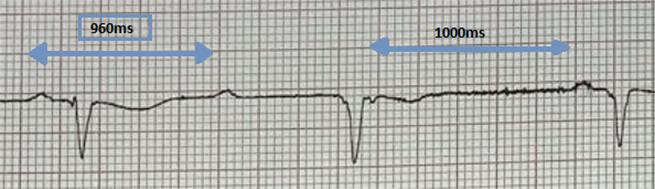
Ventriculophasic arrhythmia (VPA) is an intriguing electrocardiogram (ECG) phenomenon, often seen in patients with complete heart block, and could sometimes pose a challenging diagnostic dilemma for physicians. By definition, in VPA, the P–P intervals that contain a QRS complex are shorter than the P–P intervals that do not have a QRS complex. VPA is often a tell-tale ECG finding of complete heart block. We describe a case in which paroxysmal VPA led us to diagnose complete heart block.
Case
A 56-year-old man was referred from the emergency department for further evaluation of recurrent dizzy spells. The patient reported that he had intermittent episodes of palpitations associated with pre-syncope, but denied loss of consciousness. Additionally, he was feeling generally unwell and tired. There was no associated history of shortness of breath, chest pain, nausea, vomiting or sweating. Each episode of dizziness lasted for a few minutes and occurred both at rest and on exertion.
There was no history of recent viral infection, tinnitus, otalgia, or otorrhoea. There was no associated facial asymmetry, speech disturbance or sensory/motor symptoms. There was no travel history or any tick bites. There was no family history of cardiac problems, collapse, sudden cardiac death or early pacemaker insertion.
The patient was not on any regular medications and denied use of any illicit drugs. He used to smoke 10–15 cigarettes per day and consumed about 12 units of alcohol per week.
On clinical examination, the patient looked exhausted, lethargic and unwell. The rest of the general physical examination was unremarkable. His vitals were: blood pressure 100/60 mmHg, heart rate variable from 36–45 bpm, temperature 37.4°C, respiration rate 19 per minute, oxygen saturation of 96% on room air. Chest was clear and no murmurs found on auscultation. Jugular venous pressure was not distended and no hepato-jugular reflux demonstrated. There was no ankle oedema noted. Abdomen was soft and non-tender and no neurological deficit was elicited.
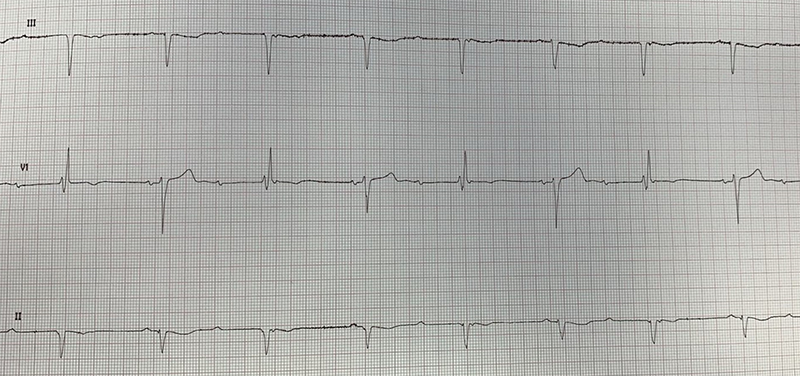
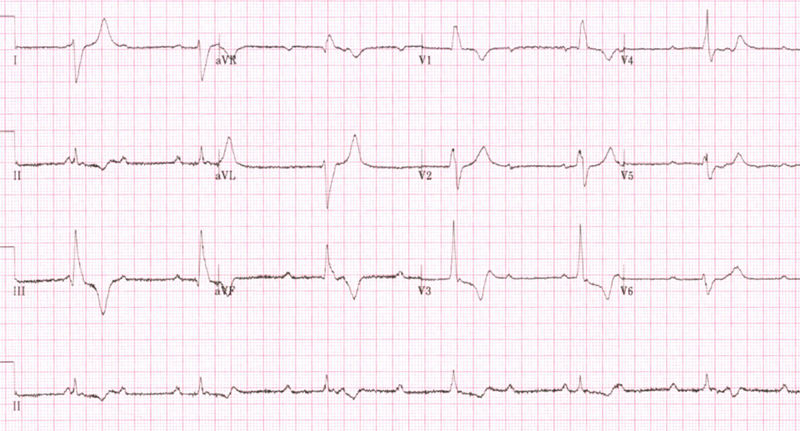
On arrival to the emergency department, electrocardiogram (ECG) demonstrated paroxysmal ventriculophasic arrhythmia (figure 1). The patient was admitted to the cardiology ward and monitored on telemetry, which further demonstrated complete heart block (figure 2). The patient was referred to the cardiology device team and a dual-chamber pacemaker (DDD-R) was inserted the same day without any overt complication. The patient symptomatically improved and was discharged the next day with regular pacemaker clinic follow-up.
