High-output heart failure (HF) is an uncommon condition. This occurs when HF syndrome patients have a cardiac output higher than eight litres per minute. Shunts, such as fistulas and arteriovenous malformations are an important reversible cause. We present the case of a 30-year-old man who presented to the emergency department due to decompensated HF. Echocardiogram showed dilated myocardiopathy with high cardiac output (19.5 L/min calculated on long-axis view). He was diagnosed with arteriovenous malformation by computed tomography (CT) and subsequent angiography, and a multi-disciplinary team decided to perform endovascular embolisation with ethylene vinyl alcohol/dimethyl sulfoxide at different times. The transthoracic echocardiogram showed a significant decrease in cardiac output (9.8 L/min) and his general condition improved significantly.
Introduction
High-output heart failure (HF) is an uncommon condition with varying aetiologies, often left uninvestigated. This type of HF is characterised by an elevated cardiac output, usually with high stroke volume, leading to biventricular dilation. According to a Mayo Clinic series involving 120 patients with high-output HF diagnosed between 2000 and 2014, the most important causes included obesity, liver cirrhosis, chronic obstructive pulmonary disease, and shunting, such as fistulas or arteriovenous malformations.1
Case report
A 30-year-old man presented to the emergency department for dyspnoea, abdominal distention, and oedema lasting 20 days. He had a history of thyroid medullar carcinoma, diagnosed 11 years ago, and treated with surgery and oral chemotherapy with sorafenib without subsequent follow-up.
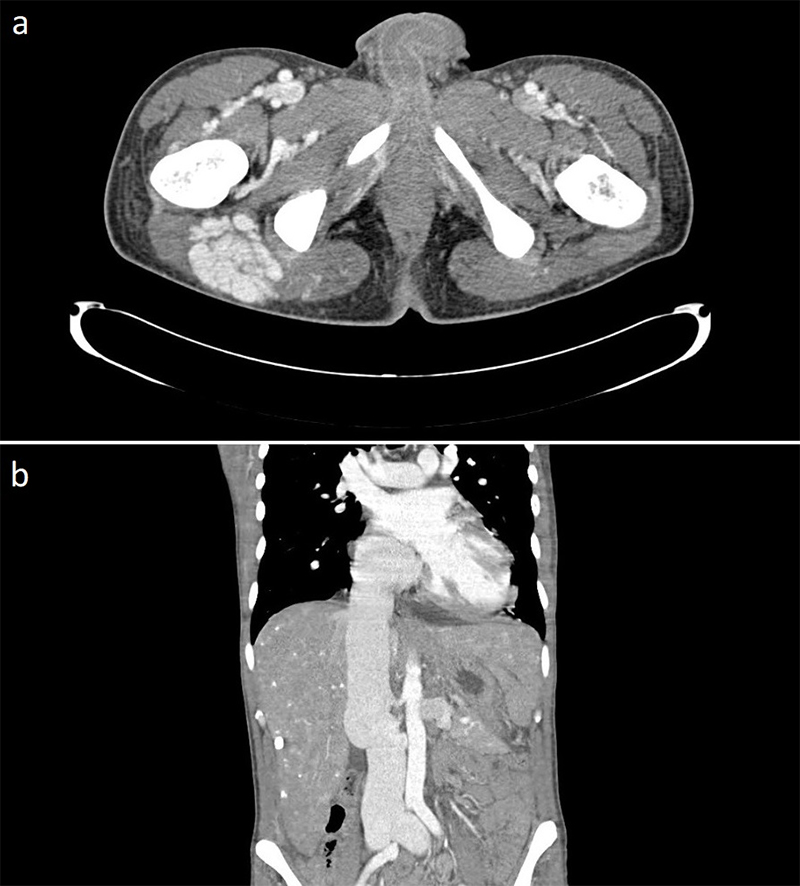
On admission, he had a blood pressure of 155/95 mmHg, a heart rate of 107 bpm, and a respiratory rate of 30 breaths per minute. The patient was afebrile with an oxygen saturation of 96%. Cardiovascular examination revealed a 3/6 systolic murmur in the mesocardium. He presented with jugular vein distention that was not collapsible, bipedal oedema reaching the upper thigh, and marked hepatomegaly palpable up to the right iliac fossa. The chest X-ray showed cardiomegaly. His N-terminal pro-B-type natriuretic peptide (NT-proBNP) measured 950 pg/ml, while his calcitonin level was higher than 2,000 pg/ml, thyroid stimulating hormone (TSH) of 9.4 mU/ml with free T4 of 0.88 ng/dL. The bedside echocardiogram showed dilated myocardiopathy with preserved biventricular systolic function (61% by biplane method) with left ventricular end diastolic diameter of 6.4 cm, severe tricuspid regurgitation and cardiac output calculated on long-axis view of 19.5 L/min. A computed tomography (CT) scan ruled out pulmonary thromboembolism, and identified bilateral ectasia of the pulmonary artery branches, severely dilated inferior vena cava, multiple lithic metastatic-type lesions in the cervical and dorsal vertebral bodies, and a large right pelvic arteriovenous malformation (AVM) (figure 1). In order to rule out other possible aetiologies of dilated cardiomyopathy, a cardiac magnetic resonance imaging (MRI) perfusion scan was performed without signs of ischaemia and absence of late gadolinium enhancement.
