Ambulatory blood pressure monitoring (ABPM) can confirm diagnosis in essential hypertension (HTN) and mitigate the ‘white-coat’ effect, preventing erroneous antihypertensive therapy. We aimed to collect a case series of over-treated hypertension in the context of ‘white-coat’ effect, resulting in pre-syncopal or syncopal episodes. We collected data retrospectively from patients presenting to syncope clinic between January 2016 and March 2017. ABPM was used at baseline and repeated at three months, following withdrawal of one or more antihypertensive agents.
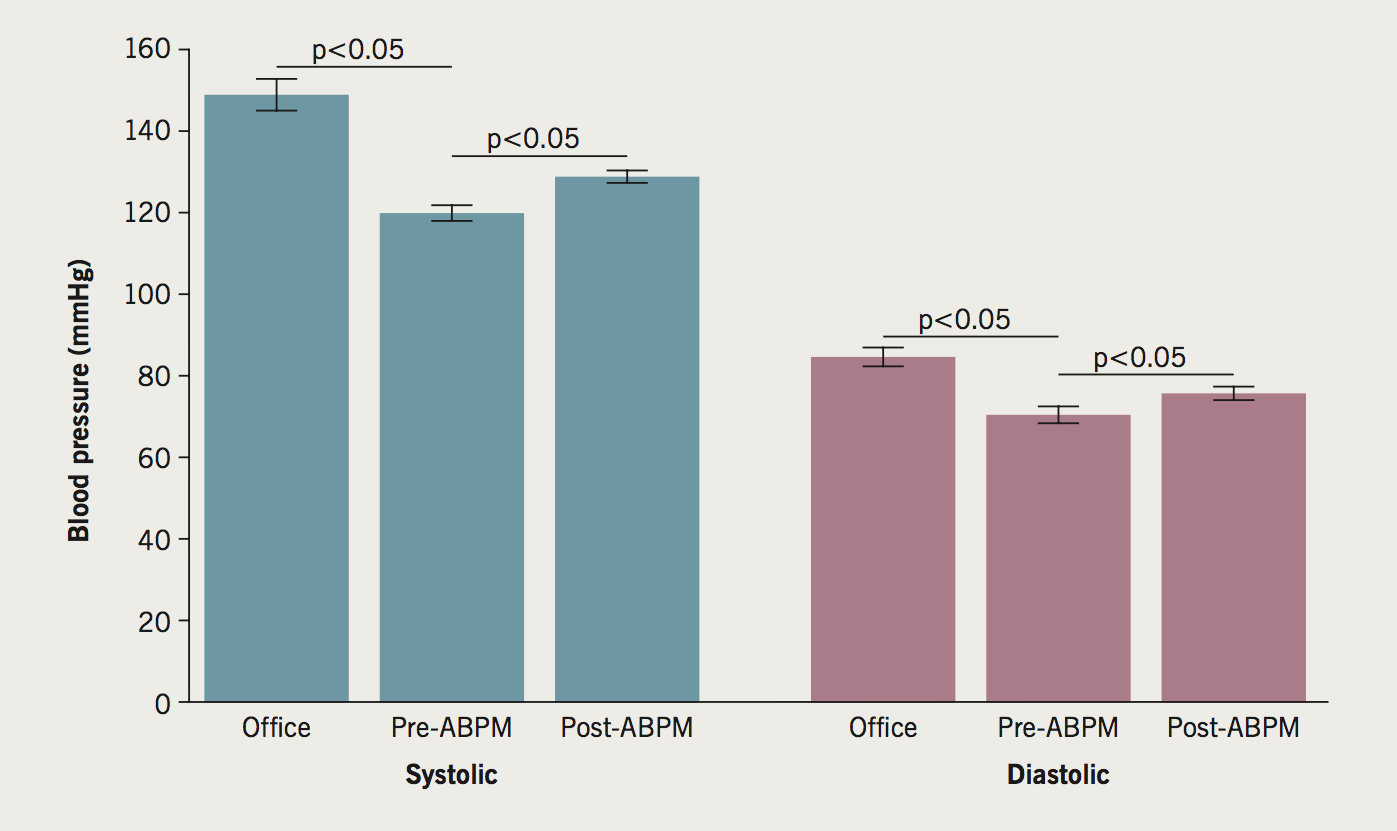
There were 39 patients with orthostatic symptoms of syncope/pre-syncope, previous HTN diagnosis and ‘white-coat’ effect included. Reducing antihypertensive therapy increased daytime ABPM (baseline vs. three months: systolic 119 ± 11 vs. 128 ± 8 mmHg, p<0.05; diastolic 70 ± 9 vs. 76 ± 9 mmHg, p<0.05) and resolved symptoms.
