To review the utility of cardiovascular magnetic resonance (CMR) in the management of hospital inpatients, we performed a retrospective review of all inpatient CMR scans performed over a six-month period at a tertiary referral cardiology centre. Patient demographics, indication for CMR imaging, results of the CMR scans and whether the results changed patient management were recorded. Change in management included medication changes, subsequent invasive procedures, or avoidance of such, and hospital discharge.
Overall, 169 patients were included in the study cohort, 66% were male, mean age was 57.1 years. The most common indication for inpatient CMR was to investigate for cardiomyopathy (53% of patients). The most prevalent diagnosis post-CMR in our cohort was ischaemic heart disease, including ischaemic cardiomyopathy and coronary artery disease. There was a complete change in diagnosis or additional diagnosis found in 29% of patients following CMR. Overall, inpatient CMR led to a change in management in 77% of patients; the most common being changes to medication regimen. CMR was well tolerated in 99% of patients and image quality was diagnostic in 93% of cine scans performed.
In conclusion, CMR is vital for the management of cardiology inpatients, having an impact that is at least as significant as in the management of outpatients.
Introduction
Cardiovascular magnetic resonance (CMR) is an advanced cardiac imaging modality indicated in the assessment of most common cardiology conditions.1 It is a technique that has become increasingly accessible and utilised in clinical practice. CMR is the gold standard in assessing cardiac chamber volume and function with infinite imaging planes, and is not restricted by body habitus, in contrast to transthoracic echocardiography.2 It also allows the non-invasive assessment of the myocardium through tissue characterisation with delayed enhancement following gadolinium-based contrast agents, and more contemporary techniques, such as parametric tissue mapping.3 Myocardial perfusion can also be assessed with CMR and has been shown to be superior to other non-invasive techniques, such as single-photon emission computed tomography (SPECT), with the additional advantage of using non-ionising radiation.4 Given these advantages, CMR is an extremely versatile imaging modality and has an important role in the clinical investigation of cardiomyopathies, ischaemic heart disease and myocarditis.5
The European CMR (EuroCMR) registry reviewed the indications, safety and impact of routine CMR on patient management on a multi-centre and multi-national scale in over 27,000 patients. The study demonstrated that routine CMR is highly impactful on patient management, particularly in the risk stratification of suspected coronary artery disease (CAD) or ischaemia, viability assessment, and in the investigation of cardiomyopathies.6 CMR has been predominantly used in the assessment of stable outpatients, but its increasing availability and clinical utility has resulted in increased inpatient referrals. The EuroCMR registry did not specifically review the utility of CMR for inpatients. Given the unique characteristics of CMR, we hypothesised its clinical use in the acute setting would be highly impactful on inpatient care.
In this single UK tertiary centre study, we sought to evaluate inpatient CMR and whether it similarly impacts patient management as was shown in the EuroCMR registry. Furthermore, as inpatients are often of higher acuity and clinically unstable compared with outpatients, we also aimed to evaluate image quality to see whether high-quality studies can be obtained in this cohort.
Materials and method
This was a clinical audit (AUDI002142) performed at St. George’s Hospital University Hospitals NHS Foundation Trust, London, UK, and, as such, external ethics were not required. We identified all inpatients who had a CMR scan between June and December 2021 at our tertiary referral centre. Scans were performed on a 3 Tesla (T) Phillips Achieva or a 1.5T Siemens Avanto scanner. Data were collected and analysed retrospectively from the electronic notes and imaging reports using a standardised proforma. We included patient demographics, known cardiac comorbidities, including hypertension, ischaemic heart disease, heart failure and atrial fibrillation, and the indication for scan as per the request details. We recorded suspected diagnosis prior to CMR and the subsequent diagnoses made following the scan. We reviewed whether the diagnosis changed following CMR and any other diagnoses made in the event of multiple findings. Change in management was defined as a change in pharmacological therapy (initiation or cessation of treatment), further procedure(s) performed as a consequence of the CMR results, and, conversely, whether the CMR prevented further invasive tests (such as coronary angiography). The data collection was performed using the same terminology as described in the EuroCMR registry to allow comparison. Consultant cardiologists with more than five years’ experience in CMR reported all scans.