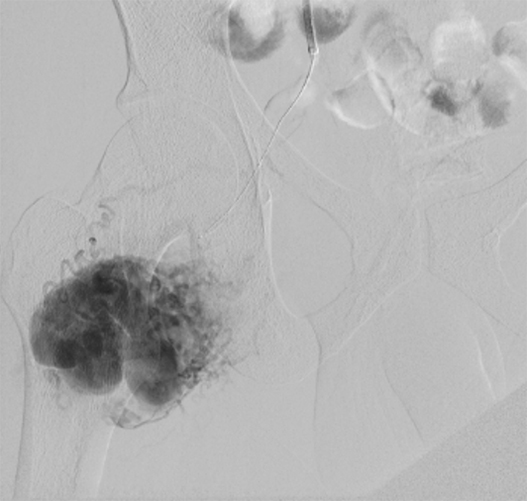
Bone biopsy revealed poorly differentiated neoplasia infiltration. The immunohistochemistry confirmed the metastatic origin of the thyroid medullar carcinoma. Aortic–iliac–femoral Doppler ultrasound demonstrated a flow compatible with AVM. A bibliographic review was carried out and the case was discussed by a multi-disciplinary team, before deciding to make a diagnostic arteriography. Right pelvic AVM tributary branches (hypogastric, upper gluteal, and superficial femoral) and a smaller contralateral AVM were identified (figure 2).
A right AVM embolisation through the left femoral artery (7 French access) was performed with a micro-catheter for the selective injection of ethylene vinyl alcohol/dimethyl sulfoxide. The control angiography at the end showed the material correctly distributed without complications.
Subsequently, the patient was admitted to the coronary unit due to decompensated HF. We initiated treatment with endovenous diuretics, but the patient responded poorly. He developed oliguria and dyspnoea, so right heart catheterisation was performed. It revealed a cardiac output of 18 L/min with a pulmonary wedge pressure of 24 mmHg and central venous pressure of 20 mmHg. Triple diuretic treatment was prescribed, eliciting an improved response. A new arteriography ruled out complications related to the procedure and showed the persistence of tributary branches with residual AVM.
Four endovascular procedures were successfully carried out. The transthoracic echocardiogram (seven days after the last procedure) showed a significant decrease in cardiac output (9.8 L/min). The patient’s decompensated HF symptoms disappeared, and his general condition improved significantly. Chemotherapy for his underlying disease was then planned.
Discussion
HF is characterised by a normal or low cardiac output, associated with increased
left-ventricle filling pressures.2 However, some HF syndrome patients present with a high output. This includes HF patients with a cardiac output higher than eight litres or 3.0 L/min/m2.3
High-output HF may be classified under two main categories:
- Rise in body oxygen consumption due to increased metabolic demand
- Low systemic vascular resistance due to peripheral vasodilation or arteriovenous shunting.
In the latter, the arteries and veins are tangled and form direct connections, bypassing normal tissues. In the second group, the shunt may be caused by arteriovenous fistulas in patients undergoing haemodialysis, or isolated AVMs, which may be congenital, post-traumatic, iatrogenic, or syndromic, particularly hereditary haemorrhagic telangiectasia.4
As seen in this case, the diagnosis is not straightforward. In most instances, various imaging tools are necessary to diagnose high-output HF and the aetiologic cause. Specifically, in this case, an echocardiogram, CT and cardiac MRI were performed in order to arrive at the diagnosis and to the aetiologic cause. About the AVM, the patient had no history of interventions or any other history to consider an iatrogenic or traumatic cause for AVM. He was not on haemodialysis, nor did he meet the clinical criteria for diagnosing hereditary haemorrhagic telangiectasia or other apparent cause, therefore, it should be considered congenital. Since high-output HF is not frequent, nor is it usual to consider it initially, diagnosis is often late. For this reason, thinking about the possibility of it is essential.
To conclude, patients with high-output HF secondary to extended AVM have been treated with different techniques, including embolisation through arterial catheterisation, stent placement with sclerotherapy, and surgical closure in selected cases.5 No treatment was reportedly better than the others. The treatment is individualised and decided by the multi-disciplinary team.
Conflicts of interest
None declared.
Funding
Research Committee, Allende Sanatorium.
Consent
The patient, in his full capacity, gave informed consent for the report of this case for educational and scientific purposes.
References
1. Reddy YNV, Melenovsky V, Redfield MM et al. High-output heart failure: a 15-year experience. J Am Coll Cardiol 2016;68:473–82. https://doi.org/10.1016/j.jacc.2016.05.043
2. Murphy SP, Ibrahim NE, Januzzi JL. Heart failure with reduced ejection fraction: a review. JAMA 2020;324:488–504. https://doi.org/10.1001/jama.2020.10262
3. Mehta PA, Dubrey SW. High output heart failure. QJM 2009;102:235–41. https://doi.org/10.1093/qjmed/hcn147
4. Koyalakonda SP, Pyatt J. High output heart failure caused by a large pelvic arteriovenous malformation. JRSM Short Rep 2011;2:66. https://doi.org/10.1258/shorts.2011.011057
5. Okada M, Kato M, Uchida K et al. Transcatheter and percutaneous procedures for huge pelvic arteriovenous malformations causing high-output heart failure. J Cardiol Cases 2015;12:162–5. https://doi.org/10.1016/j.jccase.2015.07.001
