A syncope pathway for secondary care was launched in the Queen Elizabeth University Hospital (QEUH), Glasgow, in 2016. The pathway aims to risk stratify patients into three categories: high risk (requiring admission), intermediate risk (suitable for discharge ± outpatient review) or low risk (no further investigation required). There are clear referral procedures to the rapid access syncope clinic (RASCL). Our aim was to assess the impact of the pathway on unscheduled care in terms of admission rates, length of stay and referrals to RASCL.
Data were collected on three occasions: before the introduction of the pathway, immediately after and again 14 months later. Those patients with a diagnostic ICD-10 code of ‘syncope and collapse’ or ‘orthostatic hypotension’ presenting to the QEUH (both emergency department and immediate assessment unit, via GP referral) were identified.
There were 779 patients identified, 538 were included for analysis once other diagnoses were excluded: 46% were male with an age range from 16 to 95 years with a median age of 65.5 years.
All high-risk patients were admitted. For intermediate-risk patients the admission rate fell from 62% to 52% immediately after pathway introduction and after one year to 42%, suggesting sustained improvement (p=0.08). Admission for low-risk patients after one year of pathway roll out fell from 27% to 12% (p=0.04). The median length of stay prior to introduction was three days, this fell to one day one-year post-pathway, saving 56 bed days per month.
In conclusion, a syncope pathway and RASCL has reduced admission of low-risk patients, provided appropriate follow-up for intermediate risk, and reduced length of stay for those requiring admission.
Introduction
Syncope is defined as a transient loss of consciousness (TLoC) secondary to cerebral hypoperfusion, associated with loss of tone and spontaneous recovery.1 It has a lifetime prevalence of 20%,2 and an incidence of 0.80–0.93 per 1,000 person-years, which occurs in a roughly bimodal pattern, with an initial peak in early adulthood followed by a further more pronounced peak in older age.3
Syncope is merely one form of TLoC. Other causes of TLoC include seizures, sleep disturbance, accidental falls and some psychiatric disorders. Syncope itself can be grouped into four major categories: reflex syncope (vasovagal and situational), orthostatic syncope, cardiac arrhythmias and structural cardiopulmonary disease. Of these, vasovagal syncope is the most common cause,4 accounting for up to 66% of all syncopal events seen in emergency departments (EDs).5,6 While the aetiology of syncope can be unclear on initial evaluation, the frequency of unexplained syncope is reducing with the development of more specialised clinics.7,8
Syncope results in an increased risk of mortality, regardless of cause, with those suffering from cardiogenic syncope at the greatest risk.3,7 Identification of risk factors is a crucial component in the appropriate management of syncope. Given the high costs of inpatient stay and shortage of acute medical beds, it is also important that patients who are at low risk of morbidity/mortality are not admitted unnecessarily.
Risk stratification is important so that clinicians can identify patients with a low-risk condition, enabling a patient to be discharged with adequate education, and also to recognise likely high-risk cardiovascular conditions requiring urgent investigation or admission. Risk-stratification scores have not currently shown better sensitivity or specificity compared with clinical judgement, and should not be used alone to perform syncope risk stratification.7
A syncope service was initially set up in Glasgow, UK, in 2004. This consisted of a weekly syncope clinic and information for the ED on who to refer. Referrals from the ED remained low, 4% of all syncope clinic referrals. In 2015, following the opening of the 1,109 bed Queen Elizabeth University Hospital (QEUH), three separate sites were merged and the syncope service redesigned. An improvement programme was introduced comprising: a risk-stratification pathway; a new referral process; and the availability of two urgent slots at the rebranded rapid access syncope clinic (RASCL).
RASCL is a clinician-led service and provides a one-stop assessment with timely investigations, including same-day cardiac monitoring, tilt-table testing and direct access to implantable loop recorders (ILRs). Investigation and management is in line with the European Society of Cardiology (ESC) syncope guidelines.7 The clinic ensures that patients with moderate-to-high-risk TLoC have rapid access to appropriate investigations and clinical expertise in order to make a timely diagnosis and treatment plan.
