False-negative results either from balanced ischaemia or from failure to induce optimal hyperaemia is a known limitation of vasodilator myocardial perfusion imaging (MPI). We sought to identify the prevalence of false-negative results in the kidney transplant population and to identify the risk factors predictive of false-negative MPI results at our institution.
We retrospectively studied 133 consecutive patients who were referred to us for pre-operative evaluation. Mean age was 56 years and 70% of the subjects were males. All patients who underwent vasodilator MPI and computed tomography coronary angiography (CTCA) were included.
In the studied population, false-negative vasodilator MPI test result prevalence was around 13%. In uni-variable and multi-variable analysis, diabetes and cardiovascular disease (CVD) were predictive of false-negative vasodilator MPI testing results. CTCA had a positive-predictive value (PPV) of 82%.
In conclusion, false-negative results, either from balanced ischaemia or from failure to induce optimal hyperaemia, are a major problem in the pre-operative evaluation of renal transplant patients when the vasodilator MPI test is used. CTCA could be a useful imaging modality in this patient population. We found that diabetes and CVD are significantly associated with false-negative MPI results.
Introduction
Cardiovascular disease (CVD) is the leading cause of morbidity and mortality in patients with end-stage renal disease (ESRD), and in those after renal transplant.1,2 The pre-operative cardiovascular risk assessment is critical prior to renal transplant surgery to ensure appropriate patient selection, and to prevent adverse effects on one- and three-year patient and graft survival. In addition, these patients are closely monitored for over three years and any events are reported to the United Network for Organ Sharing. The pre-operative assessment is done based on the American Heart Association and the American College of Cardiology Foundation scientific statement:2 “Noninvasive stress testing may be considered in kidney transplantation candidates with no active cardiac conditions based on the presence of multiple coronary artery disease (CAD) risk factors regardless of functional status. Relevant risk factors among transplantation candidates include diabetes mellitus, prior cardiovascular disease, more than 1 year on dialysis, left ventricular hypertrophy, age greater than 60 years, smoking, hypertension, and dyslipidemia. The specific number of risk factors that should be used to prompt testing remains to be determined, but the committee considers 3 or more as reasonable (Class IIb; Level of Evidence C)”. Most common non-invasive stress-testing modalities include dobutamine stress echo (DSE) or myocardial perfusion imaging (MPI). The diagnostic accuracy of these tests vary; sensitivity ranges from 0.29 to 0.92 for MPI and 0.44 to 0.89 for DSE, while specificity ranges from 0.67 to 0.89 for MPI and 0.71 to 0.94 for DSE.2 MPI accuracy could be affected by the presence of false-negative results.
Computed tomography coronary angiography (CTCA) provides additional anatomic information, such as the presence of obstructive disease, when MPI is negative. CTCA is being used for risk stratification in non-chronic kidney disease patients.3,4 Winther et al. showed that CTCA is a reliable test with a high sensitivity and negative-predictive value for diagnosing obstructive CAD before kidney transplantation.5 The aim of our study was to identify the prevalence of false-negative results in our kidney transplant population and to identify risk factors predictive of false-negative MPI test results.
Methods
Study site and participants
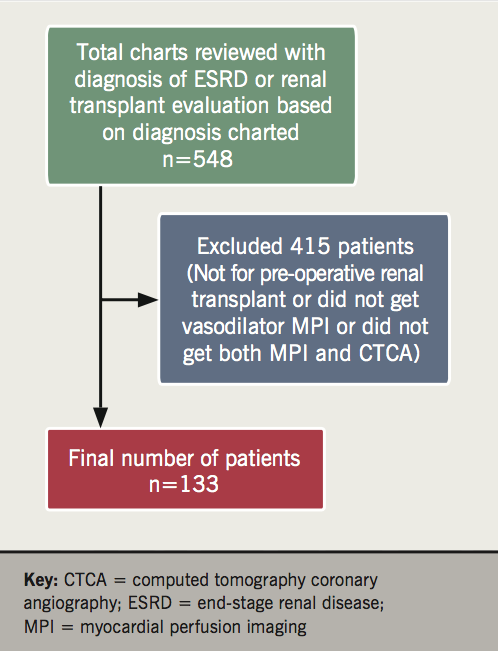
This study was a retrospective health information review that was performed over a 60-month period from 1 January 2009 to 31 December 2013. The study site was a single academic cardiology clinic in metropolitan southern Nevada, USA. We reviewed the charts of consecutive patients with the diagnosis of kidney transplant or pre-operative evaluation for kidney transplant in our electronic medical records during the study period (figure 1).
