A 34-year-old Filipino computer engineer with no previous medical history presented to the emergency department with sudden onset exertional breathlessness and intermittent palpations for 10 days. He had no associated dizziness, syncope or chest pain, and no significant family history or recent travel. Blood pressure was 126/69 mmHg and pulse 104 bpm, regular with normal volume and character. The jugular venous pressure was normal. A 4/6 continuous murmur with diastolic accentuation was heard loudest at the left lower sternal edge, associated with a diastolic thrill. Electrocardiogram (ECG) showed sinus tachycardia and no other abnormality.
Echocardiography showed a right coronary (anterior) aortic sinus aneurysm protruding into the right ventricle with a large (1.5 cm) fistula (figure 1). Biventricular size and function was normal; there were no other structural cardiac defects or evidence of infective endocarditis seen. Percutaneous device closure was not possible due to the large size of the aneurysm. He underwent cardiac surgery. There was a right coronary (anterior) aortic sinus aneurysm, which had ruptured into the right ventricle. Patch closure with bovine pericardium and aortic valve replacement with a 25 mm St. Jude Regent™ mechanical valve were
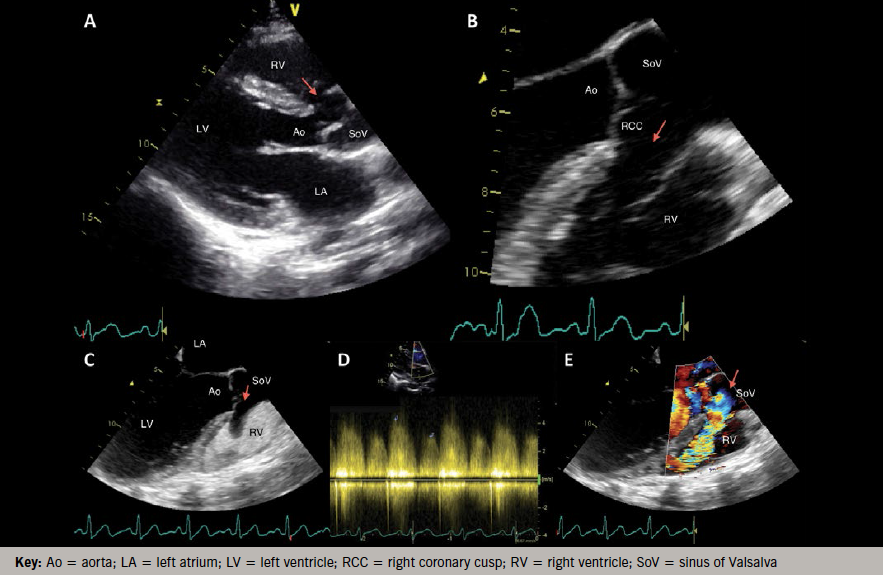
Ruptured aortic sinus (sinus of Valsalva) aneurysms are rare, but are an important differential diagnosis of a continuous murmur that can be diagnosed with echocardiography. Aortic sinus aneurysms can be congenital or acquired (e.g. due to infective endocarditis or Kawasaki’s disease), occur more often in males and have been reported in 0.15–3.5% of patients undergoing cardiac surgery. Right aortic coronary sinus aneurysms are most common, and have typically ruptured into the right ventricle; early surgical intervention can be life-saving
Conflict of interest
None declared.
