Reviewing this topic, Professor Lewis J Rubin, University of California, San Diego, US, looked at both the successes and failures of the past 20 years. He described how, as little as two decades ago, there was no treatment algorithm for PAH: “we had absolutely no understanding of the fundamental mechanisms responsible for the development of PAH” and approaches to treatment were based on a simplistic extrapolation from systemic hypertension and left-sided heart disease.
Since then, there has been a steady exploration of the molecular mechanisms underlying PAH, which has led to development of effective targeted therapeutic options such as endothelin receptor antagonists and prostacyclin derivatives. In Professor Rubin’s view, these options represent a major success, but he hoped that there would be further progress. Many patients may not respond to these therapies, and it remains a serious and life-threatening disease.
The characterisation of PAH into its clinical, pathobiological and epidemiological components has provided the opportunity to intervene therapeutically and to delay disease progression. Three factors appear to be associated with the increased pulmonary vascular resistance seen in PAH, including vasoconstriction, remodelling of the pulmonary vessel wall and thrombosis in situ. Early catheterisation studies led to the clinical characterisation of PAH, while landmark epidemiological studies such as the National Institutes of Health (NIH) Registry1 have helped to define the natural history of this disease and its risk factors and to define treatment targets.
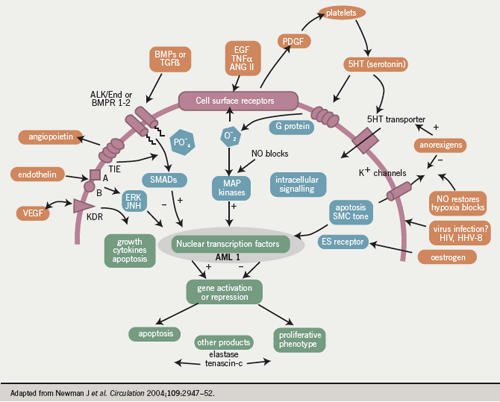
The next pathobiological phase identified the role of endothelial dysfunction, demonstrating impaired production of prostacyclin and nitric oxide (NO) and overproduction of endothelin. For the first time, this offered pathobiological targets for the treatment of this disease. Similarly, the concept of vascular growth and proliferation meant that PAH was viewed not as a single dynamic disease but rather as a much more complex process. Finally, a further area of critical importance was identification of the role of genetics in PAH, and potentially in other forms of pulmonary hypertension.
The natural history of primary pulmonary hypertension (PPH) was evaluated in the NIH Registry from 1981-87.1 Reporting just over 20 years ago, it showed that of the 194 patients included in the study, 63% were female and 37% were male, and the mean age was 36 years. Median untreated survival after diagnosis was 2.8 years. It also highlighted “the haemodynamic severity of the disease relative to the normal range”. (Pulmonary hypertension [PH] today is defined by a mean pulmonary artery pressure >25 mmHg at rest or >30 mmHg with exercise.)2
By the time patients presented, they had advanced disease and the Registry findings1 also underscored the fact that there was an unacceptable delay from the onset of symptoms to the time of diagnosis, said Professor Rubin. This was true 20 years ago and “unfortunately it’s still true today. It is one of our major failings that we still see patients present with advanced disease. We need to have a major focus on early diagnosis and early treatment…which is becoming more and more feasible”.
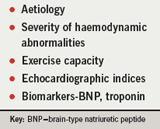
Some forms, such as systemic sclerosis-associated pulmonary arterial hypertension (SScPAH), carry an even worse prognosis than that of patients with idiopathic PAH.3 We should be able to identify such at-risk patients earlier if we invoke the right approaches to managing the condition.4 Another important element in disease management is characterising the limitations and abnormalities that patients have. There are a number of determinants or markers of survival in PAH(table 1). The six-minute walk distance, for example, has been used as an objective measure of exercise capacity and Professor Rubin stated that those who can walk longer do considerably better than those who cannot. Also, exercise distance improves with treatment. Haemodynamic markers include indices of right heart function, notably right atrial pressure and mean pulmonary artery pressure (mPAP). Echocardiographic indices include right atrial size. Useful biomarkers such as brain natriuretic peptide (BNP) are now being incorporated into management paradigms and also as end points in clinical trials.