Inclusion and exclusion criteria
Inclusion criteria:
- Patients with a diagnosis of ESRD on dialysis referred for pre-operative cardiac evaluation.
- Patients who had a pre-operative cardiac evaluation for kidney transplantation with vasodilator stress MPI and CTCA as deemed necessary by the cardiologist, depending on the functional status. Invasive coronary angiogram was performed if indicated.
Exclusion criteria:
- Age less than 18 years.
- Patients who did not undergo the pre-operative cardiac evaluation for kidney transplantation with vasodilator stress MPI and CTCA.
Tests
CTCA was done in patients with multiple risk factors and as deemed necessary by the cardiologist. False-negative results have been attributed to an impaired vasodilatory response to adenosine or due to balanced ischaemia in the dialysis population.6 Computed tomography scans were performed using the standard protocol as per Society of Computed Cardiac Tomography guidelines.7 CTCA test is considered abnormal for obstructive CAD if the severity of stenosis is ≥70% (reduction in luminal diameter) by visual estimate.
Invasive coronary angiogram is considered abnormal for obstructive CAD if the severity of stenosis is ≥70% (reduction in luminal diameter) by visual estimate. Vasodilator MPI was performed with regadenoson and 99mTechnetium-sestamibi using standard protocols approved by the American Society of Nuclear Cardiology.8 MPI is considered abnormal if there is a fixed or reversible perfusion defect. We included both types of perfusion defects, as the fixed defects were also associated with increased cardiac death.9 Prognostically significant CAD was defined as presence of significant left main or proximal left anterior descending artery (LAD) or multi-vessel disease (MVD), with or without left ventricular dysfunction.
Study measurements and outcomes
We collected the demographic and clinical characteristics of each patient. Demographic variables included age, gender, race and ethnicity. Clinical variables were history of diabetes mellitus, hypertension, cardiovascular disease and hyperlipidaemia. Age was treated as a continuous variable and other variables were treated as categorical variables: gender (male vs. female), race or ethnicity (white vs. non-white), diabetes (yes or no), hypertension (yes or no), CVD (yes or no), and hyperlipidaemia (yes or no). Resource of the data gathering was self-reported information by the patients (gender and race or ethnicity) and historical information (age, diabetes, hypertension, CVD and hyperlipidaemia) from the electronic health records of the patients. We measured the prevalence of false-negative vasodilator MPI results and the positive-predictive value of CTCA. We also estimated the predictors of false negativity of vasodilator MPI testing.
Statistical analysis
Positive-predictive value was defined as the true positive/(true positive + false positive). False negativity was defined as false negative/(true positive + false negative). To estimate predictors of false negativity of MPI testing, we also performed logistic regression. Each demographic and clinical variable were independent variables and entered simultaneously in a multi-variate logistic regression model. Unadjusted odds ratios (OR) and adjusted OR with corresponding 95% confidence intervals (CI) were computed. There was no female patient with false negativity and, hence, the gender variable was removed from the final model. Pearson correlation of the independent variables was used to determine whether any variables highly correlated and, therefore, were not recommended for inclusion in the same regression model. A high correlation was defined as a correlation coefficient >0.7.10 We could not find high correlation between independent variables. Hosmer and Lemeshow test was applied for testing appropriateness of model fitness for multi-variate logistic regression.11 All statistical analyses were performed using SPSS statistical software version 24 (IBM Analytics Inc., Amonk, New York, USA, 2015). All reported p values were two-tailed and a p value <0.05 was considered statistically significant.
