COVID-19 and vaccine development
Trials in progress
At the time of writing there are more than 120 proposed vaccine approaches, seven of which are in clinical trial (Phase 1 or Phase1/2) and 70 or so in preclinical evaluation.1 Of those in clinical studies:
- two encode vectors where the surface S-protein of COVID-19 is incorporated into a non-replicating chimpanzee adenovirus vector (China and UK)
- two use a conventional inactivated whole virus (both China)
- two employ a messenger RNA vector encoding the S-protein (China and USA)
- one is a DNA vaccine (USA).
The time frames for each of these clinical trials varies from six months (the UK study at the University of Oxford with more than 1,000 subjects) to as far out as November 2021 (for one of two ‘inactivated virus’ Phase 1 studies in China). In June this year, Imperial College London will begin trials of a self-amplifying RNA construct containing the S-protein RNA sequence embedded in an RNA vector that allows continuous copying of the RNA.
Both the Oxford and Imperial trials have been funded by the UK government and while it will take time to establish efficacy the vaccine giant, The Serum Institute of India, has already agreed to begin manufacturing of millions of doses of the Oxford vaccine candidate in anticipation of a successful outcome. It will enter a combined PhaseII/III trial with around 5000 subjects in a month or so.
Expectations and uncertainties
The approach of most vaccine constructions is to present the surface S-protein to the immune system in the hope of either generating antibodies that block binding of COVID-19 to the receptor, ACE2, widely expressed in many cell types, or by inducing a robust cellular response, or both. Reduction of the viral load could then occur via antibody-mediated elimination, or by induction of adaptive cellular responses, ideally recognising early viral proteins before virus assembly and leading to lysis of virus producing cells.
The likely response to a vaccine, however, is made uncertain by current data from infected individuals who present a confusing immunological picture. For example, high neutralizing antibody status has been observed in older persons but in some younger persons who have experienced the same disease duration, low or sometimes undetectable antibody responses have been recorded, presenting a mechanistic conundrum.2 Is the virus assault in younger persons neutralised by innate immune cellular responses or via T-cells channelled towards an adaptive cellular response (CD8+) rather than through a humoral antibody (CD4+) response?
Where antibody responses have been seen, a further unknown is how long that immune response lasts, placing a great deal of uncertainty on the value of ‘immunity certificates’. With SARS-CoV, the immune response persisted for four to five months then began to drop steadily, whereas with MERS-CoV immunity appears to be have been much longer lived. No answers to these questions are yet available for COVID-19.
To add insult to injury, the rate of mutation (from copying errors) of the COVID-19 single strand RNA genome seems to be quite high. In a recent analysis of Wuhan patient virus samples, mutations were identified that in some instances resulted in virulence increases of up to 270 times using in vitro cell killing assays.3 A recent analysis that included COVID-19 samples from Belgium (non-peer reviewed)4 has suggested, worryingly, the emergence of a viral mutant that likely arose by recombination where two virus strains exchange sequence segments after simultaneous infection. If some of these mutations, by whatever mechanism, also generate immune escape mutants, vaccine development could become an even greater challenge than for influenza.
Truncated development timelines
Professor Sarah Gilbert (Professor Vaccinology, University of Oxford), who is leading the Oxford adenovirus vaccine study, has drawn attention to an obvious but critical issue with any shortened vaccine development programme. How do you assess efficacy in a clinical trial cohort where you cannot ethically expose the subjects to the virus post-vaccination? Even if that were permitted, it would be difficult in practice to measure efficacy in locations where there is a strict lockdown in place that prevents anything but incidental exposure. The most effective way of getting to an efficacy measure is via a longer-term Phase III trial where subjects post-vaccination, experience exposure during a naturally re-occurring COVID infection, always assuming it returns during the trial period. With such a requirement, the suggestion that vaccine availability may be a year or so away is not at all unreasonable and, even with such timing, would still be on an ‘extraordinarily truncated’ timeline. An alternative might be to carry out trials in geographical areas where the virus is at a much earlier stage of infection, a possibility being explored by the Oxford team.
