International guidelines recommend ‘heart teams’ as the preferred method for decision-making. Heart team processes, mandatory attendees and investigations vary significantly between hospitals. We assessed outcomes following mitral valvular surgery in a tertiary referral centre with a dedicated mitral multi-disciplinary team (MDT).
This was a single-centre retrospective review of prospectively collected data within the ‘mitral database’ of mitral valvular disease patients. The ‘mitral MDT’ meeting involved pre-operative imaging and clinical data review, including mandatory transoesophageal echocardiography; recommendation for planned procedure, as well as an appropriate surgeon; and review of echocardiography images and clinical outcomes after surgery had been performed.
Between 2016 and 2020, 395 patients with mitral valvular disease were discussed at MDT. Of these, 310 patients underwent surgery. During the same time interval, 75 patients had surgery without MDT discussion: 84% of patients not discussed were urgent or emergent procedures and, in these, the most common pathology was degenerative mitral regurgitation (DMR, 46%) followed by infective endocarditis (30%). Of those discussed at MDT the pathology was: DMR 65%; mitral stenosis 14%; functional mitral regurgitation (MR) 5%; rheumatic MR 4%; endocarditis 4%; ischaemic MR 4%; and other pathologies 4%. For patients with DMR having elective surgery, the repair rate was 93% with mortality 2% and median (IQR) length of stay 5 (4–6) days. Postoperative transthoracic echocardiography demonstrated 99% of elective DMR patients had ≤2+ MR and <1% severe (3+) MR.
In conclusion, a dedicated ‘mitral MDT’ can enhance the safe delivery of care with consistently high repair rates for DMR patients with excellent outcomes.
Introduction

Timely corrective surgery for severe mitral regurgitation (MR) reduces the risk of limiting symptoms and irreversible left ventricular dysfunction.1,2 Left untreated, severe MR carries a poor prognosis. In asymptomatic patients, the estimated five-year rates of death from any cause, death from cardiac causes and adverse cardiac events (death, heart failure or new atrial fibrillation), are 22%, 14% and 33%, respectively.2 The prognosis for symptomatic patients is significantly worse, and further adversely affected by older age and comorbidities, including atrial fibrillation, pulmonary hypertension, left atrial dilatation, and reduced left ventricular systolic function.3-5 For surgical management, mitral valve repair has been shown to demonstrate superior outcomes to mitral valve replacement.6,7 In 2015, around 2,400 mitral valve repairs were performed in Great Britain and Ireland,8 with an associated mortality ranging from 1.09% (isolated elective mitral valve repair) to under 6% (urgent mitral valve repair).8
In spite of the fact that the role of the multi-disciplinary team (MDT) meeting has been developed and widely adopted in the management of coronary artery disease,9 the ‘mitral MDT’, nationally, has lagged behind and varied in composition, frequency and type of cases discussed. Decision-making in ‘heart teams’ is accepted as being the preferred clinical method, and is now recommended in International guidelines, although little evidence exists to corroborate this.10
Bridgewater et al. focused on institutional, rather than individual, process issues to define standards for best practice in mitral valve repair by consensus of a multi-disciplinary professional group of cardiac surgeons, anaesthetists, and cardiologists. By providing challenging, yet achievable, standards, those centres undertaking mitral valve repair could both benchmark their care and be stimulated towards improvements in care.11
It is the intention of this study to investigate outcomes following mitral valvular surgery in a tertiary referral centre with a dedicated ‘mitral MDT’.
Materials and method
Following Society for Cardiothoracic Surgery of Great Britain and Ireland recommendations (SCTS), and in keeping with European guidelines,10 a ‘mitral MDT’ was set up and developed, since 2015, at the James Cook University Hospital, Middlesbrough. The team consists of dedicated clinicians with a subspecialist interest and expertise in caring for patients with MR, and comprises core members: cardiac surgeons; imaging cardiologist with expertise in echocardiography, magnetic resonance imaging (MRI), and cardiac computed tomography (CT); cardiologists with expertise in heart failure management; interventional cardiologist with expertise in percutaneous treatment of structural heart disease; cardiac anaesthetists; and specialised nurses. The core group of consultant cardiologists and cardiac surgeons were all accredited specialists in their field, working in a tertiary referral National Health Service (NHS) hospital, with years of experience in the management of valvular heart disease. They all have declared interest in the mitral valve, are regular attendees and participants at the MDT meeting and have continued professional development (CPD) in this area. An environment of mutual respect, trust, equality, constructive discussion and opportunity to challenge is encouraged. An imaging cardiologist reviews the images prior to the meeting and acts as chair of the meeting.