In conclusion, some patients exhibit pre-syncope or syncope due to over/erroneous HTN treatment resulting in orthostatic hypotension. Our findings suggest that reducing antihypertensive medications may resolve symptoms, without rendering them hypertensive.
Introduction
Essential or primary hypertension (HTN), defined as an office blood pressure (BP) ≥140/90 mmHg with no identifiable cause, is a well-documented risk factor for cardiovascular disease, and the most common cardiovascular condition to be seen in primary care.1 It also represents the strongest single modifiable risk factor with regards to future morbidity and mortality.2,3
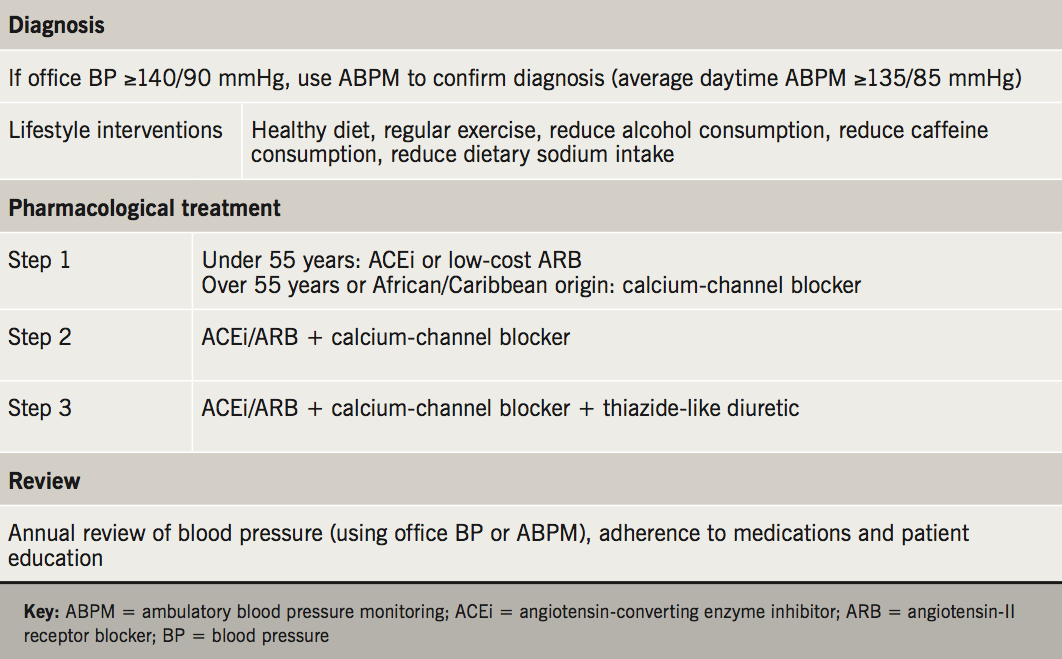
As such, current guidelines advocate pharmacological treatment if lifestyle measures are insufficient. The National Institute for Health and Care Excellence (NICE) clinical guideline for the treatment of HTN recommends step 1 treatment with an angiotensin-converting enzyme (ACE) inhibitor or an angiotensin-II receptor blocker (ARB) in those under 55 years, and a calcium-channel blocker (CCB) or thiazide-like diuretic in those over 55 years, or black people of African or Caribbean family origin of any age. If this fails to control BP despite optimal dose, then recommended step 2 treatment is a combination of ACE inhibitor or ARB and CCB or thiazide-like diuretic. Step 3 treatment consists of ACE inhibitor/ARB with CCB and a thiazide-like diuretic (table 1). The reduction in cardiovascular mortality and morbidity is directly determined by the magnitude of BP reduction regardless of the agent used, with the goal being to reduce the average daytime BP to below 135/85 mmHg.4
However, treatment with antihypertensives can both cause or exacerbate orthostatic hypotension, defined as a reduction of systolic BP of at least 20 mmHg within three minutes of standing compared with the baseline BP in a sitting or supine position.5,6 Indeed, drug-related hypotension is the most frequent cause of orthostatic hypotension among patients presenting to the emergency department with syncope.7
Furthermore, a diagnosis of HTN that is based only on office BP recordings is susceptible to the ‘white-coat’ effect, whereby readings are higher when checked in a healthcare environment than if checked via multiple home BP readings or using average ambulatory BP.8