Discussion
Ventriculophasic arrhythmia (VPA) is described as a phasic variation of P–P interval with and without QRS.1 In this phenomenon, the P–P interval with QRS complexes are shorter as compared with the P–P intervals without QRS complexes (figure 3). Approximately, 30% of cases with complete atrioventricular (AV) block are associated with VPA. Complete heart block (CHB), is an abnormal heart rhythm resulting from a defect in the cardiac conduction system in which there is no conduction through the atrioventricular node (AVN), leading to complete dissociation of the atria and ventricles.2,3
The mechanism of VPA is still not fully understood. Rosenbaum and Lepeschkin proposed the most plausible explanation as two phase chronotropic effects.4 The positive chronotropic effect results in an early appearance of a P-wave following the QRS complex, which in turn causes shortening of the P–P interval that contains a QRS complex.
Two potential mechanisms have been proposed regarding the positive chronotropic effect. First, atrial stretch caused by the mechanical effects of ventricular systole may expedite the discharge of impulses from a normal sinus node. Second, as a result of ventricular contraction, blood supply to the sinus node improves, which in response leads to an earlier sinus node discharge and a P-wave following the QRS complex.5,6 On the contrary, due to a negative chronotropic effect, it may result in lengthening of the next P–P interval without an intervening QRS complex. A plausible explanation for a negative chronotropic effect involves arterial baroreceptor-mediated changes in vagal tone.
Conclusion
Ventriculophasic arrhythmia is a common, but probably under-appreciated finding, associated with one-third of the patients with complete heart block. Several mechanisms have been postulated but no clear explanation has been agreed upon. The clinical significance of ventriculophasic arrhythmias depends largely upon the underlying cardiac status and rhythm disorders.
Conflicts of interest
None declared.
Funding
None.
Patient consent
The patient provided written consent for publication. All attempts were made to ensure patient confidentiality was maintained.
References
1. Chung EK. A reappraisal of ventriculophasic sinus arrhythmia. Jpn Heart J 1971;12:401–04. https://doi.org/10.1536/ihj.12.401
2. Narula OS, Scherlag BJ, Javier RP, Hildner FJ, Samet P. Analysis of the A-V conduction defect in complete heart block utilizing His bundle electrograms. Circulation 1970;41:437–48. https://doi.org/10.1161/01.CIR.41.3.437
3. Kashou AH, Goyal A, Nguyen T, Chhabra L. Atrioventricular block. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2020. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459147/
4. Rosenbaum MB, Lepeschkin E. The effect of ventricular systole on auricular rhythm in auriculoventricular block. Circulation 1955;11:240–61. https://doi.org/10.1161/01.CIR.11.2.240
5. Hashimoto K, Tanaka S, Hirata M, Chiba S. Responses of the sinoatrial node to change in pressure in the sinus node artery. Circ Res 1967;21:297–304. https://doi.org/10.1161/01.RES.21.3.297
6. De Marchena E, Colvin-Adams M, Esnard J, Ridha M, Castellanos A, Myerburg RJ. Ventriculophasic sinus arrhythmia in the orthotopic transplanted heart: mechanism of disease revisited. Int J Cardiol 2003;91:71–4. https://doi.org/10.1016/S0167-5273(02)00597-1