But there are at least two other potentially problematic unknowns, among the many. The first will exercise the minds of those who have experience or knowledge of responses to the Dengue vaccine. Individuals who already have ‘non-neutralising’ anti-dengue antibodies (either from vaccination or a previous dengue infection), who then experience a further infection, may develop a serious haemorrhagic fever (DHF) that can be life-threatening. This antibody-dependent enhancement (ADE) is believed to be induced by non-neutralising antibody-dengue complexes that exacerbate the infection by pulling virus into cells via Fc receptors. We have no prior knowledge of whether an anti-COVID vaccine may follow a similar mechanistic route – similar although low frequency ADE was seen with SARS5 and pre-existing non-neutralising anti-SARS antibodies that cross-react with common epitopes on COVID-19, for example, would be candidates. Thus any clinical studies would need to tread with caution making safety an unquestionable priority.
A second, more complex question arises from observations during the 2003–2004 SARS pandemic that implicated interleukin 6 (IL6),6 an inducer of the Th17 cell differentiation and a potentially ‘bad’ cytokine known to be elevated during COVID-19 infection. If Th17 cells are activated by COVID-19 leading to eosinophil (and monocyte) extravasation from blood to lungs, a potential safety concern noted with first generation SARS vaccines based on viral vectors, then COVID-19 vaccine designs may need to evolve rapidly to bypass such undesirable mechanistic diversions if they are seen to occur.7
‘Non est vivere sed valere vita est’ (life is more than just staying alive).
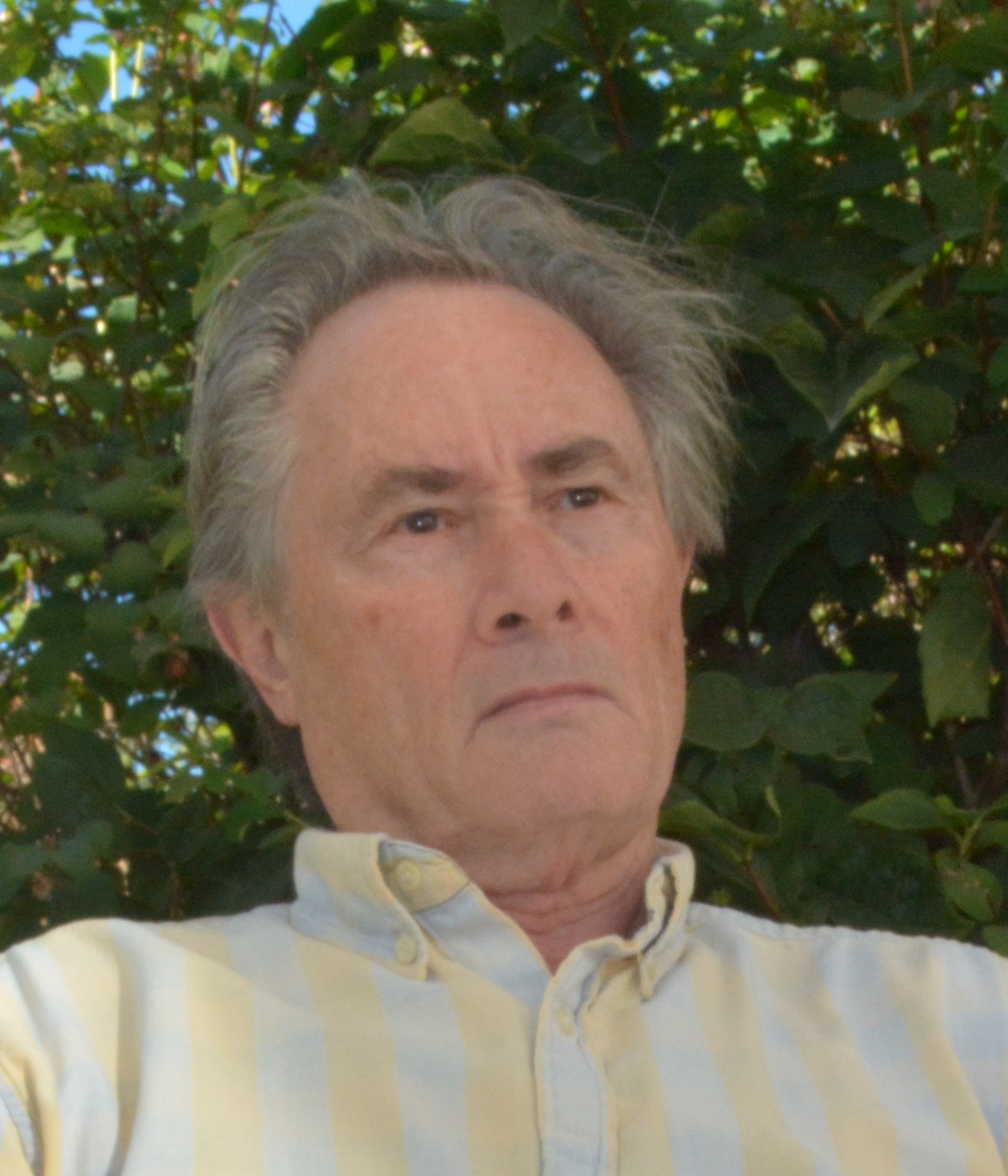
Professor Anthony Rees
Emeritus Professor and Rees Consulting AB
Uppsala, Sweden
(rees@reesconsultingab.com)
Professor Rees is author of The Antibody Molecule: From antitoxins to therapeutic antibodies (Oxford Medical Series, Oxford University Press, 2014). His new book A new history of vaccines will be published later this year.
References
- World Health Organization (WHO). Update on WHO Solidarity Trial – accelerating a safe and effective COVID-19 vaccine. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov/solidarity-trial-accelerating-a-safe-and-effective-covid-19-vaccine (last accessed 11th May 2020).