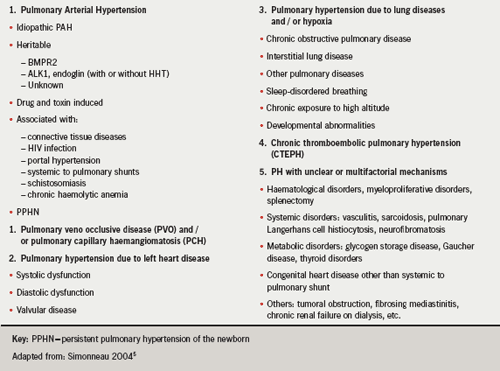
PAH classification
There have been major developments in the classification of pulmonary hypertension since the First World Symposium on Diagnostic Classification in Geneva in 1973, which basically divided the disease into primary and secondary pulmonary hypertension, depending on whether or not the patient had identifiable causes or risk factors.4 Things have moved on to a more complex classification.5 Although some may regard this classification as too complex, Professor Rubin believes that the classification is useful because it serves as the differential diagnosis, which is critical for assessing patients with pulmonary hypertension, who may share certain features in common or be quite different (table 2). This classification is a living document, he explained; it changes, and continues to change, as our thinking and experience evolve.
PAH pathophysiology
PAH is largely a vasoproliferative disease, a process which is characterised by growth and proliferation of all the layers of the vessel wall.6 We have learned much about what may contribute to the transition from the normal to the remodelled pulmonary vessel. Studies have demonstrated a variety of abnormalities which are intrinsic to the smooth muscle cell or the endothelial cell, requiring cross-talk between the two cells. The hallmark is proliferation and probably altered apoptosis. Possibly, in the early phase of the disease, an intrinsic abnormality of contraction may occur as well, although this has not been confirmed.
Three important pathways have been identified in pulmonary hypertension (table 3).7
These pathways are known from animal studies, and clinical trials have shown that targeting these three pathways does lead to improvements in patients with PAH.8-12
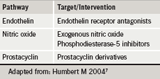
The endothelin pathway, or the so-called overproduction of endothelin, can be targeted with endothelin receptor antagonists. Underproduction of prostacyclin is addressed by the use of a prostacyclin analogue; and targeting underproduction of nitric oxide (NO) by augmenting the signal for its production and inhibiting its breakdown via a phosphodiesterase (PDE) inhibitor. There is of course a “whole variety of other pathways” which have been suggested to be abnormal and implicated in PAH, and many abnormalities have been demonstrated. The challenge for the future is to prioritise these and to try and gain an understanding of which of these abnormalities are causative.
Conflict of interest
LJR serves on advisory committees for Actelion, Pfizer, MD Primer, Encysive, Novartis and Gilead.
References
- D’Alonzo GE, Barst RJ, Ayres SM et al. Survival in patients with primary pulmonary hypertension. Results from a national prospective registry. Ann Intern Med 1991;115:343–9.
- Galie N, Torbicki A, Barst R et al. Guidelines on diagnosis and treatment of pulmonary arterial hypertension. The Task Force on Diagnosis and Treatment of Pulmonary Arterial Hypertension of the European Society of Cardiology.Eur Heart J 2004;25:2243–78.
- Kawut SM, Taichman DB et al. Hemodynamics and survival in patients with pulmonary arterial hypertension related to systemic sclerosis. Chest 2003;123:344–50.
- Hatano S, Strasser R, Eds. Primary pulmonary hypertension. World Health Organization, Geneva, 1975.
- Simonneau G, Galie N, Rubin L et al. Clinical classification of pulmonary arterial hypertension. J Am Coll Cardiol 2004;43:S5–S12.
- Humbert M, Morrell N, Archer S et al. Cellular and molecular pathobiology of pulmonary arterial hypertension. J Am Coll Cardiol 2004;43:S13–S24.
- Humbert M, Sitbon O, Simonneau G. Treatment of pulmonary arterial hypertension. N Engl J Med 2004;351:1425–36.
- Galie N, Olschewski H, Oudiz RJ et al. Ambrisentan for the treatment of pulmonary arterial hypertension. Results of the ARIES Study 1 and 2. Circulation 2008;117:3010–19.
- Rubin LJ, Badesch DB, Barst RJ et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med 2002;346:896–903.
- Barst RJ, Langleben D, Frost A. Sitaxsentan therapy for pulmonary arterial hypertension. Am J Respir Crit Care Med 2004;169:441–7.
- Galie N, Ghofrani HA, Torbicki A et al. Sildenafil citrate therapy for pulmonary arterial hypertension. N Engl J Med 2005;353:2148–57.
- Barst RJ, Rubin LJ, Long WA et al. A comparison of continuous intravenous epoprostenol (prostacyclin) with conventional therapy for primary pulmonary hypertension. N Engl J Med 1996; 334:296–302.