The ‘mitral MDT’ involves pre-operative imaging and clinical data review, including mandatory transoesophageal echocardiography; recommendation for the planned procedure, as well as choice of appropriate cardiac surgeon with expertise and results as good as national targets. Decisions regarding intervention are based on European Society of Cardiology (ESC)12 and American Heart Association (AHA)13 guidelines. The process is designed to determine whether the mitral valve is amenable to repair and for subsequent referral to an expert mitral valve repair surgeon. Following surgery, the MDT reviews transthoracic echocardiography images for grade of MR (trans-valvular vs. para-valvular) and clinical outcomes. A comprehensive database to capture data and facilitate the MDT process has been developed, which allows for further audit and research.
Since the inception of the mitral MDT at our centre in 2015, there has been a concerted effort to capture all mitral cases for discussion within a quorate forum of the mitral MDT. Cardiologists from local and peripheral centres are encouraged to refer to the MDT, and local cardiac surgeons with expertise in mitral valvular surgery form part of the quorate forum. Over time, with improved infrastructure and awareness of the mitral MDT, fewer patients have slipped through the MDT review net. It is the aim of the MDT to include all mitral valvular disease patients for formal review and discussion with a view to agreeing a consensus management plan. Although no specific exclusion criteria exist, capturing urgent/emergent cases prior to weekly MDT review sessions remains logistically difficult. Although these patients were not discussed to avoid delaying definitive treatment, with the system currently evolving to electronic MDT discussion to include urgent cases, only emergent patients will be missed in the future. As a dedicated weekly forum, the mitral MDT offers a platform for learning and training for specialist trainees, medical students and allied health professionals, so they can develop their understanding of the principles and practice in management of mitral valvular disease. Research and audit projects are encouraged and facilitated with access to the specialist mitral MDT database through approved channels.
Following hospital approval for this departmental clinical audit, we performed a retrospective review of the prospectively collected data within the ‘mitral database’ between 2016 and 2020. Anonymised patient outcome data are collected routinely for local and national databases. The study sought to address the following specific questions:
- Were all patients undergoing mitral valve surgery, since 2016, discussed at the ‘mitral MDT’?
- Did all patients with degenerative mitral valve disease undergo mitral valve reparative surgery?
- For degenerative mitral regurgitation (DMR) patients, was the observed mortality following elective mitral repair within expected risk?
- Were all elective DMR patients, who had undergone mitral valve repair, left with moderate (≤2+) MR or less at early (less than six weeks) echocardiography?
Ethics committee approval was not required, as anonymised patient outcome data are collected routinely for local and national databases. Data were analysed with statistical package SPSS 27.0. Categoric or ordinal data were compared using χ2 tests or Kendall tau-b, respectively. Continuous data are presented as mean ± standard deviation (SD) or median (lower, upper quartiles). Normally distributed data were compared using independent two-sided t-tests. Skewed data were either logarithmically transformed or analysed non-parametrically (Mann-Whitney U test).
Results
Table 1. All patients discussed at mitral multi-disciplinary team (MDT) meeting from January 2016 to May 2020
| Total patients discussed in MDT | N=395 |
|---|---|
| Surgery, n (%) | 310 (78) |
| Non-interventional outcome, n (%) | 49 (12) |
| Medical treatment, n (%) | 25 (6) |
| Surgical turn down, n (%) | 2 (0.6) |
| Mitraclip, n (%) | 8 (2) |
| Balloon valvuloplasty, n (%) | 1 (0.3) |
Between 2016 and 2020, 395 patients with mitral valvular disease were discussed at the MDT (figure 1). Of these, 310 patients underwent surgery (table 1). During the same time interval, 75 patients had surgery without MDT discussion (table 2): 84% of patients not discussed underwent urgent or emergent procedures and, in these, the most common pathology was DMR (46%) followed by infective endocarditis (30%). Those not discussed at the MDT had a higher median EuroSCORE 2 risk profile (6.8% vs. 2%).