Image quality
The quality of the steady-state free-precession (SSFP) cines and delayed enhancement imaging were assessed by a Level 3 EACVI accredited operator with more than five years’ experience in CMR (KDK). Image quality of the cines were rated as good, adequate, or poor. Good was deemed high-quality short-axis and long-axis images with no significant artefact. Adequate, limited artefact but still able to measure cardiac volumes with a high degree of confidence. Poor was deemed insufficient quality to measure cardiac volumes to obtain a reliable ejection fraction. The delayed enhancement images were also rated good, adequate or poor. Similar to the cines, good included studies with long- and short-axis images with no significant artefact and adequate included studies with, limited artefact but still able to make a clinical diagnosis with a high degree of confidence. Poor images were non-diagnostic.
Table 1. Baseline patient demographics
| Number | % | |
|---|---|---|
| Gender | ||
| Male | 112 | 66% |
| Female | 57 | 34% |
| Age, years | ||
| <21 | 9 | 5% |
| 21–40 | 28 | 17% |
| 41–60 | 51 | 30% |
| 61–80 | 68 | 41% |
| >80 | 13 | 8% |
| Cardiac history | ||
| Hypertension | 57 | 34% |
| Ischaemic heart disease | 30 | 18% |
| Heart failure | 23 | 14% |
| Atrial fibrillation | 18 | 11% |
| Valvular heart disease | 10 | 6% |
| Nil known | 69 | 41% |
Results
In total, 169 patients were included in this study (baseline patient demographics are included in table 1). The majority of patients were male (66% patients). Mean age was 57.1 ± 19.0 years. The most common pre-existing cardiac conditions were hypertension (34%) and known ischaemic heart disease (18%). The median time from electronic request to scan completion was two days (range 0–11 days) and the median time from scan to hospital discharge was four days (range 0–97 days).
The most common reasons for admission to hospital were chest pain (32%), dyspnoea (14%) and syncope (13%). There were 13% of patients admitted post-cardiac arrest. The primary indication for inpatient CMR was to investigate for cardiomyopathy (53%), including the assessment of left ventricular systolic dysfunction (LVSD) and inherited cardiac conditions, such as hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM), amyloid and arrhythmogenic cardiomyopathy (AVC) (table 2). Overall, 17% of scans performed were to assess myocardial viability and the indication in 12% of scans was to further evaluate suspected CAD.
Table 2. Primary indication for cardiovascular magnetic resonance (CMR) scan
| Indication | N | % |
|---|---|---|
| Cardiomyopathy | 89 | 53% |
| Viability | 29 | 17% |
| Suspected CAD | 21 | 12% |
| Assessment post-cardiac arrest | 15 | 9% |
| Myocarditis | 11 | 7% |
| Other | 4 | 2% |
| Key: CAD = coronary artery disease | ||
The most common diagnosis following CMR imaging was CAD, including myocardial infarction and ischaemic cardiomyopathy (ICM). Non-ischaemic cardiomyopathy (NICM) including, for example, DCM, hypertensive heart disease and tachycardia-mediated cardiomyopathy was diagnosed in 23% patients (table 3). HCM and infiltrative cardiomyopathies were reported in 12% of scans included in this cohort. Myocarditis was detected in 11% of scans. Of note, 12% of scans performed were normal.
