In this regular series ‘ECGs for the fainthearted’ Dr Heather Wetherell will be interpreting ECGs in a non-threatening and simple way. In this issue, we apply the knowledge gained so far to a situation that may be encountered in general practice.

Calling all clinicians…(including psychiatrists). This month we’re going to focus on an issue that is cropping up more and more frequently in primary care, but is of equal relevance to any clinician, whether based in the primary or secondary care setting, as demonstrated by the case scenario below. As you read:
- Imagine that you’re the GP in the hot seat.
- What are you thinking about as the story unfolds?
- What knowledge do you need to make an effective diagnosis?
Case
A 44-year-old man presents to you (his GP) on Monday morning.
He explains that he was taken to A&E after a sudden collapse during which he hit his head at a party on Saturday evening. By the time the paramedics arrived he had already regained consciousness but was taken to A&E as a precaution.
At A&E he recalls that he had blood taken, an electrocardiogram (ECG) and a computed tomography (CT) head scan. He was advised, by the A&E doctor who assessed him that all investigations were normal, and that his transient loss of consciousness was thought to be alcohol induced.
He protested that the ‘party’ was a small family gathering during which he drank very little alcohol. Likewise, he feels it extremely unlikely that anyone would have tampered with his drink (another suggestion made at A&E). Since that evening he has felt fine, but remains very concerned about the cause of his collapse. He tells you he thinks he was dismissed as another ‘drunkard’ by A&E.
You examine him and find his blood pressure is 106/64 mmHg, with normal heart sounds. His pulse is strong and regular. His lung fields are clear.
He has no personal past history of palpitations, or chest pain; and no family history of cardiac problems. His only medication is citalopram, which he has taken since his marriage breakdown a year ago.
You check on the hospital ICE/Path Links systems and note the normal CT scan along with the normal full blood count, glucose, thyroid function tests, and urea and electrolytes (including normal potassium). The hospital ECG is, of course, not available to you, so you agree to perform another in view of his ongoing concern.
Figure 1 shows the ECG you obtain. What does it show?
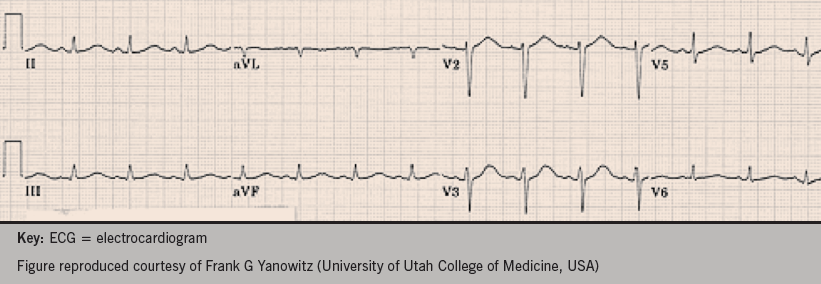
Let’s analyse the ECG methodically to get the answer. Take a few minutes to think about each of the following questions, then read on.
- Q1: What is the rate and rhythm?
- Q2: Is the axis normal?
- Q3: Is the PR interval normal?
- Q4: Is the conduction through the QRS rapid and normal, or delayed?
- Q5: What about the QT interval?
- Q6: Does the QT interval need correcting? (i.e. QTc)
How did you do?
ECG analysis
Q1: The ECG shows sinus rhythm. We have no paper speed on this ECG, but assuming standard paper speed of 25 mm/second (mm/s), we can calculate the rate to be approximately 94 beats per minute (bpm) (i.e. divide 300 by the number of large squares between complexes: 300 ÷ 3.2 = 94).
Q2: The axis is normal.
Q3: The PR interval is normal at four small squares or 0.16 s (normal range 3−5 small squares, or
0.11–0.20 s)
Q4: The QRS interval is normal at <3 small squares, or 0.11 s (normal range 1.5−2.5 small squares, or 0.6−0.11 s)
Q5: The QT interval (from the start of the Q deflection to the end of the T wave) is approximately 10 small squares (0.40 s).
Q6: Does the QT interval on this ECG need correcting?
Yes.
The QT interval is affected by heart rate, in an inversely proportional relationship:
- faster heart rates gives rise to a shorter QT interval (longer once corrected)
- slower heart rates give rise to a longer QT interval (shorter once corrected).
