Many heart failure patients are eligible to receive financial support (Disability Living Allowance or Attendance Allowance) because of their impaired mobility. Those with a very limited prognosis can gain rapid access to these benefits by claiming under “special rules” with the support of a report (DS 1500) from their doctor.
Easily accessible routine clinical data are summarised that identify patients whose claims are most likely to succeed.
Introduction
The financial difficulties of the NHS, including those of cardiac services, are often highlighted in the medical press. However, patients’ financial problems are rarely addressed and the specific issue of helping heart failure patients to obtain their financial entitlements has never been discussed in the Journals.
It is now widely accepted that patients with heart failure have similar needs for supportive and palliative care as do patients with cancer: to control physical and psychological distress and for social and financial support.1,2
Many of these needs will be addressed when palliative care strategies3-5 are more widely implemented, as recommended by the Modernisation Agency.6 This has rightly focussed attention on patients’ medical needs, but in so doing the provision of practical financial support can be overlooked.7 This has widespread implications: patients with progressive diseases, irrespective of aetiology, have mutual concerns about their ability to cope financially as a result of their altered physical, social or employment situation, and about the burden that this puts on their families.8
Financial provisions for patients who are ill or disabled
In the UK, the Disability and Carers Service, part of the Department for Work and Pensions (DWP), provides non-means-tested, tax-free financial support (currently £62.25 per week) for patients ‘who need help with their personal care or have mobility difficulties because of an illness or disability’.9 Disability Living Allowance (DLA) is available for patients who claim before the age of 65 years and Attendance Allowance (AA) for those claiming aged 65 years or over. However, the processing of claims is often prolonged: claims will not normally succeed until the need for support has been present for three months for DLA or six months for AA – the ‘qualifying period’ – and there is often a further delay of many more months before the claim is processed and the benefit is paid.
In 1990 the DWP, recognising that some patients have a very limited life expectancy (described as being ‘terminally ill’), introduced ‘special rules’ to ensure that in such cases claims are dealt with very quickly. The normal qualifying period and other routine entitlement conditions are waived and the process is activated when a patient submits a claim specifically under the ‘special rules’ supported by their general practitioner (GP) or consultant completing a DS 1500 report, preferably submitted at the same time. For the purpose of the ‘special rules’ the legislation defines a patient as terminally ill if ‘he suffers from a progressive disease…. and his death can reasonably be expected within six months’.
Currently, ‘special rules’ cases are processed within the Department’s target clearance time of eight days.10 Despite this, most eligible heart failure patients do not submit claims.
Why don’t patients claim their financial entitlement?
The majority of heart failure patients eventually develop ‘mobility difficulties’ and will then qualify for DLA or AA. However, only approximately 50% of all eligible patients, most of whom have cancer, claim these benefits under either the normal or the special rules:11 there is also evidence that the neediest patients are the least likely to claim.12 There have been few studies into why so many patients do not claim, none of which specifically relate to heart failure patients. However, study of unselected patient groups has identified reasons that are as likely to apply to those with heart failure as to others. They include fear of stigmatisation because they are seeking financial help, ignorance of their entitlements, difficulties with form-filling, ignorance of available benefits and a lack of appropriate advice or encouragement from healthcare professionals, some of whom are also unaware of the available benefits.13
Claiming under the
special rules
There are two groups of heart failure patients who might claim under the special rules:
- Those whose eligibility for DLA or AA was overlooked until late in the natural history of their disease.
- Patients whose prognosis is poor from the time of diagnosis.