Table 3. Diagnosis following inpatient CMR
| Diagnosis post-CMR | N | % |
|---|---|---|
| Cardiomyopathy | 21 | 12% |
| NICM | 39 | 23% |
| ICM/CAD | 58 | 34% |
| Myocarditis | 18 | 11% |
| Thrombus | 5 | 3% |
| Pericardial disease | 5 | 3% |
| Note: Cardiomyopathy in this study refers to hypertrophic cardiomyopathy and infiltrative conditions, such as amyloid and cardiac sarcoid Key: NICM = non-ischaemic cardiomyopathy – including dilated cardiomyopathy, hypertensive cardiomyopathy and tachycardia-induced cardiomyopathies; ICM = ischaemic cardiomyopathy; CAD = coronary artery disease |
||
Impact of CMR on patient management
Inpatient CMR led to a new or additional diagnosis in 29% patients (figure 1). In four patients there was a new finding of left ventricular (LV) thrombus. Overall, CMR performed on inpatients impacted clinical management in 77% (130/169) of patients. Most commonly this was a change in pharmacological therapy, which occurred in a total of 54 (32%) patients. A proportion of patients had an invasive procedure, such as cardiac device implantation or coronary angiography following the result of the CMR scan (28% patients). Inpatient CMR led to the avoidance of undertaking further procedures in 11 (7%) patients – predominantly avoiding left heart catheterisation (LHC) in cases with no myocardial viability demonstrated on CMR. Further investigations as a result of the CMR findings were requested in 12 (7%) patients. This included non-invasive tests, such as computed tomography (CT) imaging, genetic testing or electrophysiology tests. The outcome of CMR facilitated patient discharge from hospital in 23 (14%) patients (figure 2).
Image quality and safety profile of CMR
The majority (88%) of scans were performed at 3T with only 12% scans performed at 1.5T. Image quality was diagnostic (good or adequate) in 93% of cine scans and in 87% of scans with late gadolinium enhancement (LGE). Overall, image quality of the cines was good in 67%, adequate in 26% and poor in 5% of patients. For the LGE images, 59% of scans were good, 28% adequate and 6% poor (table 4). In terms of patient acceptability and safety profile of inpatient CMR, 99% scans were well tolerated: two patients did not tolerate the scan, this was due to anxiety during the scan in one case and claustrophobia in the second case, and one patient was unable to proceed due to raised body mass index. There was one case of contrast extravasation.
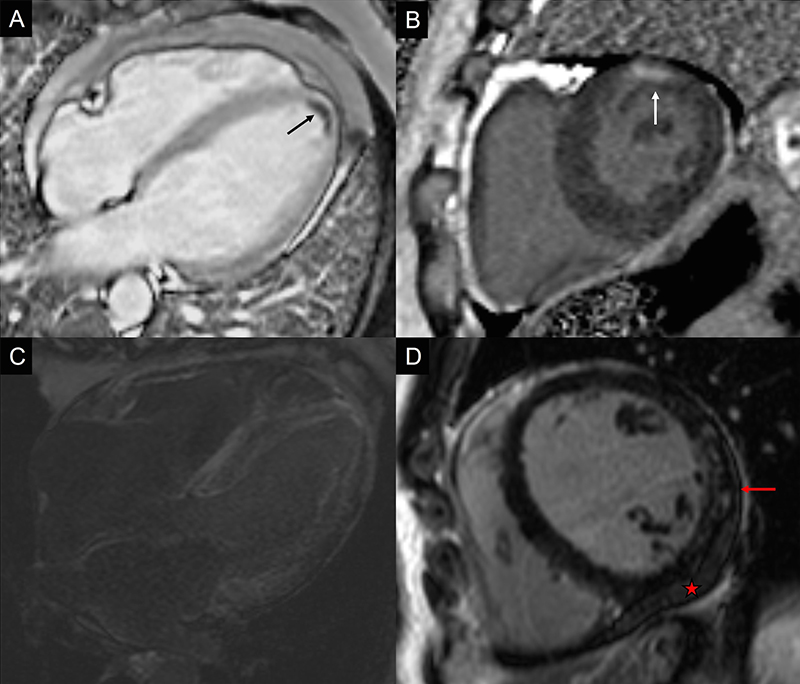
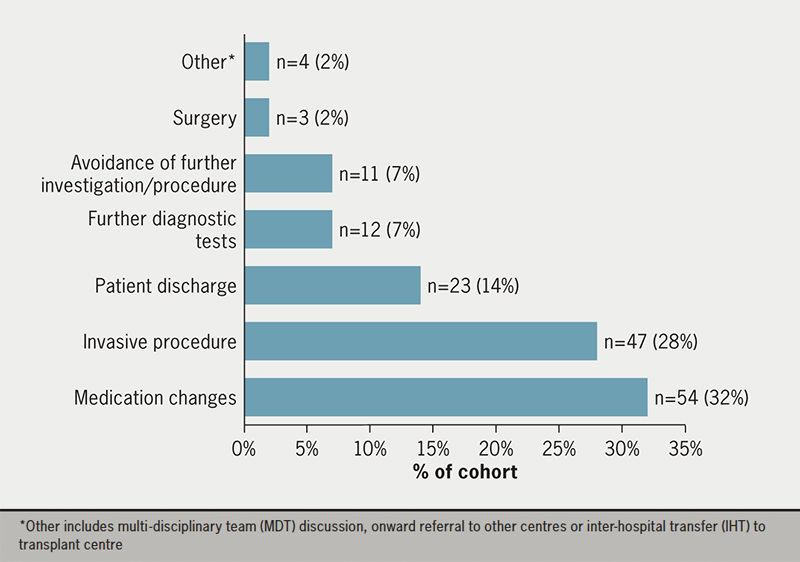
Table 4. CMR scan image quality
| Image quality | Cine % (n) |
LGE % (n) |
|---|---|---|
| Good | 67% (114) | 59% (100) |
| Adequate | 26% (44) | 28% (48) |
| Poor | 5% (8) | 6% (10) |
| No images | 2% (3) | 7% (11) |
| Key: LGE = late gadolinium enhancement | ||
Discussion
In this study we have shown that CMR is crucial for inpatient management in tertiary cardiac centres with 77% of studies resulting in a change in management. To the best of our knowledge, this study is the first to specifically look at inpatient scans and the subsequent impact on patient care.