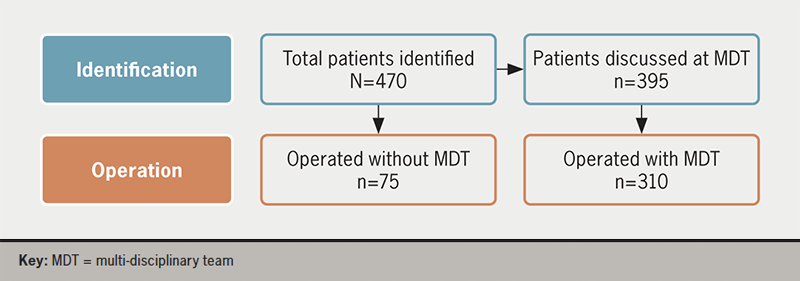
Table 2. Demographic data of patients (n=385) who underwent mitral valve surgery (2016–2020) that were discussed at mitral MDT meeting compared with those who underwent surgery but were not discussed at mitral MDT meeting
| MDT (n=310) | No MDT (n=75) | p | |
|---|---|---|---|
| Mean age ± SD, years | 66 ± 12 | 64 ± 13 | 0.344 |
| Female, n (%) Male, n (%) |
116 (38) 194 (62) |
29 (39) 46 (61) |
0.030 |
| Median BMI (IQR), kg/m2 | 26 (24–29) | 26 (22–29) | 0.457 |
| Urgent/emergent, n (%) | 55 (18) | 63 (84) | <0.001 |
| Median NYHA (IQR) | 3 (2–4) | 4 (3–4) | <0.001 |
| Diabetes mellitus (oral therapy/insulin), n (%) | 29 (9) | 1 (23) | 0.002 |
| Atrial fibrillation/flutter, n (%) | 114 (37) | 21 (28) | 0.114 |
| Extra-cardiac arteriopathy, n (%) | 14 (5) | 4 (5) | 0.768 |
| TIA/CVA, n (%) | 48 (16) | 8 (11) | 0.852 |
| Good LV function (LVEF ≥50%), n (%) | 216 (70) | 50 (67) | 0.748 |
| Moderate LV function (LVEF 30–49%), n (%) | 81 (26) | 19 (25) | 0.876 |
| Poor LV function (LVEF <30%), n (%) | 8 (3) | 6 (8) | 0.281 |
| Moderate pulmonary hypertension, n (%) | 31 (10) | 12 (16) | 0.142 |
| Severe pulmonary hypertension, n (%) | 39 (13) | 16 (21) | 0.053 |
| Chronic lung disease, n (%) | 52 (17) | 15 (20) | 15 (20) |
| Poor mobility, n (%) | 1 (0.3) | 7 (9) | 0.101 |
| Median CrCl (IQR), ml/min | 78 (60–100) | 63 (45–99) | 0.027 |
| Median EuroSCORE 2 (IQR), % | 2.0 (1.2–4.5) | 6.8 (1.2–14.3) | 0.621 |
| Key: BMI = body mass index; CrCl = creatinine clearance; CVA = cerebrovascular accident; IQR = interquartile range; LV = left ventricular; LVEF = left ventricular ejection fraction; MDT = multi-disciplinary team; NYHA = New York Heart Association; SD = standard deviation; TIA = transient ischaemic attack | |||
|
Table 3. Pathology of patients who attended operating room that were discussed at mitral MDT meeting
|
|||||||||||||||||||||
|
Table 4. Mitral valve surgery in degenerative mitral regurgitation: repair versus replacement. All operated patients MDT versus no MDT discussion
|
|||||||||||||||||||||
|
Table 5. Outcome following DMR repair-only surgery: in-hospital mortality elective versus urgent/emergent. All operated patients whether discussed or not at mitral MDT meeting
|
|||||||||||||||||||||
|
Table 6. Outcome following elective DMR repair-only surgery: assessment of postoperative mitral regurgitation by early (up to 6 weeks postoperative) transthoracic echocardiography. Operated patients whether discussed or not at mitral MDT meeting
|
|||||||||||||||||||||
Of those discussed at MDT, DMR was the most common pathology (65%) followed by: mitral stenosis (14%); functional MR (5%); rheumatic MR (4%); endocarditis (4%); ischaemic MR (4%); and other pathologies (4%) (table 3). Of all DMR patients undergoing surgery (elective; urgent/emergent), the mitral reparative repair rate was higher for patients discussed at MDT compared with those not discussed (92% vs. 80%) (table 4).