All claimants under the special rules have, by definition, a limited life expectancy. It is therefore important that their claims are submitted as soon as their eligibility is recognised. Patients’ failure to claim under the special rules is not only for the reasons given above. There are two other barriers both related to the patients’ poor prognosis. First, some doctors may be reluctant to inform patients of their poor prognosis, or patients may not wish to be informed about it,10 although there are rules and procedures in place to allow claims by a third party. The second barrier relates to the difficulty of prognostication, a common problem irrespective of disease aetiology14 and one which has been repeatedly confirmed in the case of heart failure.15 This difficulty is related to the variable natural history of heart failure, the high prevalence of sudden death and recurrent episodes of deterioration, which respond unpredictably to treatment.16 Under these circumstances doctors are understandably reluctant to assert that ‘death can reasonably be expected within six months’.
However, senior officials at the DWP have explained that prognostic accuracy is not required:10 ‘when the special rules were devised it was recognised that it is impossible to determine accurately when a person will die’. It is because of this that the phrase ‘death can reasonably be expected within six months’ implies the need for ‘an element of clinical judgement’ rather than requiring certainty. In fact the patients’ doctors are ‘deliberately not asked to give a prognosis’.
After receipt of the patient’s claim form and DS 1500 report, a decision maker at the Disability and Carers Service (an Executive Agency of the DWP) ‘takes medical advice on each special rules case from doctors who provide medical services to the agency in addition to the evidence from the patient’s own GP or consultant’. They decide, on the merits of individual claims in the light of all the evidence before them, what is a reasonable expectation.10
Nevertheless, despite these reassurances, many doctors are likely to remain unwilling to support a claim unless they can be reasonably confident that it has a good chance of being accepted.
Four criteria therefore need to be fulfilled to ensure that support is provided for eligible patients’ claims:
- better understanding of the special rules
- easily accessible evidence showing that for many patients ‘death can reasonably be expected within six months’
- wide dissemination of this evidence
- a strategy to ensure that qualifying patients are not overlooked.
Identifying patients most likely to qualify under the special rules
The vast majority of qualifying patients will have advanced heart failure, defined as having severe limitations (New York Heart Association [NYHA] III/IV) despite optimum conventional medication.17 This clinical scenario is seen in patients with both reduced and (relatively) preserved left ventricular systolic dysfunction. Most patients in the former group have a low ejection fraction of approximately 25–30%. Patients with these characteristics have an annual mortality of 30–50%.17
The figure (50%) is largely based on the outcome in patients recruited for clinical trials and epidemiological studies, who differ significantly from ‘average’ heart failure patients by virtue of treatment, age, and co-morbidities.
- The majority of patients, for clinical, organisational or financial reasons, still do not receive optimal treatment18 and so are deprived of its prognostic benefits.
- Most have a worse prognosis than the quoted annual mortality of 50% because they are at least 10 years older than the patients on whom that figure is based.19 This has a major impact on mortality. The annual mortality increases by between 10% and 40% for each decade increase in age.20–22 As a result, the annual mortality in a cohort of unselected patients with advance heart failure may be 60–70% rather than 50%.21
- Non-cardiac co-morbidities are very common and may dramatically reduce life expectancy. Seventy-five per cent of patients aged 65 years or older, who constitute 80% of the heart failure population, have three or more co-morbidities and approximately 50% have four or more.23
These factors are usually documented and easily accessed from patients’ clinical records. Each has an important independent impact on prognosis. Consequently, the more of these factors a patient has the more likely it is that they will fulfil the criteria of the special rules.
The prognostic impact of common co-morbidities
Renal failure, diabetes, depression, cognitive impairment, chronic obstructive pulmonary disease (COPD) and atrial fibrillation, are common and each independently reduces life expectancy. However, with respect to the published studies of each co-morbidity, patient characteristics, diagnostic criteria, methodology and statistical analyses vary and as a result they cannot be directly compared nor can the data be pooled (table 1).