There were several key findings relating to the indication for CMR, CMR outcomes and consequent impact on patient management worth further discussion. The most common indication in our cohort was to investigate for cardiomyopathy, whereas in the EuroCMR registry, CMR was most commonly used to assess ischaemia. Several reasons for this variance are likely. First, inpatients with troponin-positive events are likely to undergo invasive coronary angiography in our centre, in accordance with the major international society guidelines.7 Urgent diagnostic angiography is readily accessible, and so stress-perfusion imaging is more commonly used in the outpatient setting in patients with stable, chronic coronary disease.8,9 There is increasing evidence that CMR prior to coronary angiography is useful in the inpatient setting as it may help to target intervention, assess viability and prevent repeated angiography.10,11 No stress CMR was performed on an inpatient basis in our cohort. However, at our centre there is routine use of invasive functional assessment with fractional flow reserve (FFR) to assess bystander coronary artery disease, which may then be treated simultaneously.12 However, there is potentially a role for inpatient stress perfusion CMR to assess bystander disease at the same time as assessing myocardial viability.
The most common diagnosis following CMR imaging was ischaemic cardiomyopathy and coronary heart disease in our patient cohort. This is comparable with the EuroCMR registry, which found that CMR was particularly important in suspected CAD and ischaemia. CMR had a high utility in this subgroup of patients with the assessment of viability of myocardium, aetiology of LVSD and in the planning of potential revascularisation and/or device strategies.
Similar to the EuroCMR registry, which evaluated the use of routine CMR, we found that there was a strong impact of CMR on patient management overall, leading to a change in 77% of patients (61.8% in the registry). The proportion of patients who had a change in, or new, diagnosis was also numerically higher in our study; 29% compared with 8.7%. This included four cases of LV thrombus, which had not been previously identified on transthoracic echocardiogram. This highlights the utility of inpatient CMR, even above outpatient CMR, with a greater potential diagnostic yield given the selected cohort of inpatients admitted under cardiology.
In our study, the median time to scan from electronic request was only two days in acute admissions, which may facilitate earlier diagnosis impacting patient management in a more significant way compared with the use of routine CMR. In other centres, or in the non-acute setting, CMR may occur later in the diagnostic pathway, once the diagnosis is provisionally confirmed, reducing the potential impact and utility as a diagnostic method. Early scanning is crucial in the diagnosis of certain conditions, such as myocarditis and Takotsubo syndrome, where the inflammation may resolve or reduce over time, and the appearances on scan are dynamic and time-critical.13 The time from scan to discharge was a key aspect in our evaluation; the median time from scan to discharge was four days, and inpatient CMR had a direct impact on patient discharge in a significant proportion of patients who were scanned (23/169 patients). This highlights the value of CMR as a diagnostic tool among inpatients, and its use may reduce overall length of stay in selected patients and certain presentations.
