The British Society of Echocardiography (BSE) Education Committee has published a minimum dataset of 24 views for acquiring a standard adult transthoracic echocardiogram. To establish adherence to the minimum dataset, and secondly to establish the indication for echocardiography, we performed a retrospective review of 961 patients’ echocardiogram images and a prospective review (re-audit) of 832 patients’ echocardiograms, following a programme of echocardiographer education. Images were obtained from a computerised database over three months. Subjects were adult patients referred to the cardiology department of a large tertiary hospital in Oxfordshire. Results showed 17 views were consistently obtained in over 78% of patients, irrespective of audit period. Seven views were obtained in less than 50% of patients; of these, five views were performed significantly more frequently during re-audit. Apical four chamber continuous wave Doppler across the tricuspid valve, and subcostal views were performed in less than 45% of patients; this did not increase during re-audit. The main indication for performing an echocardiogram was assessment of left ventricular function, followed by assessment of valve function and investigation of arrhythmia. In conclusion, all echocardiographers need to be made aware of, and adhere closely to the requirements of the minimum dataset.
Introduction
Echocardiography plays a major role in the investigation of heart disease.1 The British Society of Echocardiography (BSE) Education Committee published a minimum dataset for performing a standard adult transthoracic echocardiogram in 2005. The intended benefits of these recommendations are to “support cardiologists and echocardiographers to develop local protocols and quality control programs for adult transthoracic study; promote quality by defining a ‘minimum dataset’ of descriptive terms and measurements and systematic approach to constructing a report; facilitate the accurate comparison of serial echocardiograms performed in patients at the same or different sites; and to facilitate the transition to digital echocardiography acquisition and reporting systems that utilise database (software) architecture”.2 The BSE notes that this would only be sufficient when the echocardiographic study is completely normal, however, some concern exists that even this minimum set of data is not being collected by all echocardiographers, on all patients. We therefore decided to audit the performance of echocardiographers within our institution with the intention of establishing how closely they adhered to the guidelines as set out in the minimum dataset.
Methods

We performed an audit of 1,793 consecutive transthoracic echocardiogram studies generated from a computerised database within the department of cardiology at the John Radcliffe Hospital, a tertiary referral hospital in Oxford, from 1 June to 25 August 2005. Approval from an ethics committee was not sought as the analysis was undertaken on an anonymised database; it was not possible to personally identify any research participants. Data collected included the indication for performing the study, as documented on the request form. We then analysed each sequence of images to determine which of the 24 views recommended by the BSE had been obtained (table 1). Two views which are included in the dataset but not supported unanimously are in italics in the table (pulsed Doppler in the left ventricular outflow tract and pulsed or continuous wave Doppler in the pulmonary artery). Data were collected retrospectively for the period 1 June to 18 July; the seven echocardiographers were then informed of the audit, and completed a programme of education to familiarise them with the requirements of the minimum dataset. Following this intervention prospective data collection occurred between 19 July and 25 August.
Data were analysed using a Chi-squared test. A p value of less than 0.05 was regarded as significant.
Results
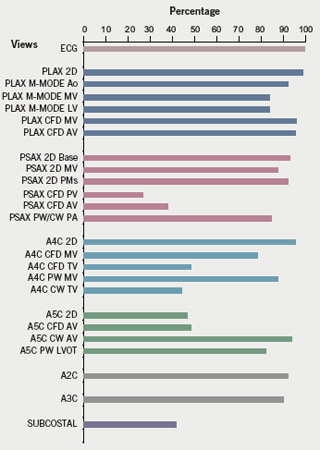

The study comprised 1,793 patients. The results are illustrated in figures 1 (retrospective data; prior to intervention) and 2 (prospective data; subsequent to intervention). Seventeen views were consistently performed in over 78% of patients, irrespective of audit period. Seven views were performed in less than 50% of patients; five of these were performed significantly more frequently after intervention (p<0.001) (figure 3). Two views, which were both performed in less than 45% of patients in the retrospective audit, did not increase significantly after intervention; these were apical four chamber continuous wave Doppler across the tricuspid valve, and subcostal. The subcostal view was actually obtained in significantly fewer patients, following intervention (p<0.05).


