period was divided by the length of their investigation period and multiplied by 365. This created a value for the rate of re-presentations in one year (365 days) during the investigation period in each patient. A similar process was carried out for the post-investigation period to create a second set of values for the rates of re-presentations in one year during the post-investigation period. The rate of re-presentations in one year was used as the input data for the paired sample t-test.
Results
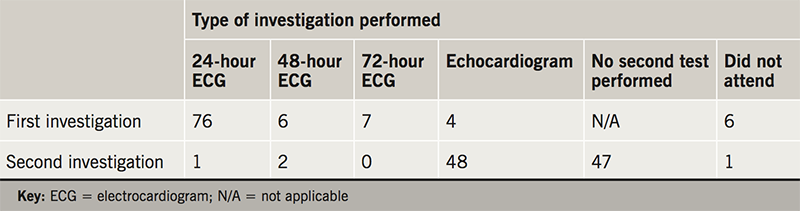
During 2016, Whaddon Medical Centre received 534 referrals to its community cardiology service for investigation into palpitations: 99 were the consequence of a presentation to an ED with palpitations (63 female, 36 male). The average age of these 99 patients was 44 years (standard deviation [SD] 16, range 16–83). See table 1 for the types of investigation performed.
Outcomes
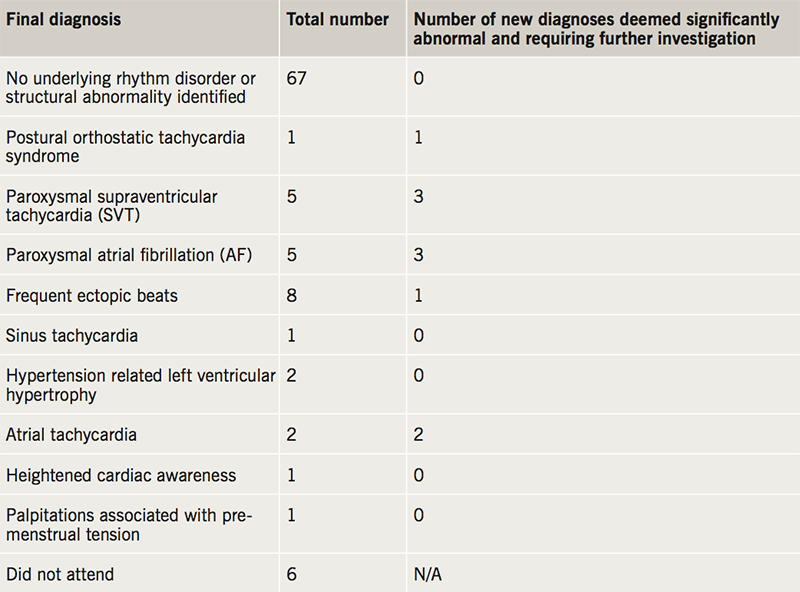
Of the 99 patient case records reviewed, six patients did not attend their initial cardiology clinic appointment and were, therefore, excluded from the study. Of the remaining 93 patients, 67 (72%) had no underlying rhythm disorder identified whatsoever and 12 (13%) had a non-significant cardiac diagnosis for their palpitations made (frequent ectopics, sinus tachycardia, mild left ventricular hypertrophy due to hypertension, heightened cardiac awareness and palpitations associated with pre-menstrual tension). Ten (11%) patients had a new significant underlying cardiac disorder identified requiring further investigation; 14 (15%) patients in total had abnormalities detected requiring further follow-up but four of these had had the abnormality identified during their ED visit (two out of the five patients with atrial fibrillation and two out of the five patients with supraventricular tachycardia had had the diagnosis made previously). See table 2 for the diagnoses given and table 3 for outcomes in different patient age groups. As a result of the investigations, 31 of the 93 patients had medication changes advised: 27 of these changes involved the recommendation of a beta blocker. Other medications advocated or altered included diltiazem (one patient), flecainide (one patient) and verapamil (two patients).
Repeat attendances
The mean investigation period duration was 149 days (SD 98.1 days). The median investigation period duration was 118 days. In this period, there were a total of 25 repeat presentations to the ED with palpitations by 14 patients (the maximum number of re-attendances by an individual patient was six). This gave a mean rate of re-presentations in one year of 0.75 presentations/patient (95% confidence interval [CI] 0.3 to 1.2). None of these patients went on to have a significant abnormality detected from their cardiology investigations.