For patients with DMR having elective surgery only, the repair rate was 93%. Within this elective repair cohort, the mortality was 2% and median (IQR) length of stay 5 (4–6) days. For all DMR patients who underwent mitral reparative surgery, those performed on an urgent/emergent basis had higher in-hospital mortality compared with those that underwent elective surgery (6% vs. 1%) (table 5).
Postoperative transthoracic echocardiography demonstrated 99% of elective DMR patients had ≤2+ MR and <1% severe MR following reparative surgery (table 6).
Discussion
This single-centre retrospective study was designed to review the practice of mitral valvular reparative surgery in a centre with a well-established specialised ‘mitral MDT’ working collectively towards enhanced patient outcomes. The ‘mitral MDT’ was formed to meet the demands of rapidly changing medical practice, where there has been a paradigm shift towards shared decision-making. Recently, evidence for feasibility and timeliness to decision and treatment has emerged in the management of coronary artery disease.14 Furthermore, the implementation of a multi-disciplinary heart team for mitral valve disease has been shown, in a small study, to be a valuable approach for the selection of patients for different treatment modalities: 30-day mortality dropped from 4.4% to 1.7% for surgically treated patients when specified to a dedicated surgeon.15 In another single-centre cohort, shared decision-making within the mitral heart team assigned low-risk patients with favourable anatomy to surgical repair, while high-risk patients underwent Mitraclip or surgical replacement. This strategy was associated with improved outcomes for Mitraclip patients and those undergoing surgical or percutaneous repair of isolated primary mitral regurgitation.16
Our dedicated mitral MDT has been designed to capture and record, within its database, all patients flagged up to our tertiary centre with mitral valve disease. These patients undergo a comprehensive review by an expert quorate panel to decide on the best management plan, which may be surgical. With increased awareness throughout the trust, and development of pathways, our intention is to build a secure framework to channel all patients found with mitral valve disease, within our trust or referring hospitals, directly to our mitral MDT. This wider process ensures all patients are reassured they have received an expert and complete review of their newly found diagnosis of mitral valve disease. As the mitral MDT is a new phenomenon nationally, we believe our experience sets out the frameworks for other trusts to build their dedicated service.
Our data suggest that, with the addition of this well-functioning specialised mitral team, consistently high rates of repair for DMR can be achieved. All of the repair rates are above the ESC target for a heart valve centre. In patients with DMR, who did not have a MDT discussion, lower repair rates (80%) were seen. Statistical significance was not achieved, presumably due to the relatively small number of cases analysed retrospectively. The over-riding reason for lower repair rates in those not discussed at MDT group is unclear. Those not discussed at MDT (n=75) were more likely to present as urgent/emergent surgical cases with more comorbidities and higher risk. We speculate, but recognise it is difficult to elucidate, these patients may not have had the subtle benefits of the MDT, which include robust anatomical delineation of the degenerative pathology by transoesophageal echocardiography, consensus on the mechanism of regurgitation, and the highlighting of potential issues with a plan for repair.
The majority (78%) of those patients (n=395) referred to and discussed at the MDT underwent surgery. Of those remaining, the MDT recommendations were for: non-interventional outcome (12%); medical treatment (6%); Mitraclip (2%); surgical turn-down (<1%); and balloon valvulopasty (<1%). Prior to the intervention of MDT discussion, it was possible that consensus may not have been reached on patient management, as both indications for surgery (less than severe MR; secondary MR without a revascularisation indication) or suitability for surgery, were unclear (anatomy; comorbidities; asymptomatic with high-risk repair).
