Aortic dissection is a rare and potentially fatal complication of coronary angiography. We report a case of a woman in her late 80s who underwent a left femoral approach coronary angiogram for evaluation of a transcatheter aortic valve replacement (TAVR). Following the procedure, she had a cardiac arrest and was found to have a descending aortic dissection on transoesophageal echocardiogram. Autopsy showed an acute intimal tear of the descending aorta, most likely related to catheter manipulation. Patients undergoing evaluation for TAVR, who tend to be elderly with concomitant atherosclerosis, are at risk for complications following cardiac catheterisation including aortic dissection.
Case
A woman in her late 80s with a past medical history of severe aortic stenosis, rheumatic fever, coronary artery disease with prior myocardial infarction, and atrial flutter, presented with worsening shortness of breath, chest pain and near syncope. Prior to presentation she was undergoing evaluation for transcatheter aortic valve replacement (TAVR). Given the escalation of her symptoms, she was admitted for expedited evaluation.
Upon admission, she was haemodynamically stable with a harsh systolic murmur. As a prelude to TAVR, coronary angiography was performed. The angiogram was technically challenging due to heavily calcified and tortuous vessels throughout the iliac vessels and aorta. Ultimately, a left femoral approach was required and a drug-eluting stent was successfully placed in the left anterior descending artery. Ten hours after the procedure, she experienced severe abdominal pain radiating to her back and went into pulseless electrical activity (PEA) arrest. Return of spontaneous circulation was obtained after cardiopulmonary resuscitation and epinephrine. Minutes later, she experienced a second PEA arrest. Emergent bedside transoesophageal echocardiogram (TOE) revealed a descending aortic dissection and rupture. Given prolonged resuscitation and lack of cardiac activity on TOE, further heroic efforts were felt to be futile.
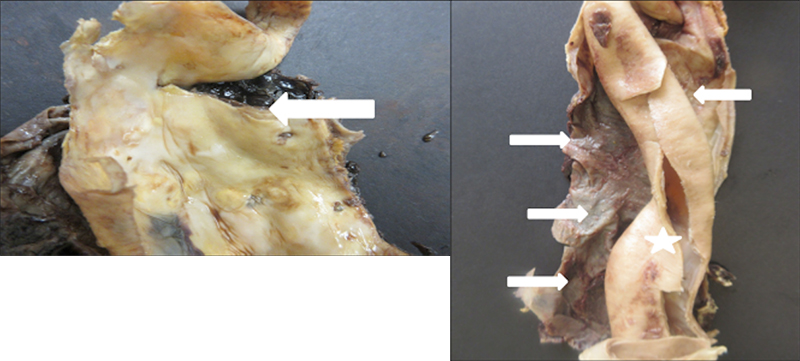
The patient’s autopsy demonstrated mild-to-moderate atherosclerosis throughout the aorta with an acute intimal tear originating in the descending aorta progressing antegrade to the iliac vessels and retrograde to the descending aortic arch. Adventitial haemorrhage and rupture was identified adjacent to the origination of the dissection (figure 1).
Discussion
Aortic dissection is an uncommon, yet known and potentially fatal complication of cardiac catheterisation. The European Society of Cardiology (ESC) aorta guidelines describe a risk of iatrogenic aortic dissection (IAD) following coronary angiography of less than four per 10,000 and less than two per 1,000 after percutaneous coronary intervention (PCI).1 Data from the Society for Thoracic Surgeons and American College of Cardiology TAVR registry demonstrated a risk of IAD following TAVR of four per 1,000.2 The most commonly reported location for dissection involves the abdominal aorta related to catheter manipulation, although extension from the coronary arteries into the ascending aorta can also occur.1 In a series of IAD from the International Registry of Acute Aortic Dissection, 88% of those with type B aortic dissection had prior catheterisation. Compared with spontaneous aortic dissection, the iatrogenic cases were older, more likely to have atherosclerosis and to present with indolent haemodynamic instability, and carried mortality which was significantly higher than spontaneous type B aortic dissection.3
Guidelines for management of IAD are lacking due to the rarity of the complication, but ESC aortic guidelines suggest a conservative approach may be appropriate in the majority of cases, particularly with dissections affecting the abdominal aorta.1
Conclusion
The dissection in this case, likely, was related to catheter manipulation and trauma of the subintimal space in the setting of a heavily atherosclerotic aorta. If significant atherosclerosis is identified in the descending aorta pre-procedure, a radial approach for angiography may be preferable. However, transfemoral access is preferred in TAVR, and, as the patient population is often elderly with concomitant atherosclerosis, this group remains at risk for complications. Aortic dissection should be considered if new significant chest, back or abdominal pain develops, particularly with haemodynamic instability, after cardiac catheterisation.
Key messages
- Iatrogenic aortic dissection (IAD) related to cardiac catheterisation most frequently occurs in the abdominal aorta. IAD may present with haemodynamic instability and carries significant mortality
- Elderly patients with significant atherosclerosis are at increased risk for IAD and therefore patients undergoing transthoracic aortic valve replacement (TAVR) may be at risk for this complication
Conflicts of interest
None declared.
Funding
None.
Patient consent
Consent for publication was obtained from the next of kin.
References
1. Erbel R, Aboyans V, Boileau C et al. 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. Eur Heart J 2014;35:2873–926. https://doi.org/10.1093/eurheartj/ehu281
2. Holmes D, Nishimura R, Grover F et al. Annual outcomes with transcatheter valve therapy: from the STS/ACC TVT registry. J Am Coll Cardiol 2015;66:2813–23. https://doi.org/10.1016/j.jacc.2015.10.021
3. Januzzi J, Sabatine M, Eagle K et al. Iatrogenic aortic dissection. Am J Cardiol 2002;89:623–5. https://doi.org/10.1016/S0002-9149(01)02312-8