Results
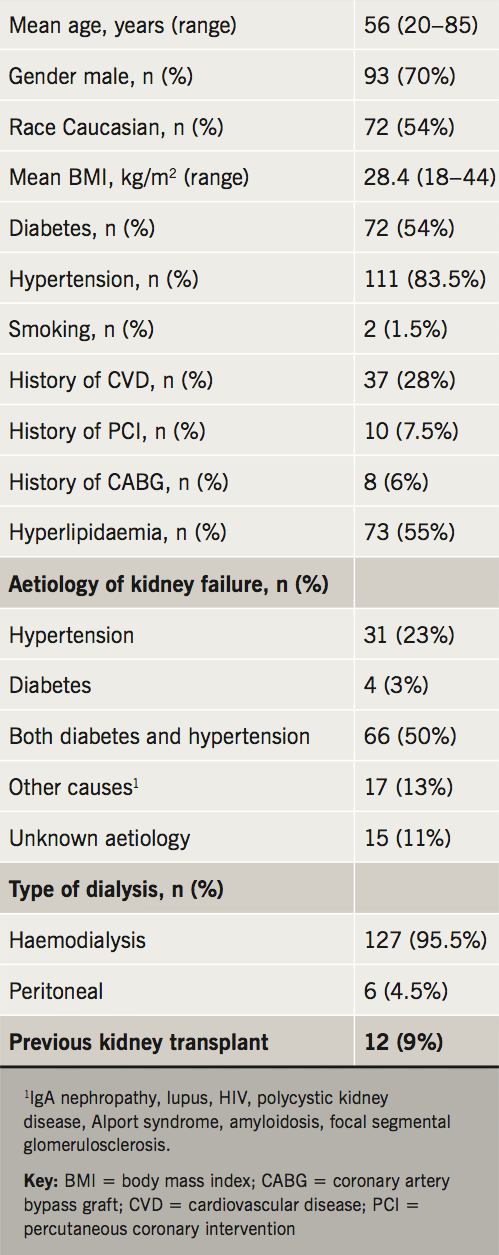
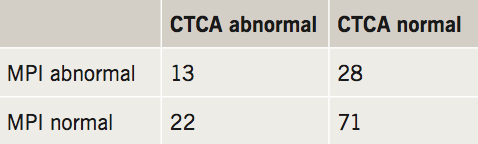
A total of 133 patient charts were reviewed. Baseline characteristics of the patients are summarised in table 1. Mean age was 56 years (range 20 to 85, standard deviation [SD] 12.9) and 70% of them were males. Participants had the following comorbidities: hypertension (83.5%), hyperlipidaemia (54.9%), diabetes (54.1%), and CVD (27.8%). Diabetes and hypertension were the most common aetiologies for ESRD in this study. Out of the 133 patients, 13 patients had abnormal results from both MPI and CTCA tests, while 71 patients had normal results from both MPI and CTCA tests. There were 22 patients (16.5%) with normal MPI and abnormal CTCA for obstructive CAD. All of these 22 patients had coronary angiogram. It confirmed the presence of obstructive CAD found on CTCA in 18 patients (tables 2 and 3), yielding a positive-predictive value (PPV) of 82%. Among these 18 patients, 13 patients had multi-vessel CAD and five patients had one-vessel or two-vessel disease. All patients with multi-vessel disease underwent coronary artery bypass grafting (CABG) surgery and patients with one-vessel or two-vessel disease underwent percutaneous coronary intervention (PCI) with stents, as per guidelines. Fractional flow reserve (FFR) was not used in this study as PCI was not performed in patients with one-vessel or two-vessel disease with lesion stenosis <70%. American College of Cardiology guidelines did not recommend it for lesion with stenosis ≥70% during the study time period.12

In logistic regression models, diabetes (unadjusted OR 2.24, 95%CI 1.51 to 14.92, p<0.01; adjusted OR 4.32; 95%CI 1.08 to 17.24, p=0.03) and CVD (unadjusted OR 4.60, 95%CI 1.02 to 20.79, p=0.04; adjusted OR 6.47, 95%CI 1.34 to 31.08, p<0.01) were associated with false-negative stress MPI results (table 4). Hosmer and Lemeshow test validated freedom from violation for multi-variate logistic regression (χ2=7.362; df=8; p=0.498).