The use of ambulatory blood pressure monitoring (ABPM) is currently recommended by the NICE guidelines in order to confirm the diagnosis, when office BP readings are persistently elevated (BP readings between 140/90 and 180/110 mmHg), in the absence of end-organ damage. The following ABPM cut-offs have been recommended by NICE, the seventh Joint National Committee (JNC 7) and the European Societies of Hypertension and Cardiology (ESH-ESC) guidelines to diagnose primary hypertension:9,10
- 24-hour average above 130/80 mmHg
- Daytime average above 135/85 mmHg
- Night-time average above 120/70 mmHg.
We hypothesise that a cohort of patients who present with syncope do so as a result of orthostatic hypotension secondary to either over- or erroneously-treated HTN, and that a reduction in the number of antihypertensive agents used can improve their symptoms. We present a case series of over-treated ‘white-coat’ hypertension, resulting in pre-syncopal or syncopal episodes.
Method
Data were collected retrospectively from attendances to a specialist syncope clinic between January 2016 and March 2017 at a teaching hospital within the UK. Patients who presented with orthostatic syncope or pre-syncope while on treatment for HTN, and in whom a comparison between office BP and daytime ABPM demonstrated a white-coat effect (discrepancy of 20/10 mmHg or more between clinic BP and average daytime ABPM) were eligible for inclusion into this study. Patients had one antihypertensive agent withdrawn at initial review, and were followed up by the syncope nurse using telephone appointments at one-month intervals. Those with persistent postural symptoms were discussed by the syncope multi-disciplinary team (MDT), and further antihypertensive therapy was withdrawn if necessary. A repeat ABPM was undertaken three months later to assess for HTN (defined as daytime ABPM ≥135/85 mmHg). Patients were subsequently followed up in clinic to assess for improvement in symptoms.
Patient records were used in order to collate information regarding age, presence of other comorbidities and medication regimens.
Statistical analysis
Data were analysed using Microsoft Excel for Mac 2011. Normality for continuous variables was tested using the histogram method. Normally distributed continuous variables were reported as mean and standard deviation (SD) and those with a non-normal distribution as median and interquartile range (IQR). Statistical comparisons were made using the paired two-tailed student t-test for normally distributed values, with statistical significance defined as a p value less than 0.05.
