This is an interesting case of wide complex tachycardia in a patient on flecainide for paroxysmal atrial fibrillation. Diagnostic possibilities were discussed, actual diagnosis revealed, and explanation provided.

Case
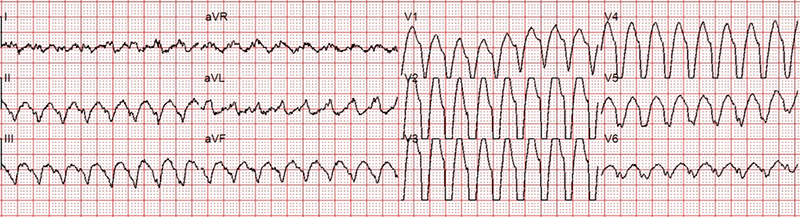
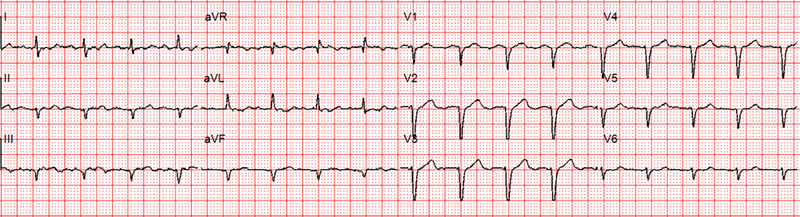
A 65-year-old woman called an ambulance for episodes of palpitation, chest pain and dizziness over the previous three to four days. She was known to suffer from paroxysmal atrial fibrillation (AF) for a while and was on flecainide 100 mg twice daily and rivaroxaban. She thought that the present palpitations were different from her usual occasional paroxysms of AF. Her echocardiogram in the past showed structurally normal heart with preserved left ventricular function. Her coronary angiogram five years ago showed normal coronary arteries. Ambulance crew recorded two electrocardiograms (ECGs) over a period of 20 minutes. The first ECG was done during palpitation (figure 1) and the second ECG when she felt better (figure 2).
Discussion
This is a wide complex tachycardia at a rate of about 200 beats per minute. One needs to consider three differential diagnoses in all cases of regular wide complex tachycardia:
- Ventricular tachycardia (VT).
- Supraventricular tachycardia (SVT) with aberrancy.
- Antidromic atrioventricular re-entry tachycardia (AVRT).
Antidromic AVRT is very unlikely here because there is no history of regular tachycardia in the past and the second ECG (when QRS complexes are narrow) does not show pre-excitation.
VT is a definite possibility. The point against VT is absence of any substrate (no structural and functional heart disease, echocardiogram and coronary angiogram were normal). Flecainide itself though can cause VT in a structurally normal heart by slowing conduction and creating functional block and, hence, promoting re-entry. There are many case reports of flecainide-induced ventricular arrhythmias.1,2
The diagnosis here is SVT with aberrancy, more specifically atrial flutter with 1:1 AV conduction with aberrancy (left-bundle branch block [LBBB] pattern). The points in favour are:
- Flecainide is known to cause this arrhythmia.
- Flecainide can convert AF into a more organised rhythm of atrial flutter.
- The atrial rate of this flutter is slow because of flecainide. (Usually the atrial rate in flutter is around 250–350 but here the atrial rate of flutter is 200).
- As the flutter rate is slow it can conduct 1:1 through the atrioventricular (AV) node. In terms of aberrancy there is possibly LBBB, but we know that flecainide can also cause QRS prolongation by prolonging intramyocardial conduction and this effect happens more at high heart rate (use dependence).
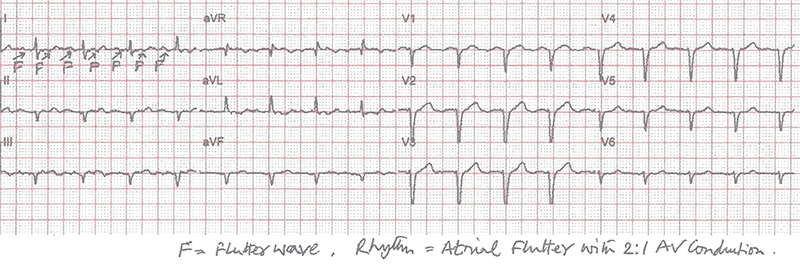
- And, most importantly, in the next ECG the arrhythmia spontaneously goes into 2:1 AV conduction (ventricular rate becomes exactly half of what it was in the previous ECG) and QRS becomes narrow proving that the initial rhythm was atrial flutter with broad QRS and not VT (figure 3).
Flecainide is known to cause this problem, particularly when it is used on its own for paroxysmal AF. The reported incidence is around 3.5–5%.3 Many cardiologists, hence, prefer to combine beta blocker with flecainide to treat paroxysmal AF. This normally prevents rapid conduction through the AV node if flecainide induces slow flutter.
This patient’s flecainide was stopped after this, and she was commenced on bisoprolol. The options of other anti-arrhythmics (sotalol, amiodarone) and AF ablation were discussed. She was not keen for AF ablation and has been doing reasonably well on bisoprolol for the moment.
Key messages
- Slow atrial flutter with 1:1 atrioventricular (AV) conduction can present as either narrow or wide complex tachycardia
- Flecainide used for atrial fibrillation can cause slow atrial flutter, which can conduct 1:1 through the AV node
- Medication to slow down AV conduction can be co-administered with flecainide to prevent a rapid ventricular rate
Conflicts of interest
None declared.
Funding
None.
Patient consent
Written consent for publication was obtained from the patient.
References
1. Banavalikar B, Shenthar J, Padmanabhan D. Unusual wide complex tachycardia during rhythm control for atrial fibrillation. Circulation 2018;138:537–9. https://doi.org/10.1161/CIRCULATIONAHA.118.036071
2. Watts TE, McElderry HT, Kay GN. An irregular wide complex tachycardia. Circulation 2017;136:773–5. https://doi.org/10.1161/CIRCULATIONAHA.117.029974
3. Andrikopoulos GK, Pastromas S, Tzeis S. Flecainide: current status and perspectives in arrhythmia management. World J Cardiol 2015;7:76–85. https://doi.org/10.4330/wjc.v7.i2.76