- Fan W, Wang A, Liu M et al. Neutralizing antibody responses to SARS-CoV-2 in a COVID-19 recovered patient cohort and their implications. medRxiv 2020 – preprint server for health sciences. https://doi.org/10.1101/2020.03.30.20047365 (last accessed 11th May 2020).
- Yao H, Lu X, Chen Q et al. Patient-derived mutations impact pathogenicity of SARS-CoV-2. medRxiv 2020 – preprint server for health sciences https://doi.org/10.1101/2020.04.14.20060160 (last accessed 11th May 2020).
- Korber B, Fischer WM, Gnanakaran S et al. Spike mutation pipeline reveals the emergence of a more transmissible form of SARS-CoV-2. bioRxiv 2020 – preprint servier for biology. https://doi.org/10.1101/2020.04.29.069054
- Yip MS, Cheung CY, Li PH et al. Investigation of antibody-dependent enhancement (ADE) of SARS coronavirus infection and its role in pathogenesis of SARS. BMC Proceedings 2011;5(Suppl 1):P80. https://doi.org/10.1186/1753-6561-5-S1-P80
- Zhang Y, Li J, Shan Y et al. Analysis of serum cytokines in patients with severe acute respiratory syndrome. Infect Immun 2004;72:4410-15. https://doi.org/0.1128/IAI.72.8.4410–4415.2004
- Hotez PJ, Corry DB, Bottazzi ME. COVID-19 vaccine design: the Janus face of immune enhancement. Nature Rev Immunol 2020 (published online 28 April 2020). https://doi.org/10.1038/s41577-020-0323-4
Expert report on COVID-19 and immunology research
An expert advisory group convened by The British Society for Immunology and the Academy of Medical Sciences has published a report COVID-19 and immunology research: what do we know and what are the research priorities?, which it calls “a rapid review of the relevant immunology research to help us understand how it can inform our response to the COVID-19 pandemic and the key research priorities we have identified for COVID-19 immunology research”.
It acknowledges that the the work in producing it was limited by the scant research that was currently available and the timeframes involved but it hopes the report will “summarise what we know, and what we do not, about the immunology of COVID-19, and set immunology research priorities”.
The report can be downloaded at: https://www.immunology.org/sites/default/files/Final_COVID-19_Immunology_report.pdf
Other articles from COVID-19 Bulletin 2:
- a review of current telemedicine platforms
COVID-19 and cardiorenal disease
- Diabetes UK position statement
- COVID-19 diagnostic glucose/lactate sensor in development