Results
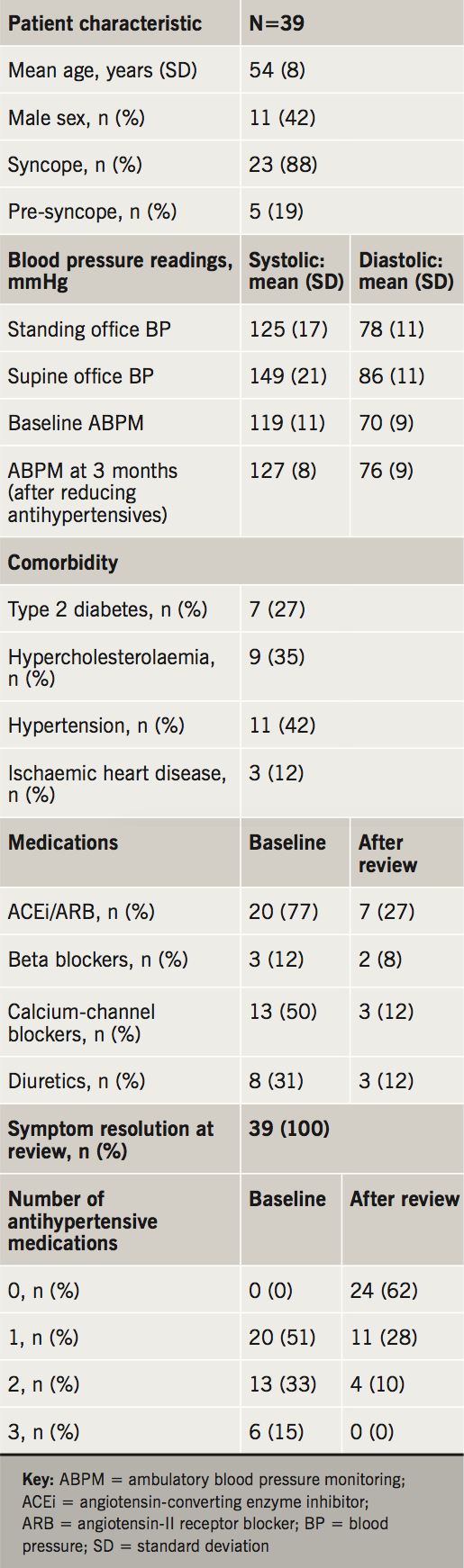
A cohort of 39 patients demonstrated a statistically significant white-coat effect (office BP vs. baseline ABPM: systolic ABPM 148 ± 19 vs. 119 ± 11 mmHg, p<0.05; diastolic ABPM 84 ± 11 vs. 70 ± 9 mmHg, p<0.05) and postural systolic BP drop (≥20 mmHg) at baseline (16 males, age: 55 ± 9 years, systolic office BP 148 ± 19 mmHg, diastolic office BP 84 ± 11 mmHg) (table 2). Definite syncopal episodes were reported by 31 individuals (79%), while the rest reported symptoms consistent with postural pre-syncope/dizziness. Following cessation of ≥1 antihypertensive agent, all patients reported resolution of syncope and/or postural hypotensive symptoms, along with an increase in daytime ABPM readings at three months compared with baseline (baseline vs. three months: systolic ABPM 119 ± 11 vs. 128 ± 8 mmHg, p<0.05; diastolic ABPM 70 ± 9 vs. 76 ± 9 mmHg, p<0.05), but still within normotensive limits (figure 1). Interestingly, 24 patients (62%) remained normotensive despite cessation of all antihypertensive medications, suggesting an erroneous initial diagnosis of hypertension in primary care, which had been based on office BP measurements alone.
Discussion
Adequate treatment of essential hypertension is necessary to reduce cardiovascular risk, and ABPM is recommended in order to both confirm the diagnosis of hypertension, and to exclude the ‘white-coat’ effect, which is seen in up to 30%.1
Our data show that despite a normal baseline ABPM while on antihypertensive treatment, reducing medications resulted in resolution of symptoms without rendering any patients hypertensive (figure 2). Based on these findings we advocate that symptoms of postural hypotension should be sought in patients on antihypertensives during routine medication reviews.