The aim of our study was to increase the number of patients discharged from the front door and reduce the length of stay for those patients admitted with a presentation of syncope. We collected data relating to the admission rate and length of stay in those patients presenting with syncope. This data collection was undertaken prior to introduction of the improvement programme, immediately after and again one year later.
Materials and method
The pathway was designed by colleagues who were involved in running the syncope service at QEUH (medicine for the elderly and cardiology) based on ESC guidelines.7 Key stakeholders in acute and general medicine, emergency medicine and neurology were consulted, and the pathway published on our Trakcare system (clinical knowledge publisher), with all our other guidelines (figure 1).
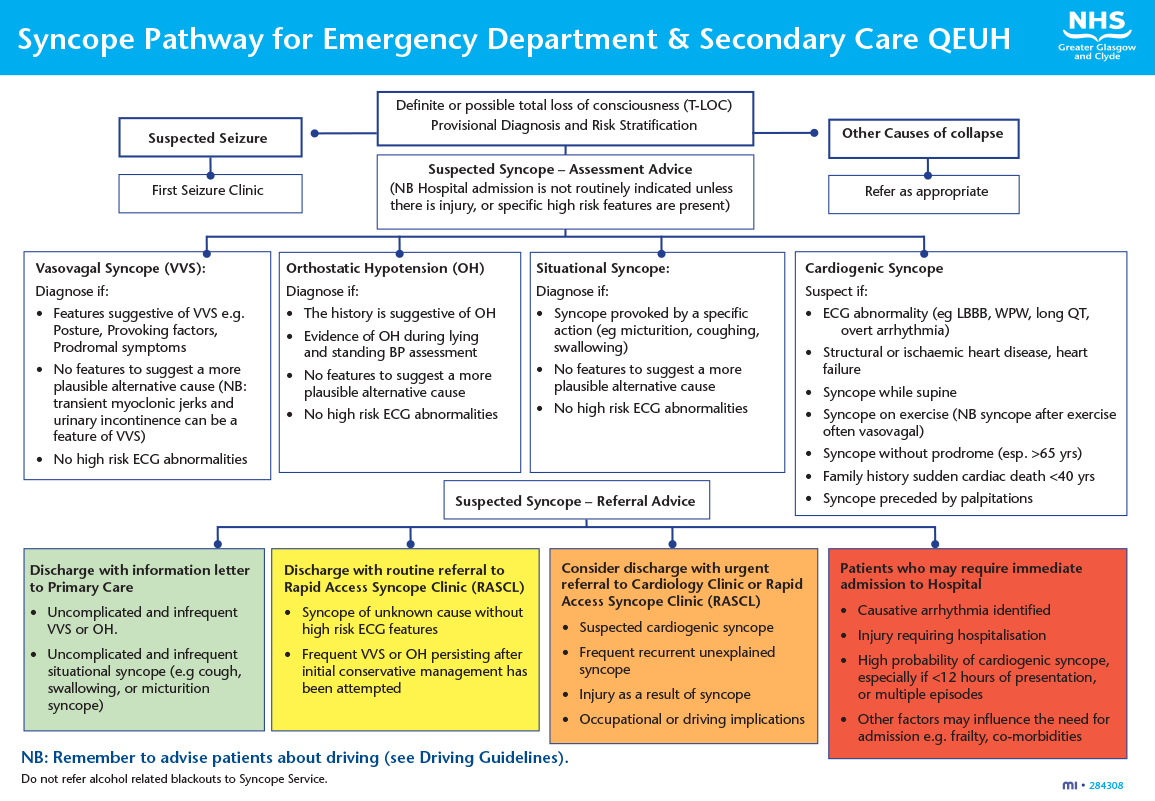
Our syncope pathway classified patients as low, intermediate or high risk according to the traffic light system. Patients with high-risk features (red and amber box) are those who require an intensive diagnostic approach and may need urgent treatment/admission. We suggest those with an injury, such as a fracture, or who are unable to manage functionally at home due to injury are admitted. For patients in the amber box, where safe discharge is an option, we offer a rapid-access appointment within two weeks. Low risk (green box) are those patients who do not need further diagnostic tests in the ED, are likely to have situational syncope, and can be followed up in primary care. Those patients in the yellow box (neither high nor low risk) may require a routine RASCL referral.