The main indication for performing an echocardiogram during this audit period was to assess left ventricular function (figure 4). Patients under investigation for a murmur, or for investigation of a previously documented native valve lesion (both placed in the category ‘valve disease’) comprised the second largest group. Investigation of arrhythmia was the third largest group; all other categories comprised less than 10% of studies performed.
Discussion
Echocardiography is a widely used tool in the investigation of heart disease. Between 42,800 and 47,700 studies per million population are carried out on an annual basis in the UK.3 The BSE minimum dataset functions as guidelines for those who perform echocardiography. This audit showed incomplete studies were being performed within our own hospital; following intervention, re-auditing revealed a significant increase in acquisition of five views. Certain views were performed in consistently low numbers of patients. The BSE guidelines state that when the condition or acoustic windows of the patient prevent the acquisition of one or more components of the dataset, this should be stated, however, this does not occur frequently in our practice. Concern exists regarding focussed studies, where echocardiographers perform a limited number of views to answer a specific question. Significant amounts of information can be missed this way, and adherence to a minimum dataset can avoid this.
Interestingly, the two views which are included in the dataset but not agreed unanimously (see above) were both performed in over 80% of our patients. The least acquired views were predominantly colour Doppler mapping for valves. The dataset specifies that at least two views with colour Doppler flow should be obtained for each valve; acquisition of most of these views did increase after educating echocardiographers about the guidelines. It may be that echocardiographers are only inclined to document abnormal findings, a sentiment that dates from a time when archive space was limited. In the normal subject, the information gained from pulse wave Doppler and colour flow Doppler is the same.
The subcostal window and continuous wave Doppler across the tricuspid valve in the apical window were both sampled infrequently and this did not improve with re-auditing. The subcostal window is important for visualising pericardial effusions and interatrial septal defects, and for looking for the presence of inferior vena cava collapse when calculating right heart pressures. Echocardiographers may not acquire subcostal views due to difficulty in obtaining quality images, for example in obese or pregnant subjects, or those that have recently undergone abdominal surgery. The BSE guidelines state that continuous wave is only necessary over the tricuspid valve if tricuspid regurgitation is visible on colour mapping. The relatively low use of this view found in this audit may therefore be appropriate.
Indications for echocardiography appear to have changed, when compared with previous studies. A large audit of over 11,000 echocardiogram referrals from primary care, performed between 1984 and 1990, showed assessment of valve disease to be the main reason for requesting a study (39%); left ventricular function assessment was requested half as frequently as in our audit (18%).4Congenital heart disease was the third most frequently cited indication (15% of studies); only 0.8% of studies in our audit were requested for congenital heart disease assessment (septal defect). These disparities may reflect differences in subgroup nomenclature, changing disease patterns and survival after cardiac events, implementation of national guidelines for physicians, and the previous audit being conducted at a specialist centre for congenital heart disease. In general, the requests for studies were appropriate.5
In conclusion, we have demonstrated that patients have been receiving incomplete echocardiographic studies, and we have highlighted the seven views that are less frequently acquired. We have shown that the indications for performing echocardiography have changed over time. It is suggested that all echocardiographers are made aware of the importance of adherence to the minimum dataset. Ensuring awareness of the required views will facilitate comprehensive echocardiographic studies.
Acknowledgements
The authors gratefully acknowledge the contribution made by Joe de Bono, Tony Protheroe and Cassandra Hammond to this manuscript.
Conflict of interest
No funding was sought for this audit, and no competing interests are declared.
Key messages
- The British Society of Echocardiography recently published a minimum dataset of the echocardiographic views needed to perform a complete adult transthoracic echocardiogram
- This audit showed the majority of views were obtained in the majority of patients. Five views were performed significantly more frequently during re-audit. Two views were performed in less than 45% of patients, and this did not increase during re-audit
- The main indication for performing an echocardiogram was assessment of left ventricular function followed by assessment of valve function and investigation of arrhythmia
- All echocardiographers need to familiarise themselves with the minimum dataset to ensure acquisition of high quality, comprehensive echocardiographic studies
References
- Department of Health. National Service Framework for Coronary Heart Disease. London: Department of Health, 2000.
- Echocardiography in South Thames. British Society of Echocardiography: Recommendations of a working party. February 2000.
- Hackett D. Cardiac workforce requirements in the UK. British Cardiac Society workforce committee, June 2005.
- Williams SG, Currie P, Silas JH. Open access echocardiography: a prospective audit of referral patterns from primary care. Int J Clin Pract 2003;57:136–9.
- Cheitlin MD, Alpert JS, Armstrong WF et al. ACC/AHA guidelines for the clinical application of echocardiography: executive summary. J Am Coll Cardiol 1997;29:862–79.