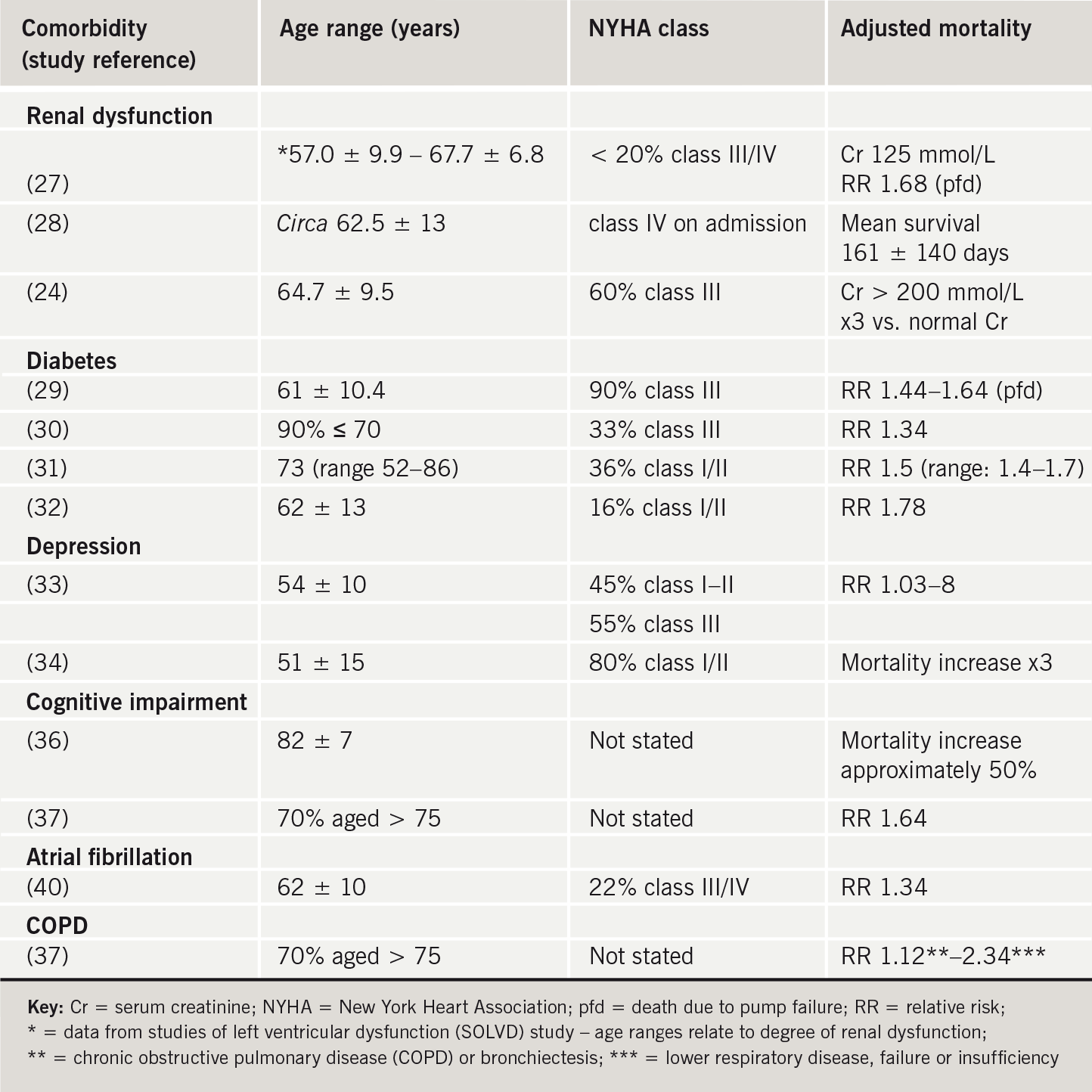
Renal dysfunction/failure
Renal dysfunction has a greater impact on prognosis than other co-morbidities.24 With each 1 ml/min decline in glomerular filtration rate (GFR) the mortality increases by 1%,25 but the serum creatinine level often does not begin to rise until the GFR has fallen to approximately 50 ml/minute.26 Consequently, a very modest increase in serum creatinine, to approximately 125 mmol/L, is associated with a rise in mortality of 50% (relative risk [RR] 1.4–1.6) which is independent of age, symptoms and diabetes.27
In addition, independent of other risk factors, as renal function deteriorates further, mortality continues to rise.24 Consequently, patients whose serum creatinine is greater than 150–200 mmol/L have a mortality two to three times that of patients with a normal value.24,28
The implication is that any increase in serum creatinine, especially in those of ‘average’ age and above who are not responding to conventional treatments, has serious implications for life expectancy.