The mean period of time from the conclusion of the patient’s investigations and the date of this study was 402 days (SD 154 days). The median period of time was 380 days. A total of 10 repeat presentations to the ED occurred in this period by nine patients: two had had significant abnormalities detected from the cardiology investigations. This gave a mean rate of re-presentations in one year of 0.11 presentations/patient (95% CI 0.04 to 0.18).
There was a significant difference between the rates of re-presentations to ED in one year in the investigation period (mean 0.75, SD 2.17) and post-investigation period (mean 0.11, SD 0.344); t(93)=1.988, p=0.05.
Discussion
Our study demonstrated that only 11% of referrals for palpitations after an ED attendance to a community cardiology service result in a new, significant cardiac diagnosis. This is much lower than previous studies that had either been performed over 20 years ago,2,4 or included patients that had not presented to an ED.6,7 This might reflect the increase in attendances to EDs, a change in patient behaviour or an increase in out-of-hour’s services referring patients on to ED because of lack of ECG and assessment facilities. Although only 11% of patients receiving a significant diagnosis seems a small proportion, this is not dissimilar to the percentage of abnormalities requiring further investigation that are detected from well-established breast cancer screening programmes (5–14%).8
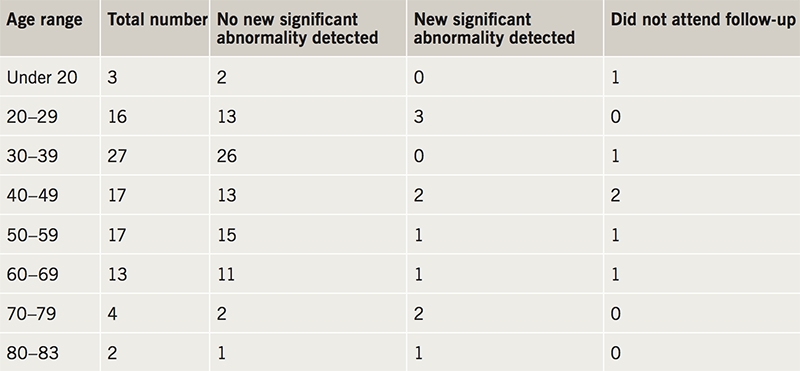
The vast majority of patients, particularly those in the lower age groups, had no identified cardiac pathology. Identification of new significant pathology in the 30–49 age group (two out of 44) was notably lower than that in the under 30 (three out of 19 patients) and over 50 (four out of 24 patients) age groups. This provides much needed data to support clinicians in their decisions not to refer all those presenting to the ED with palpitations on for further investigative work.
A previous study has suggested that 75% of patients suffering from palpitations will go on to experience recurrent episodes.9 One benefit of referring all patients who present to the ED with palpitations is the reassurance they feel when assessed in a specialist clinic. Although the majority of the patients that were referred to the cardiology community centre did not receive a diagnosis for their palpitations, on conclusion of cardiology investigations, the likelihood of patients re-attending the ED complaining of palpitations reduced by around seven times. This significant difference can be interpreted as highlighting the beneficial effect of reassurance in the patient population. After the outcome of investigations were reported, only two of the 14 patients who had presented again to the ED in the investigation period had further attendances with palpitations (one had three attendances during the investigation period and one attendance after, the other had two attendances during the investigation period and one after). Neither of these two patients had an abnormality identified from their investigations. Further studies are needed to investigate this in a qualitative way. There may be other causes behind this trend; perhaps during the investigation period, patients were encouraged to attend their ED when they experienced palpitations in the hope of recording an arrhythmia on ECG. In chronically resource-stretched healthcare systems, offering an investigation to a patient that is highly likely to show no abnormality may go on to reduce the likelihood of that same patient continuing to present to healthcare professionals with the same benign complaint.
Limitations
This study only investigated the referrals to the local community cardiac service. Although this service receives over 70% of all primary care referrals (all referrals recommended from the ED will have to be performed by the patient’s GP) some patients would have been referred to the local hospital, and are, therefore, not included in this study. It is possible that the hospital outpatient cardiology department received a greater proportion of referrals with significant undiagnosed cardiac pathology, as GPs may have specifically referred to secondary care if they had greater suspicion of cardiac pathology.