Data were collected on three occasions: before the introduction of the pathway (December 2015 to January 2016), immediately after pathway introduction (January to February 2016), and again 14 months later (April to June 2017). Patients diagnosed with ‘syncope and collapse’ or ‘orthostatic hypotension’, according to ICD-10 classification, were identified through electronic coding of diagnosis by the admitting clinician at time of leaving either the ED or GP assessment area for admission or discharge home. This information was then used to flag case notes for initial review via the Clinical Portal (Orion Health, Auckland, New Zealand) to confirm correct coding. Those with an incorrect diagnosis were excluded.
Data were collected retrospectively and included: age; gender; department attended; grade of assessing clinician; initial diagnosis; electrocardiogram (ECG) findings; presence of arrhythmia; lying/standing blood pressure measurements; total episodes of TLoC; previous attendances with syncope; whether injury was sustained; history of alcohol excess; reason for admission; suspected cause of syncope; length of stay; driving status; provision of driving advice; and appropriate management plan according to the newly designed syncope pathway.
Results
A total of 779 patients were identified during the three data collection periods. Of these, 241 patients were excluded (235 not syncope, six with no case notes available) and 538 patients were included in the final analysis. Table 1 shows the demographic data collected: 46% were male. Age range was 16 to 95 years with a mean age of 65.5 years: 86% of patients presented to hospital via the ED. Table 2 shows the cornerstone assessment at initial referral.
Table 1. Patient demographics
| Before pathway 22/01/15 to 22/01/2016 | After pathway 22/01/16 to 22/02/16 | 1-year post-pathway 01/04/2017 to 30/06/2017 | Total | |
|---|---|---|---|---|
| Number of patients | 108 (average 27 patients/week) |
108 (average 27 patients/week) |
322 (average 25 patients/week) |
538 |
| Males | 47.2% (n=51) | 46.3% (n=50) | 46% (n=147) | 46% (n=248) |
| Mean age, years | 68.5 | 63.5 | 65 | 65.5 |
| Presented via emergency department | 88.9% (n=96) | 88% (n=95) | 84% (n=271) | 86% (n=462) |