Diabetes
Several studies have found that, as with renal impairment, the impact of diabetes on the prognosis is largely independent of age, ejection fraction and/or NYHA class. As a result, patients with diabetes, including, in one report, those 10 years younger than the average patient, and with only moderate left ventricular impairment have a 30–75% higher mortality than patients without diabetes.29-33
Depression
Depression, at least in the medium-to-long term, adversely affects the prognosis in heart failure. In two studies, the mortality of patients 20 years younger than most heart failure patients increased with time from diagnosis to between three and eight times that of the non-depressed.33,34
Cognitive impairment and dementia
Mild cognitive impairment and progression to dementia are very common in patients with heart failure:35 both are associated with an increase in mortality of up to almost five-fold (RR 1.64–4.9).36,37
COPD and other chronic lung diseases
Heart failure is a common underlying cause of death in patients with COPD38 and patients with heart failure are often hospitalised because of its complications. The mortality of patients with a range of chronic pulmonary pathologies including COPD and bronchiectasis is increased by between 10% and 30% compared with patients without lung disease.23
Atrial fibrillation
Patients with atrial fibrillation have an increased mortality of approximately 30–50% compared with those in sinus rhythm independent of underlying cardiac pathology.39 A recent report concluded that, in patients from the studies of left ventricular dysfunction (SOLVD) trial with symptomatic or asymptomatic left ventricular dysfunction who had atrial fibrillation, the mortality was 34% higher than in those in sinus rhythm.40
Anaemia
Anaemia is common in heart failure and, with very few exceptions, studies report an association with increased mortality.41 However, it is not clear if it is an independent predictor of prognosis since it is common in several of the co-morbidities noted above, even when they are not associated with heart failure,42 i.e. anaemia is certainly a marker of increased mortality but not necessarily an independent predictor.
Strategy for identifying eligible patients
Many patients have a worse prognosis than the commonly quoted 50% annual mortality for patients with advanced heart failure. The data reviewed here can be used to identify most of the patient groups who would qualify for financial support under the special rules. A large majority of these eligible patients will have a combination of intractable symptoms, age over 65 years and a combination of the co-morbidities discussed although, clearly, some will qualify for other quite different reasons.
A recent admission to hospital can also be used as a trigger for assessing patients’ eligibility to claim as this event identifies, in general terms, patients with an above-average mortality.43 The reported post-discharge mortality varies widely, depending on inclusion criteria and patient characteristics, for example an annual mortality of 36% in relatively young patients44 but a mean survival of only 4 ± 4 months in the very old.45
Patients and their carers benefit physically, socially and psychologically from timely financial support.46 The identification of those who are entitled to this should therefore become an integral part of the routine clinical assessment of patients with heart failure. This is especially important for those eligible under the special rules scheme.
Healthcare professionals involved in the management of patients with heart failure should understand the claims process, know which patients might be eligible, and be able to discuss the available benefits with patients and to assist with form-filling.
Acknowledgements
I wish to thank senior advisers at the Department for Work and Pensions who explained and clarified the ‘special rules’ during my correspondence with them, and Jennifer Wallace, independent research statistician, for advice and explanation of statistical data quoted in this paper.
Conflict of interest
None declared.