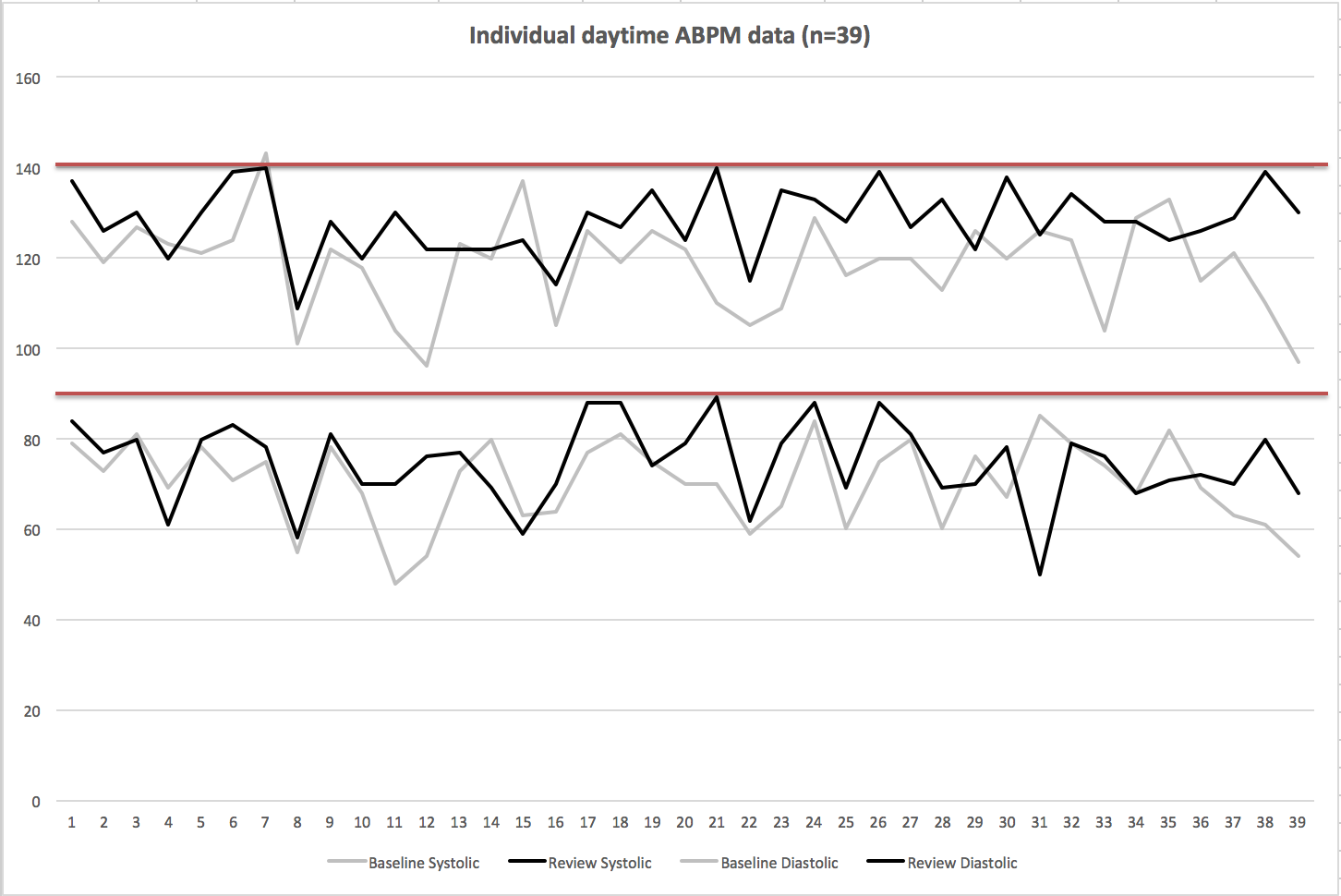
Additionally, in patients with pharmacologically treated hypertension presenting with syncope, postural hypotension should be considered as an iatrogenic cause even in the presence of normal office BP or ABPM. Furthermore, repeat ABPM can be used to confirm that these patients do not go on to become hypertensive following cessation of one or more pharmacological agents. Our data also show the value of using ABPM to confirm the initial diagnosis of hypertension prior to commencing pharmacotherapy, as 62% of our cohort remained normotensive despite cessation of all antihypertensive medications, suggesting an erroneous initial diagnosis.