If you happen to catch an ECG at exactly 60 bpm, then you don’t need to calculate a corrected QTc. In the ECG case here, the heart rate is faster than
60 bpm. This can falsely reassure, making the QT interval appear shorter than it actually is.
More often than not, the QT interval needs to be ‘corrected’ for fast or slow heart rates. One of the most popular methods for this correction is using Bazetts formula. Most ECG machines will have calculated this for you.
Bazetts formula:
QTc (ms) = QT interval (ms) divided by the square root of the RR interval(s).
So, if we take the example case above:
QT = 400 ms
RR = 0.56 s (14 mm between complexes x
0.04 s)
So, QTc = 400 ms ÷ √ 0.56 s
= 533 ms (0.53 s)
The normal QTc interval should be 0.36–0.44 s (9–11 small squares).
This ECG reveals a prolonged QT interval.
(Note QT interval duration seen on the ECG is more than 50% of the RR interval – this is a good ‘eye-balling’ indication that it is prolonged in this patient).
As a general rule of thumb:
A QTc of <0.40 s is highly unlikely to be significant
A QTc of >0.47 s (in men) and >0.48 s ( in women) is highly likely to be significant.
A QTc of 0.41−0.46 s is indeterminate, and long QT more difficult to exclude.
A QTc interval of >0.46 s is the frequently used cut-off.
Discussion
Long QT syndrome is known to cause life-threatening ventricular arrhythmias such as ‘torsades de pointes’ (polymorphic ventricular tachycardia) and ventricular fibrillation. These arrhythmias might present as dizzy spells, syncope, blackouts, or sudden death.
Long QT syndrome is caused by mutations in genes, which encode ion channels (potassium and sodium). This leads to a repolarisation abnormality, which predisposes to arrhythmia.
In some individuals, the QT prolongation only occurs after the administration of certain medications. Citalopram is a frequently prescribed antidepressant, and is just one of the more commonly prescribed medications, but more and more antipsychotics are now being prescribed with potential interactions. Safe prescribing advice, specific to citalopram, is detailed by the MHRA in their 2011 update (available at http://www.mhra.gov.uk/Safetyinformation/DrugSafetyUpdate/CON137769), but it is important to emphasise that QT prolongation is usually only seen in the high-dose regimes.
Combinations of two or more such medications increases the risk further.
More about drug-induced QT prolongation and a list of potential drugs to cause it can be found at http://www.ggcprescribing.org.uk/media/uploads/ps_extra/pse_21.pdf
Cardiac events in long QT can be triggered by:
- Vigorous exercise – especially swimming/diving (long QT type 1)
- Auditory stimuli – especially on waking e.g. alarm clock, phone, doorbell (long QT type 2)
- Sleep/rest without arousal (long QT type 3).
Investigations
If long QT is suspected or diagnosed, it is always important to consider electrolyte and endocrine abnormalities.
Serum potassium, magnesium and calcium should always be checked. It’s possible that alcohol may induce a diuresis sufficient to cause a transient potassium loss, and hypokalaemia.
Thyroid function (TFTs) should also be checked. Whilst most patients with long QT will have normal thyroid function, in rare instances, hypothyroidism has given rise to QT prolongation.
Treatment of long QT
- Beta blockers are effective in 80% of cases
- Atrial pacing (if bradycardia induced with beta blocker)
- Implantable cardioverter defibrillator (ICD)
- Mexiletine (long QT3)
This patient, with a history of blackout, should be referred to a cardiologist for further assessment. He may well need an ICD if he turns out to have persistent QT prolongation with no other precipitant. Such a device will deliver a ‘shock’ if the patient has episode of ventricular fibrillation, helping to prevent sudden cardiac death.
Once long QT syndrome is confirmed, it is advisable for any children of the patient to be examined and tested for this condition, as it can be inherited.
Patients with long QT syndrome should avoid participation in competitive sports, strenuous exercise, and stress-related emotions.
Author’s note
This discussion around the QT interval has been kept deliberately simple. In fact, the measurement and assessment of the QT interval is far from straightforward and, like many things in medicine, is fraught with pitfalls. If you’re interested in taking this lesson to another level, you can read more about it in an article by Jo Yaldren (@jyaldren) and Dave Richley (available at https://dl.dropboxusercontent.com/u/84902616/QT article.pdf).
Thank you.
Further information
For GPs interested in progressing their confidence in ECG skills, there is an excellent e-Module available, on which these teachings are based:
And for those of you who are even more e-savvy, don’t forget @ECGclass!