Key messages
- Many heart failure patients are eligible for financial support, and claims submitted by those with the worst prognosis are currently processed within eight days
- Most patients do not receive their financial entitlement because of misunderstanding of the claims process by doctors, other staff and patients
- Potentially successful applicants can often be identified from readily accessible clinical profiles
References
- World Health Organization. WHO definition of palliative care. Available from: http://www.who.int/cancer/
- Thomas K. Care for the dying at home. Oxford: Radcliffe Publishing, 2005; (Chap 13):203–15.
- Department of Health. Gold Standard Framework: a programme for community palliative care. www.goldstandardsframework.nhs.uk
- Department of Health. Gold Standard Framework: NHS end of life care programme. www.goldstandardsframework.nhs.uk/developments.php
- NHS Modernisation Agency. National Cancer Plan 2005:
Liverpool care of the dying pathway.
www.lcp-mariecurie.org.uk - NHS Modernisation Agency. Coronary Heart Disease Collaborative 2004. Supportive and palliative care for advanced heart failure. Available from: www.modern.nhs.uk/chd
- McIntyre R. Support for family and carers. In: Lugton J, Kindlen M (eds.). Palliative care: the nursing role. Edinburgh: Churchill Livingstone, 1999;193–215.
- Kutner JS, Steiner JF, Corbett KK, Jahnigen DW, Barton PL. Information needs in terminal illness. Soc Sci Med 1999;48:1341–52.
- www.direct.gov.uk
- Personal communications: Senior Officials, Department of Works and Pensions.
- Hoskins R, Carter D. Welfare benefits screening and referral: A new direction for community nurses? Health Soc Care Community 2000;8:390–7.
- Frost R. Missing out for years. Report on two years of the Disability Living Allowance and Attendance Allowance campaign. Bristol City Council Money Advice Service.
- Chapple A, Ziebland S, McPherson A, Summerton N. Lung patients perceptions of access to financial benefits: a qualitative study. Br J Gen Pract 2004;54:589–94.
- Christakis NA, Lamont EB. Extent and determinants of errors in doctors’ prognoses in terminally ill patients: prospective cohort study. BMJ 2003;320:469–73.
- Cowburn PJ, Cleland JGF, Coates AJS et al. Risk stratification in chronic heart failure. Eur Heart J 1998;19:696–710.
- Hanratty B, Hibbert D, Mair F et al. Doctors’ perceptions of palliative care for heart failure: focus group study. BMJ 2002;325:581–5.
- Stevenson LW. Design of therapy for advanced heart failure. Eur J Heart Fail 2005;7:323–31.
- Murphy NF, Simpson CR, McAlister FA et al. National survey of the prevalence, incidence, primary care burden and treatment of heart failure in Scotland. Heart 2004;90:1129–36.
- Petrie MC, Berry C, Stewart S et al. The failing ageing heart. Eur Heart J 2001;22:1978–90.
- Martinez-Sellez M, Robles JAG, Prieto L et al. Heart failure in the elderly: age related differences in clinical profile and mortality. Int J Cardiol 2005;102:55–60.
- Ho KKL, Anderson DM, Kannel WB et al. Survival after the onset of congestive heart failure in Framingham heart study subjects. Circulation 1993;88:107–15.
- MacIntyre K, Capewell S, Stewart S et al. Evidence of improving prognosis in heart failure: trends in case fatality in 66,547 patients hospitalised between 1986 and 1995. Circulation 2000;102:1126–31.
- Braunstein JB, Anderson GF, Gerstenblith G et al. Noncardiac comorbidity increases preventable hospitalization and mortality among medicare beneficiaries with chronic heart failure. J Am Coll Cardiol 2003;42:1226–33.
- Hillege HL, Girbes ARJ, deKam PJ et al. Renal function, neurohormonal activation and survival in patients with chronic heart failure. Circulation 2000;102:203–10.
- McAlister FA, Ezekowitz J, Tonelli M et al. Renal insufficiency and heart failure. Prognostic and therapeutic implications from a prospective cohort study. Circulation 2004;109:1004–9.