Table 2. Cornerstone assessment at initial referral
| Before pathway | After pathway | 1-year post-pathway | Total | |
|---|---|---|---|---|
| ECG done | 94.4% (n=102) | 98.1% (n=106) | 97.2% (n=315) | 97.2% (n=523) |
| L+S BP done | 44.4% (n=48) | 36.1% (n=39) | 26.8% (n=87) | 32.3% (n=174) |
| Key: ECG = electrocardiogram; L+S BP = lying and standing blood pressure | ||||
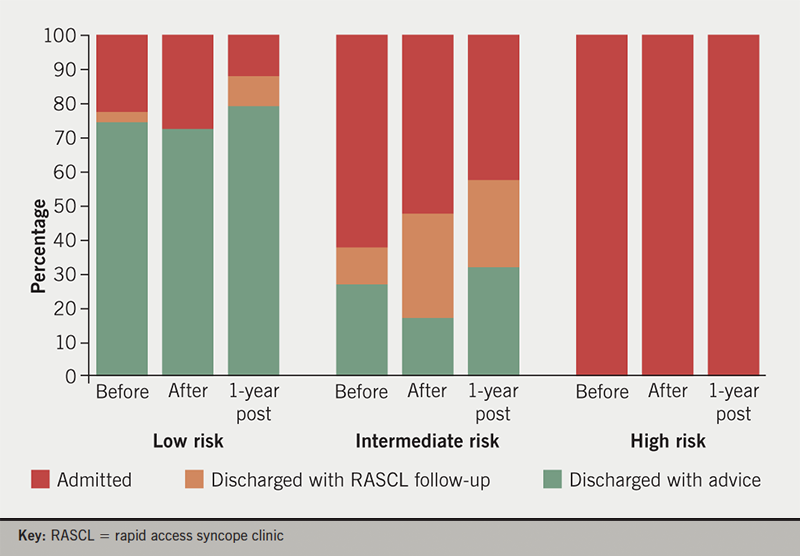
Prior to and following the introduction of the pathway, all high-risk patients were admitted. There was no immediate fall in the admission of low-risk patients but, after one year, the low-risk admission rate had fallen from 27% to 12% (p=0.04 calculated through 2 × 2 contingency table using Fisher’s exact test). For intermediate-risk patients, the admission rate fell from 62% to 52% immediately after pathway introduction and, after one year, had fallen a further 10% to 42%, suggesting the improvement has been sustained (p=0.08) (figure 2).
The median length of stay for patients admitted for investigation of syncope (excluding those admitted for injury, intercurrent illness or frailty) prior to the introduction of the pathway was three (range 0–42) days. This fell to 1.5 (range 1–18) days immediately after pathway introduction and one (range 0–18) day after one year (p=0.002, calculated using student’s t-test).
Table 3. Reasons for admission of low-risk patients
| Reason | Number |
|---|---|
| Awaiting troponin | 4 |
| Collapse ?cause for observation/telemetry | 13 |
| ?Cerebrovascular accident | 1 |
| ?Hypoglycaemia | 1 |
| For intravenous fluids | 2 |
During the data collection period, there were two re-presentations from within the low-risk patient group with further episodes of syncope, neither of which resulted in subsequent admission or harm. All urgent referrals to RASCL were seen within two weeks. Referrals from the ED to RASCL have increased each year to 17% of all clinic referrals.
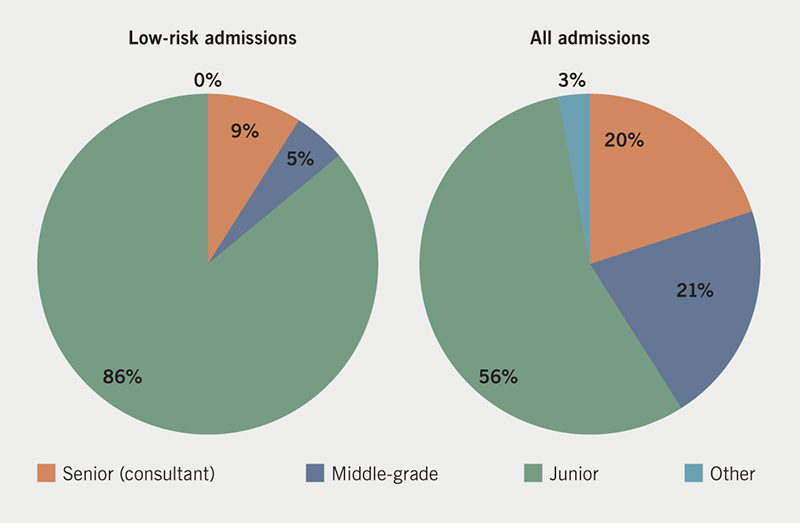
In the most recent data collection cycle, 21 patients assessed as low risk were admitted. Table 3 shows the reasons for admission recorded. Of the 21 low-risk patients who were admitted, 85% were seen initially by a junior doctor. Of all patients admitted with syncope, 56% were seen initially by a junior doctor (figure 3).