It was surprising that less than 20% of all referrals to the community cardiology centre for investigations into palpitations were generated from an ED visit. Although the remit of this investigation focused on patients that had presented to the ED, the study may have benefited from including patients that had presented to urgent care centres also, another 24-hour primary care service.
Implications for clinical practice
Less than 5% of patients referred to the community cardiology centre between the ages of 30 and 49 had significant cardiac pathology identified that required further specialist referral. In the under 30 age group, 16% of patients had significant cardiac pathology identified. In the over 49 age group, 17% had significant cardiac pathology identified. Although a number of arrhythmogenic causes of palpitations are clinically significant,10 and should not be overlooked, emergency physicians recognise that palpitations are a common and often benign complaint.11 Given that almost half of all patients referred to the community cardiology centre were between the ages of 30 and 49, perhaps future guidance on when to refer palpitations to secondary services should place greater emphasis on the age groups of patients most likely to be suffering from an underlying cardiac condition.
The positive impact of completing the secondary care cardiology investigations on reducing ED re-attendance with the same complaint emphasises the importance of reassurance in the management of palpitations. Emergency and cardiology physicians should ensure that they take the time to explain to a patient with benign palpitations why they do not require further investigations or follow-up.
Conflicts of interest
None declared.
Funding and study approval
There are no funding sources to declare and ethical approval was not required for this project.
Key messages
- Just over a quarter of patients presenting to the emergency department with palpitations and referred on to secondary cardiology services had a cardiac cause for their palpitations identified; with around 10% having new significant pathology requiring further investigation detected
- Receiving a conclusion from follow-up investigations into the cause of their palpitations correlates with reduced re-attendance to the emergency department with palpitations
- Patients between the ages of 30 to 49 presenting to the emergency department with palpitations may be less likely to have an underlying cardiac abnormality compared with younger and older age ranges
References
1. Reavley PDA. Palpitations. RCEM Learning 2017. Available at: https://www.rcemlearning.co.uk/references/palpitations/
2. Probst MA, Mower WR, Kanzaria HK, Hoffman JR, Buch EF, Sun BC. Analysis of emergency department visits for palpitations (from the National Hospital Ambulatory Medical Care Survey). Am J Cardiol 2014;113:1685–90. https://doi.org/10.1016/j.amjcard.2014.02.020
3. National Institute for Health and Care Excellence. Palpitations. Clinical Knowledge Summaries. London: NICE, 2015. https://doi.org/10.1002/14651858.CD009502.pub3
4. Weber BE, Kapoor WN. Evaluation and outcomes of patients with palpitations. Am J Med 1996;100:138–48. https://doi.org/10.1016/S0002-9343(97)89451-X
5. Thavendiranathan P, Bagai A, Khoo C, Dorian P, Choudhry NK. Does this patient with palpitations have a cardiac arrhythmia? JAMA 2009;302:2135. https://doi.org/10.1001/jama.2009.1673
6. Mayou R, Sprigings D, Birkhead J, Price J. Characteristics of patients presenting to a cardiac clinic with palpitation. QJM 2003;96:115–23. https://doi.org/10.1093/qjmed/hcg017
7. Wolff A, Cowan C. 10 steps before your refer for palpitations. Br J Cardiol 2009;16:182–6. Available from: https://bjcardio.co.uk/2009/07/10-steps-before-your-refer-for-palpitations/
8. Rauscher GH, Murphy AM, Orsi JM, Dupuy DM, Grabler PM, Weldon CB. Beyond the mammography quality standards act: measuring the quality of breast cancer screening programs. AJR Am J Roentgenol 2014;202:145–51. https://doi.org/10.2214/AJR.13.10806
9. Fraser S, Evans MF. Diagnosis and prognosis of patients with palpitations. Can Fam Physician 1997;43:2131–2. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2255099/pdf/canfamphys00070-0053.pdf
10. Raviele A, Giada F, Bergfeldt L et al. Management of patients with palpitations: a position paper from the European Heart Rhythm Association. Europace 2011;13:920–34. https://doi.org/10.1093/europace/eur130
11. Probst MA, Kanzaria HK, Hoffman JR et al. Emergency physicians’ perceptions and decision-making processes regarding patients presenting with palpitations. J Emerg Med 2015;49:236.e2–243.e2. https://doi.org/10.1016/j.jemermed.2015.02.013