As we view the MDT process to be beneficial in our hospital and region, we aim to increase the number of cases reviewed by: developing our online eMDT capability (quorate; data and outcome recording) so as to have comparable infrastructure available to ‘capture’ urgent/emergent cases prior to surgery; weekly MDT meetings (currently fortnightly); and retrospective postoperative MDT review of cases that were not discussed pre-operatively.
For patients with DMR having elective surgery and discussed by the MDT, repair rates meet international standards (93%) with low mortality and length of stay. Quality outcomes, including postoperative transthoracic echocardiography, were excellent with 99% of elective DMR patients left with residual MR 2+ or less and only <1% with severe (3+ or greater) MR. Of those DMR cases not receiving repair, the suggestion was that this was due to more complex pathology (i.e. not single scallop posterior leaflet disease) decided pre-operatively at MDT or intra-operatively due to an unsatisfactory result of primary repair.
Although no trial data currently exist to determine the impact of the mitral MDT on outcomes, among our clinicians the consensus is that the structure and process has impacted positively. The MDT setting provides a more comprehensive and consistent assessment of mitral valve pathology by expert attendees and allows a consensus opinion to emerge.
The ESC has recommended the shift towards decision-making within ‘heart teams’, although limited data exist, currently, to support their benefit. With the introduction of the mitral MDT, individual centres can benchmark surgical results for degenerative disease against ESC criteria, which provides a platform for further quantitative assessment and improvement.
Although the mitral MDT is felt to enhance the delivery of safe and appropriate care, limitations are recognised. Occasionally, the absence of a referring cardiologist, particularly from peripheral institutions, means decision-making is entirely dependent on the quality of the information provided. As such, symptomatology, comorbidities, quality of imaging and details of treatments to date, may not be wholly correct or of the required standard, and, as such, may introduce inaccuracies or impact on making the correct decisions. With better technology, the referrers themselves should be able to be more involved in the MDT remotely, to overcome this challenge. This has been a particular benefit of the new ways of working online during the COVID pandemic, allowing much wider participation, without the need to travel to meetings. Finally, a significant hurdle to clinicians adopting the MDT process is the need to defer their decisions to achieve a consensus in a MDT setting.
Conclusion
In conclusion, a dedicated ‘mitral MDT’ can enhance the safe delivery of care with consistently high repair rates for DMR patients with excellent outcomes. The benefit of the mitral MDT lies in the balanced discussions between multiple specialists, leading to informed, evidence-based bespoke decisions for each individual patient. The standardised approach to reviewing each patient and capturing data in a purpose-built database improves clinical governance and provides a platform for a strong research base. The heart team is thought to be able to:17
- More objectively interpret the available diagnostic information
- Implement guideline-directed therapy
- Consider and involve local expertise
- Through shared decision-making, take into account patient preferences and provide a more uniform decision-making process.
The authors encourage further studies to elucidate the reasons why repair for DMR patients did not take place to seek to improve repair rates safely going forward. With the wider adoption nationally of the dedicated mitral MDT, focusing future research towards a multi-centre randomised-controlled trial comparing outcomes of patients discussed versus not discussed at MDT would help establish objectively the degree of benefit provided by this process.
Key messages
- A dedicated ‘mitral multi-disciplinary team (MDT)’ can enhance the safe delivery of care with consistently high repair rates for degenerative mitral regurgitation (DMR) patients with excellent outcomes
- The benefit of the mitral MDT lies in the balanced discussions between multiple specialists leading to informed, evidence-based bespoke decisions for each individual patient
- The standardised approach to reviewing each patient and capturing data in a purpose-built database improves clinical governance and provides a platform for a strong research base
- The heart team is thought to be able to more objectively interpret the available diagnostic information; implement guideline-directed therapy; consider and involve local expertise; and, through shared decision-making, take into account patient preferences and provide a more uniform decision-making process
Conflicts of interest
None declared.
Funding
None.
Study approval
The authors confirm that the investigative methods used do conform to the standards of good research practice. Data utilised were anonymous and extracted from the prospectively collected, purpose-built clinical database for the mitral MDT. Patient anonymity was maintained throughout and only hospital registration numbers were utilised.