We also advocate care to be taken in implementing the American Heart Association (AHA) 2017 guideline for the prevention, detection, evaluation, and management of high blood pressure in adults, which defines elevated BP as 120–129/<80 mmHg, and stage 1 hypertension, requiring pharmacological treatment, as office BP 130–139 (systolic) or 80–89 (diastolic) mmHg (for primary prevention, in the presence of a 10-year cardiovascular risk equivalent to >10%).11 This is in comparison to the NICE hypertension guidelines, which endorse pharmacological treatment to be offered in the context of ‘stage 1 hypertension’ (defined by NICE as an office BP >140/90 mmHg) and the presence of a 10-year cardiovascular risk equivalent to >20%.
While Reboussin et al. have shown in a large meta-analysis that the optimal BP target for office systolic BP may be below 130 mmHg, and that such lowering reduces the risk of myocardial infarction, stroke, heart failure, and major cardiovascular events, such stringent goals would nonetheless expose more patients to the potential of developing postural symptoms relating to orthostatic hypotension. This was also shown in the results of the Systolic Blood Pressure Intervention Trial (SPRINT), whereby intensive pharmacological BP reduction (to less than 120 mmHg office systolic BP) did result in lower rates of major cardiovascular events, but was also associated with significantly higher rates of syncope and hypotension.12
Thus, greater emphasis should be placed on lifestyle interventions, such as weight loss, sodium restriction, increased physical activity, reduced alcohol and caffeine intake, smoking cessation and healthy diet (reduced fat and increased fruits, vegetables and grains), both prior to initiation of antihypertensive agents and also in addition to such agents, especially in patients with AHA defined stage 1 hypertension (130–139 or 80–89 mmHg) and no evidence of target organ damage.
Our results corroborate those from several previous studies investigating medication-induced orthostatic hypotension.13,14 However, prior studies have primarily focused on investigating this phenomenon in the context of an elderly population, and have demonstrated medication-induced orthostatic hypotension to be a common cause for syncope and pre-syncope in this cohort. These studies have gone on to highlight antihypertensive and cardiovascular medications to be the most common culprits.15 In one study, pharmacological washout of antihypertensive medications in an elderly cohort resulted in a reduction of symptomatic orthostatic hypotension from 23% to 0% over 12 months.16 In the Discontinuation of Antihypertensive Treatment in Elderly people (DANTE) study, stopping antihypertensive agents resulted in 50% of the cohort being free from orthostatic hypotension at four months.17
The present study is novel in that it is the first to involve the usage of both a baseline ABPM to confirm the presence of ‘white-coat’ hypertension and a repeat ABPM at three months after reducing antihypertensive therapy. Furthermore, it is inclusive of patients of all ages, and, therefore, represents a younger cohort than that traditionally assessed when investigating orthostatic hypotension as a cause of syncope or pre-syncope.
Our findings are limited with respect to the sample size and single-centre data collection. The data were also collected retrospectively, and are, thus, restricted with respect to potential variation in the quality of patient record keeping. There is also a lack of control group to compare whether there is any significant placebo effect to the withdrawal of one or more antihypertensives. Nonetheless, our findings show that doing so is safe and does not render such patients hypertensive.
Conclusion
A cohort of patients present with syncope due to over- or erroneous-treatment of hypertension resulting in orthostatic hypotension. This is likely to be due to their initial diagnosis being made based on office BP readings rather than ABPM. The findings from the present study suggest that when one or more antihypertensive medications are stopped in these patients, their symptoms of syncope or pre-syncope can resolve, while their BP remains within normal limits.