This study has several implications on clinical practice: CMR findings led to a change in medication regimen in a large number of patients and prompted further diagnostic investigations, such as CT chest scans, positron-emission tomography (PET), exercise tolerance or cardiac genetic testing. In some instances, CMR prevented further investigation, for example, in the cases where patients were scanned early it prevented the need for invasive coronary assessment in 8/169 cases. As such, there is a growing role in risk stratifying patients with suspected ischaemic heart disease or new LVSD to undergo CMR prior to diagnostic angiography. This minimises the procedural risk associated with cardiac catheterisation, may reduce the burden of tests required and, potentially, expedites discharge. One published study found there was a reduced rate of invasive coronary assessment in patients with non-ST-elevation myocardial infarction (NSTEMI) who underwent CMR first, compared with routine clinical care, with overall similar clinical outcomes.11 The specific EuroCMR registry protocol demonstrated that in 1,706 patients who had CMR for suspected CAD,14 the CMR was normal in 866/1,706 patients – which is a significant proportion of patients who could have avoided invasive angiography. Ongoing work is required to assess which patients may benefit the most from CMR performed early in the clinical course.
In terms of the safety and quality of CMR in our study, CMR was very well tolerated in our patient cohort and image quality was diagnostic in 93% cines. This is numerically lower in comparison to the EuroCMR registry (98%) but not unexpected. Inpatients are more likely to be clinically unstable and decompensated compared with outpatients, and so it can be challenging to obtain good quality, diagnostic images due to difficulties associated with breath holding and arrhythmias. It is reassuring that even in this group of patients we were able to make diagnoses in most studies.
This study, to the best of our knowledge, is the first to review the utility of inpatient CMR at a tertiary referral centre. A previous study evaluated routine use of CMR in a district general hospital (DGH) setting.14 Interestingly, the results were similar to our study and the most common indications for CMR were investigation of suspected CAD and in the diagnosis of cardiomyopathy. Of note, more viability studies were performed in our cohort (17%) compared with the patients referred for routine CMR at the DGH in this paper (9.1%), which may reflect accessibility to CMR in the acute instance in those with suspected CAD or ischaemia. There was more stress CMR performed in the outpatient cohort, as would be expected with the assessment of suspected stable CAD. Image quality was deemed diagnostic in 99.9% of cases in this published study, which was higher than we found in our inpatient cohort, but as would be expected with stable patients. Our results are also corroborated by the EuroCMR registry in which CMR was found to change patient management in 62% of cases (similar to 77% in our study).15 They found that importantly, CMR was normal in 11%. This is also reflected in our study where 12% of patient scans were normal studies.
Limitations identified within this study include the relatively short study period of six months and the relatively small sample size (169 patients). The retrospective observational nature of this study increases the risk of information bias. There was a degree of selection bias given only inpatient scans among patients who were admitted under cardiology or requested following discussion with the cardiology team were included. In addition, there was a lack of comparator group in this study, for example inpatients that did not have CMR and had echocardiogram ± angiography alone, a comparator group would have allowed us to further validate our findings. Prospective studies that randomise patients to inpatient and outpatient CMR and compare factors, such as certainty of diagnosis, length of hospital stay, impact on patient management and number of invasive procedures, would be of particular interest to corroborate our findings.
Conclusion
CMR is an essential tool in the early assessment of cardiology inpatients. In this single tertiary centre study, we have shown that inpatient CMR is safe, diagnostic and has a direct impact on patient management, corroborating the EuroCMR registry findings. More widespread use of CMR in the acute setting could prevent unnecessary invasive investigations and treatments, and improve patient care.