Discussion
In this study, we found that balanced ischaemia or failure to induce optimal hyperaemia accounting for false-negative results was a significant problem in the pre-operative evaluation of kidney transplant patients. Its prevalence was 13.5%. Failure to induce optimal hyperaemia was described by Ragosta et al. in ESRD patients.6 Wang et al. showed that MPI has low sensitivity (69%) in this patient population.13 A recent paper by Gomez et al. describing the role of MPI in ESRD patients suggested that heart rate response to vasodilator stress provided incremental risk stratification.14 This is an important finding in patients evaluated for kidney transplantation with negative MPI results.
In our study, in the patients with false-negative results, three-vessel disease was found in 13 patients and one-vessel or two-vessel disease was found in five patients, reinforcing the fact that, apart from balance ischaemia, vasodilators may not achieve optimal hyperaemia in dialysis patients. As all the patients underwent coronary angiogram when both MPI and CTCA or CTCA were abnormal, we were able to calculate PPV of CTCA, which was 82%. In the ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) and CORE 64 (Coronary Artery Evaluation Using 64-Row Multidetector Computed Tomography Angiography) studies, PPV of CTCA ranged from 64% to 91%.15,16 So, with incremental testing, patients with false-negative MPI results were identified. Winther et al. also showed that a noninvasive approach with use of either CTCA or a combination of CTCA and single photon emission computed tomography (SPECT) to rule out obstructive CAD seems recommendable in kidney transplant candidates.5
However, one of the limitations of use of CTCA in this patient population is the impact of high calcium, leading to high false-positive results. This problem could be mitigated with CTCA fractional flow reserve (FFR),17,18 or by hybrid imaging.5 Another limitation is cost, and radiation would limit the routine application of hybrid testing or CTCA as the primary modality of evaluation at this time. Although, one could argue that with prospectively electrocardiogram (ECG)-triggered CTCA, radiation can be reduced to less than 2 mSv.19
Nonetheless, in order to find out who would benefit from the above strategy, we did a logistic regression analysis. Our analysis identified diabetes and CVD as predictors of false negativity of MPI testing. Larifla et al. showed that diabetes, male gender and history of CVD are the strongest predictors of multi-vessel disease in Afro-Caribbean patients.20
Study limitations
We acknowledge several limitations of the current study. First, our data were collected from a single academic institution. Most of the study participants were from a metropolitan area and were referred for pre-operative evaluation. Referral bias as selection bias could occur as depicted in a previous stress test study.21 Second, resources of data gathering were from electronic health records which relied on healthcare providers data input. Therefore, inter-observer or recall bias potentially occurred. Third, the study sample size was limited as it was a single-centre experience.
Conclusion
Negative vasodilator MPI test can be misleading in the pre-operative evaluation of ESRD patients awaiting kidney transplant as it has prognostic implications. We found that diabetes and CVD were significantly associated with the presence of prognostically significant CAD, despite negative MPI results. MPI or CTCA can be an initial modality for diagnosis of CAD in this patient population. However, in patients with a history of diabetes and CVD, CTCA or hybrid testing is probably more accurate. Larger prospective studies are warranted to confirm our findings.
Key messages
- Vasodilator myocardial perfusion imaging (MPI) testing has a major limitation in the pre-operative evaluation of renal transplant patients, when used. Computed tomography coronary angiography (CTCA) could be a useful imaging modality in this patient population
- We found that diabetes and cardiovascular disease are significantly associated with false-negative MPI results
Conflicts of interest
None declared.
Study funding
None.
Study approval
This study was approved by the Institutional Review Board of University Medical Center of Southern Nevada.