Key messages
- Diagnosis and treatment of hypertension based only on office blood pressure recordings may be susceptible to the ‘white-coat’ effect
- Orthostatic symptoms relating to over- or erroneous-treatment of hypertension are not limited to the elderly population
- The findings from the present study suggest that when one or more antihypertensive medications are stopped in these patients, their symptoms of syncope may resolve, while their blood pressure remains within normal limits
Acknowledgement
HJ and NA have contributed equally to this manuscript and have joint first authorship.
Conflict of interest
None declared.
References
1. Krause T, Lovibond K, Caulfield M, McCormack T, Williams B. Management of hypertension: summary of NICE guidance. BMJ 2011;343:d4891. https://doi.org/10.1136/bmj.d4891
2. Lawes CM, Vander Hoorn S, Rodgers A; for the International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 2008;371:1513–18. https://doi.org/10.1016/S0140-6736(08)60655-8
3. Rapsomaniki E, Timmis A, George J et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014;383:1899–911. https://doi.org/10.1016/S0140-6736(14)60685-1
4. National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. CG127. London: NICE, 2011. Available from: https://www.nice.org.uk/guidance/cg127
5. Milazzo V, Stefano CD, Servo S et al. Drugs and orthostatic hypotension: evidence from literature. J Hypertens 2012;1:104. https://doi.org/10.4172/2167-1095.1000104
6. Mathias CJ. Orthostatic hypotension: causes, mechanisms, and influencing factors. Neurology 1995;45(4 suppl 5):S6–S11.
7. Sarasin FP, Louis-Simonet M, Carballo D et al. Prevalence of orthostatic hypotension among patients presenting with syncope in the ED. Am J Emerg Med 2002;20:497–501. https://doi.org/10.1053/ajem.2002.34964
8. Ben-Dov IZ, Ben-Arie L, Mekler J, Bursztyn M. Reproducibility of white-coat and masked hypertension in ambulatory blood pressure monitoring. Int J Cardiol 2007;117:355–9. https://doi.org/10.1016/j.ijcard.2006.04.088
9. Chobanian AV, Bakris GL, Black HR et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–71. https://doi.org/10.1001/jama.289.19.2560
10. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281–357. https://doi.org/10.1097/01.hjh.0000431740.32696.cc
11. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Coll Cardiol 2017:online first. https://doi.org/10.1016/j.jacc.2017.11.006
12. The SPRINT Research Group. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med 2015;373:2103–16. https://doi.org/10.1056/NEJMoa1511939
13. Kamaruzzaman S, Watt H, Carson C, Ebrahim S. The association between orthostatic hypotension and medication use in the British Women’s Heart and Health Study. Age Ageing 2010;39:51–6. https://doi.org/10.1093/ageing/afp192
14. Fedorowski A, Burri P, Juul-Moller S, Melander O. A dedicated investigation unit improves management of syncopal attacks (Syncope Study of Unselected Population in Malmo – SYSTEMA I). Europace 2010;12:1322–8. https://doi.org/10.1093/europace/euq168
15. Press Y, Punchik B, Freud T. Orthostatic hypotension and drug therapy in patients at an outpatient comprehensive geriatric assessment unit. J Hypertens 2016;34:351–8. https://doi.org/10.1097/HJH.0000000000000781
16. Fotherby MD, Potter JF. Orthostatic hypotension and anti-hypertensive therapy in the elderly. Postgrad Med J 1994;70:878–81. https://doi.org/10.1136/pgmj.70.830.878
17. Moonen JE, Foster-Dingley JC, de Ruijter W et al. Effect of discontinuation of antihypertensive medication on orthostatic hypotension in older persons with mild cognitive impairment: the DANTE Study Leiden. Age Ageing 2016;45:249–55. https://doi.org/10.1093/ageing/afv199