Discussion
Introduction of a syncope pathway has resulted in fewer admissions of low- and intermediate-risk patients with a reduction in length of stay and a saving of approximately 56 bed days per month (1.8/day). At £222/day (2016 costs) for an inpatient bed,9 this represents a significant potential cost saving. Even more importantly in this era of bed shortages, it is an opportunity to free up a scarce resource. It was noted that the cornerstone work up of syncope is suboptimal in some areas of unscheduled care, in particular in terms of postural blood pressure: 100% of those patients who attend RASCL will have a postural blood pressure, and ongoing education must continue in those referring areas. Twenty-one patients were admitted who were classed as low risk, with the majority being seen initially by relatively junior doctors. Whether this was due to lack of awareness of the pathway (with frequent staff rotations at these grades, this is quite likely), or cautiousness in these relatively inexperienced doctors, is unclear. Ensuring that these grades of doctor are informed about the pathway at the start of their rotation may help to reduce the admission rate even further.
Conclusion
We have achieved ongoing improvement in syncope management through the use of a pathway integrating front door teams with a specialist clinic. This has resulted in reduced admissions for low-risk patients, appropriate follow-up for intermediate-risk and reduced length of stay for those requiring admission.
Key messages
- The syncope service in Glasgow was redesigned, comprising: a risk-stratification pathway; a new referral process; and the availability of a rapid access syncope clinic
- The pathway allowed for risk stratification of patients into low, intermediate or high risk
- The pathway resulted in fewer admissions of low and intermediate risk patients, with a reduction in length of stay of those admitted and a saving of approximately 56 bed days per month
Conflicts of interest
None declared.
Funding
None.
Acknowledgements
We sincerely thank Dr John Byrne and Dr Brian Murphy (cardiology colleagues who co-designed the syncope pathway) and Dr Clare Smyth for her help with data collection.
Study approval and consent
None required.
References
1. Puppala VK, Dickinson O, Benditt DG. Syncope: classification and risk stratification. J Cardiol 2014;63:171–7. https://doi.org/10.1016/j.jjcc.2013.03.019
2. Chen LY, Shen WK, Mahoney DW, Jacobsen SJ, Rodeheffer RJ. Prevalence of syncope in a population aged more than 45 years. Am J Med 2006;119:1088.e1–1088.e7. https://doi.org/10.1016/j.amjmed.2006.01.029
3. Soteriades ES, Evans JC, Larson MG et al. Incidence and prognosis of syncope. N Engl J Med 2002;347:878–85. https://doi.org/10.1056/NEJMoa012407
4. Chen-Scarabelli C, Scarabelli TM. Neurocardiogenic syncope. BMJ 2004;329:336–41. https://doi.org/10.1136/bmj.329.7461.336
5. Alboni P, Brignole M, Menozzi C et al. Diagnostic value of history in patients with syncope with or without heart disease. J Am Coll Cardiol 2001;37:1921–8. https://doi.org/10.1016/S0735-1097(01)01241-4
6. Brignole M, Menozzi C, Bartoletti A et al. A new management of syncope: prospective systematic guideline-based evaluation of patients referred urgently to general hospitals. Eur Heart J 2006;27:76–82. https://doi.org/10.1093/eurheartj/ehi647
7. Brignole M, Moya A, de Lange FJ et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J 2018;39:1883–948. https://doi.org/10.1093/eurheartj/ehy037
8. Kenny RA, Brignole M, Dan GA et al. Syncope unit: rationale and requirement – the European Heart Rhythm Association position statement endorsed by the Heart Rhythm Society. Europace 2015;17:1325–40. https://doi.org/10.1093/europace/euv115
9. National Institute for Health and Care Excellence. Costing statement: implementing the NICE guideline on transition between inpatient hospital settings and community or care home settings for adults with social care needs. NG27. London: NICE, 2015. Available from: https://www.nice.org.uk/guidance/ng27/resources/costing-statement-2187244909