- Bannister KM, Field MJ. Clinical physiology of the kidney. In: Ledingham JGG, Warrel DA (eds). Concise Oxford textbook of medicine. Oxford: Oxford University Press, 2000;1105–11.
- Dries DL, Exner DV, Domanski MJ et al. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol 2000;35:681–9.
- Aaronson D, Mittleman MA, Burger AJ. Elevated blood urea nitrogen level as a predictor of mortality in patients admitted for decompensated heart failure. Am J Med 2004;116:466–73.
- Domanski M, Kraus-Steinrauf H, Deedwania P et al. The effect of diabetes on outcome of patients with advanced heart failure in the BEST Trial. J Am Coll Cardiol 2003;42:
914–22. - Shindler DM, Kostis JB, Yusuf S et al. Diabetes mellitus, a predictor of morbidity and mortality in the studies of left ventricular dysfunction (SOLVD) trials and registry. Am J Cardiol 1996;77:1017–20.
- Gustafsson I, Brendorp B, Seibaek M et al. Influence of diabetes and diabetes-gender interaction on the risk of death in patients hospitalized with congestive heart failure. J Am Coll Cardiol 2004;43:771–7.
- Burger AJ, Tsao L, Aronson D. Prognostic impact of diabetes in patients with acute decompensated heart failure. Am J Cardiol 2005;95:1117–19.
- Junger J, Shellberg D, Muller-Tasch T et al. Depression increasingly predicts mortality in the course of congestive heart failure. Eur J Heart Fail 2005;7:261–7.
- Faris R, Purcell H, Henein MY et al. Clinical depression is common and significantly associated with reduced survival in patients with non-ischaemic heart failure. Eur J Heart Fail 2002;4:541–51.
- Taylor J, Stott DJ. Chronic heart failure and cognitive impairment: co-existence of conditions or true association? Eur Heart J 2002;4:7–9.
- Zuccala G, Pedone C, Cesari M et al. The effects of cognitive impairment on mortality among hospitalized patients with heart failure. Am J Med 2003;115:97–103.
- McLennan SN, Pearson SA, Cameron J et al. Prognostic importance of cognitive impairment in chronic heart failure patients: does specialist management make a difference? Eur J Heart Fail 2006;8:494–501.
- Curkendall SM, DeLuise C, Jones JK et al. Cardiovascular disease in patients with chronic obstructive pulmonary disease. Ann Epidemiol 2006;16:63–70.
- Benjamin EJ, Wolf PA, D’Agostino RB et al. Impact of atrial fibrillation on the risk of death. The Framingham Heart Study. Circulation 1998;98:946–52.
- Dries DD, Exner DV, Gersh BJ et al. Atrial fibrillation is associated with an increased risk for mortality and heart failure progression in patients with asymptomatic and symptomatic left ventricular systolic dysfunction: A retrospective analysis of the SOLVD trials. J Am Coll Cardiol 1998;32:695–703.
- Lindenfeld J. Prevalence of anaemia and effects of mortality in patients with heart failure. Am Heart J 2005;149:391–401.
- Kosiborod M, Curtis JB, Wang Y et al. Anaemia and outcome in patients with heart failure. Arch Intern Med 2005;165:2237–44.
- Wolinski FD, Smith DM, Stump TE et al. The sequelae of hospitalization for congestive heart failure among older adults. J Am Geriatr Soc 1997;45:558–63.
- Jaagosild P, Dawson NV, Thomas C et al. Outcomes of acute exacerbations of severe congestive heart failure: quality of life, resource use and survival. Arch Intern Med 1998;158:1081–9.
- Wang R, Mouliswar M, Denman S et al. Mortality of the institutionalized old hospitalized with congestive heart failure. Arch Intern Med 1998;158:2464–8.
- Murray SA, Boyd K, Kendall M et al. Dying of lung cancer or heart failure: prospective qualitative interview study of patients and their carers in the community. BMJ 2002;325:929–32.