References
1. Ling LH, Enriquez-Sarano M, Seward JB et al. Clinical outcome of mitral regurgitation due to flail leaflet. N Engl J Med 1996;335:1417–23. https://doi.org/10.1056/NEJM199611073351902
2. Enriquez-Sarano M, Avierinos JF, Massika-Zeitoun D et al. Quantitative determinants of the outcome of asymptomatic mitral regurgitation. N Engl J Med 2005;352:875–83. https://doi.org/10.1056/NEJMoa041451
3. Guazzi M, Galie N. Pulmonary hypertension in left heart disease. Eur Respir Rev 2012;21:338–46. https://doi.org/10.1183/09059180.00004612
4. Maganti K, Rigolin V, Enriquez-Sarano M, Bonow R. Valvular heart disease: diagnosis and management. Mayo Clin Proc 2010;85:483–500. https://doi.org/10.4065/mcp.2009.0706
5. Pfeffer M, Shah A, Bourlaug B. Heart failure with preserved ejection fraction in perspective. Circ Res 2019;124:1598–617. https://doi.org/10.1161/CIRCRESAHA.119.313572
6. Enriquez-Sarano M, Schaff HV, Orszulak TA et al. Valve repairs improves the outcome of surgery for mitral regurgitation: a multivariate analysis. Circulation 1995;91:1022–8. https://doi.org/10.1161/01.CIR.91.4.1022
7. Lee EM, Shapiro LM, Wells FC. Superiority of mitral valve repair in surgery for degenerative mitral regurgitation. Eur Heart J 1997;18:655–63. https://doi.org/10.1093/oxfordjournals.eurheartj.a015312
8. Grant SW, Jenkins DP. National cardiac surgery activity and outcomes report 2002–2016. London: Society for Cardiothoracic Surgery, 2020. Available from: https://scts.org/professionals/reports/resources/default.aspx
9. Luckraz H, Norell M, Buch M, James R, Cooper G. Structure and functioning of a multidisciplinary ‘Heart Team’ for patients with coronary artery disease: rationale and recommendations from a joint BCS/BCIS/SCTS working group. Eur J Cardiothorac Surg 2015;48:524–9. https://doi.org/10.1093/ejcts/ezv083
10. Chambers JB, Prendergast B, Iung B et al. Standards defining a ‘Heart Valve Centre’: ESC Working Group on Valvular Heart Disease and European Association for Cardiothoracic Surgery Viewpoint. Eur J Cardiothorac Surg 2017;52:418–24. https://doi.org/10.1093/ejcts/ezx283
11. Bridgewater B, Hooper T, Munsch C et al. Mitral repair best practice: proposed standards. Heart 2006;92:939–44. https://doi.org/10.1136/hrt.2005.076109
12. Falk V, Baumgartner H, Bax J et al. 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur J Cardiothorac Surg 2017;52:616–64. https://doi.org/10.1093/ejcts/ezx324
13. Nishimura R, Otto C, Bonow R et al. 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2017;135:e1159–e1195. https://doi.org/10.1161/CIR.0000000000000503
14. Domingues CT, Milojevic M, Thuijs D et al. Heart team decision making and long term outcomes for 1000 consecutive cases of coronary artery disease. Interact Cardiovasc Thorac Surg 2019;28:206–13. https://doi.org/10.1093/icvts/ivy237
15. Heuts S, Olsthoorn JR, Hermans SMM et al. Multidisciplinary decision-making in mitral valve disease: the mitral heart team. Neth Heart J 2019;27:176–84. https://doi.org/10.1007/s12471-019-1238-1
16. Kulling M, Corti R, Noll G et al. Heart team approach in treatment of mitral regurgitation: patient selection and outcome. Open Heart 2020;7:e001280. https://doi.org/10.1136/openhrt-2020-001280
17. Head SJ, Kaul S, Mack MJ et al. The rationale for Heart Team decision-making for patients with stable, complex coronary artery disease. Eur Heart J 2013;34:2510–18. https://doi.org/10.1093/eurheartj/eht059