Key messages
- This is the first comprehensive review of the use of cardiovascular magnetic resonance (CMR) in the acute setting at a tertiary cardiology referral centre
- The main indications for inpatient CMR include investigation of new left ventricular systolic dysfunction, assessment of possible cardiomyopathy and in suspected acute coronary syndrome
- Inpatient CMR changes patient management and leads to medication changes, further investigation or, interestingly, results in the avoidance of further invasive procedures, such as coronary angiography
Conflicts of interest
None declared.
Funding
None.
Study approval
This was a clinical audit (AUDI002142) performed at St. George’s Hospital University Hospitals NHS Foundation Trust, London, UK, and, as such, external ethics were not required.
References
1. Salerno M, Sharif B, Arheden H et al. Recent advances in cardiovascular magnetic resonance: techniques and applications. Circ Cardiovasc Imaging 2017;10:e003951. https://doi.org/10.1161/CIRCIMAGING.116.003951
2. Assomull RG, Pennell DJ, Prasad SK. Cardiovascular magnetic resonance in the evaluation of heart failure. Heart 2007;93:985–92. https://doi.org/10.1136/hrt.2003.025304
3. Messroghli DR, Moon JC, Ferreira VM et al. Clinical recommendations for cardiovascular magnetic resonance mapping of T1, T2, T2 and extracellular volume: a consensus statement by the Society for Cardiovascular Magnetic Resonance (SCMR) endorsed by the European Association for Cardiovascular Imaging (EACVI). J Cardiovasc Magn Reson 2017;19:75. https://doi.org/10.1186/s12968-017-0389-8
4. Greenwood JP, Maredia N, Radjenovic A et al. Clinical evaluation of magnetic resonance imaging in coronary heart disease: the CE-MARC study. Trials 2009;10:62. https://doi.org/10.1186/1745-6215-10-62
5. Pennell DJ, Sechtem UP, Higgins CB et al. Clinical indications for cardiovascular magnetic resonance (CMR): Consensus Panel report. Eur Heart J 2004;25:1940–65. https://doi.org/10.1081/JCMR-200038581
6. Bruder O, Schneider S, Nothnagel D et al. EuroCMR (European Cardiovascular Magnetic Resonance) registry: results of the German pilot phase. J Am Coll Cardiol 2009;54:1457–66. https://doi.org/10.1186/1532-429X-11-S1-O13
7. Collet JP, Thiele H, Barbato E et al. 2020 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2021;42:1289–367. https://doi.org/10.1093/eurheartj/ehaa909
8. National Institute for Health and Care Excellence. Recent-onset chest pain of suspected cardiac origin: assessment and diagnosis. CG95. London: NICE, 2016. Available from: https://www.nice.org.uk/guidance/cg95
9. Gulati M, Levy PD, Mukherjee D et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol 2021;78:e187–e285. https://doi.org/10.1161/CIR.0000000000001029
10. Kim RJ, Wu E, Rafael A et al. The use of contrast-enhanced magnetic resonance imaging to identify reversible myocardial dysfunction. N Engl J Med 2000;343:1445–53. https://doi.org/10.1056/NEJM200011163432003
11. Smulders MW, Kietselaer BLJH, Wildberger JE et al. Initial imaging-guided strategy versus routine care in patients with non-ST-segment elevation myocardial infarction. J Am Coll Cardiol 2019;74:2466–77. https://doi.org/10.1016/j.jacc.2019.09.027
12. Patricio L, Tonino PAL, De Bruyne B et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009;360:213–24. https://doi.org/10.1056/NEJMoa0807611
13. Kato K, Daimon M, Sano M et al. Dynamic trend of myocardial edema in Takotsubo syndrome: a serial cardiac magnetic resonance study. J Clin Med 2022;11:987. https://doi.org/10.3390/jcm11040987
14. Abraham G, Shamsi A, Daryani Y. Comprehensive study of routine clinical use of cardiac MRI in a district general hospital setting. Br J Cardiol 2018;25:111–14. https://doi.org/10.5837/bjc.2018.020
15. Bruder O, Wagner A, Lombardi M et al. European cardiovascular magnetic resonance (EuroCMR) registry – multi-national results from 57 centers in 15 countries. J Cardiovasc Magn Reson 2013;15:1–9. https://doi.org/10.1186/1532-429X-15-9