References
1. Pilmore H, Dent H, Chang S, McDonald SP, Chadban SJ. Reduction in cardiovascular death after kidney transplantation. Transplantation 2010;89:851–7. https://doi.org/10.1097/TP.0b013e3181caeead
2. Lentine KL, Costa SP, Weir MR et al. Cardiac disease evaluation and management among kidney and liver transplantation candidates: a scientific statement from the American Heart Association and the American College of Cardiology Foundation. J Am Coll Cardiol 2012;60:434–80. https://doi.org/10.1016/j.jacc.2012.05.008
3. Catalán P, Leta R, Hidalgo A et al. Ruling out coronary artery disease with noninvasive coronary multidetector CT angiography before noncoronary cardiovascular surgery. Radiology 2011;258:426–34. https://doi.org/10.1148/radiol.10100384
4. Fathala A. Coronary computed tomography angiography for risk stratification before noncardiac surgery. Ann Card Anaesth 2016;19:31. https://doi.org/10.4103/0971-9784.173017
5. Winther S, Svensson M, Jørgensen HS et al. Diagnostic performance of coronary CT angiography and myocardial perfusion imaging in kidney transplantation candidates. JACC Cardiovasc Imaging 2015;8:553–62. https://doi.org/10.1016/j.jcmg.2014.12.028
6. Ragosta M, Samady H, Isaacs RB, Gimple LW, Sarembock IJ, Powers ER. Coronary flow reserve abnormalities in patients with diabetes mellitus who have end-stage renal disease and normal epicardial coronary arteries. Am Heart J 2004;147:1017–23. https://doi.org/10.1016/j.ahj.2003.07.029
7. Abbara S, Arbab-Zadeh A, Callister TQ et al. SCCT guidelines for performance of coronary computed tomographic angiography: a report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2009;3:190–204. https://doi.org/10.1016/j.jcct.2009.03.004
8. Dorbala S, Di Carli MF, Delbeke D et al. SNMMI/ASNC/SCCT guideline for cardiac SPECT/CT and PET/CT 1.0. J Nucl Med Off Publ Soc Nucl Med 2013;54:1485–507. https://doi.org/10.2967/jnumed.112.105155
9. Rabbat CG, Treleaven DJ, Russell JD, Ludwin D, Cook DJ. Prognostic value of myocardial perfusion studies in patients with end-stage renal disease assessed for kidney or kidney-pancreas transplantation: a meta-analysis. J Am Soc Nephrol 2003;14:431–9. https://doi.org/10.1097/01.ASN.0000047560.51444.3A
10. Tabachnick BG, Fidell LS. Using Multivariate Statistics 6th Edition [Internet]. Pearson, 2013. Available from: https://www.pearsonhighered.com/program/Tabachnick-Using-Multivariate-Statistics-6th-Edition/PGM332849.html
11. Hosmer DW, Lemeshow S, Sturdivant RX. Applied Logistic Regression. 3rd Edition. Hoboken, USA: John Wiley & Sons, Inc., 2013.
12. Levine GN, Bates ER, Blankenship JC et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2011;124:e574–e651. https://doi.org/10.1161/CIR.0b013e31823a5596
13. Wang LW, Fahim MA, Hayen A et al. Cardiac testing for coronary artery disease in potential kidney transplant recipients: a systematic review of test accuracy studies. Am J Kidney Dis 2011;57:476–87. https://doi.org/10.1053/j.ajkd.2010.11.018
14. Gomez J, Fughhi I, Campagnoli T, Ali A, Doukky R. Impact of integrating heart rate response with perfusion imaging on the prognostic value of regadenoson SPECT myocardial perfusion imaging in patients with end-stage renal disease. J Nucl Cardiol 2017;24:1666–71. https://doi.org/10.1007/s12350-016-0497-0
15. Budoff MJ, Dowe D, Jollis JG et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 2008;52:1724–32. https://doi.org/10.1016/j.jacc.2008.07.031
16. Miller JM, Rochitte CE, Dewey M et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008;359:2324–36. https://doi.org/10.1056/NEJMoa0806576
17. Min JK, Leipsic J, Pencina MJ et al. Diagnostic accuracy of fractional flow reserve from anatomic CT angiography. JAMA 2012;308:1237–45. https://doi.org/10.1001/2012.jama.11274
18. Koo B-K, Erglis A, Doh J-H et al. Diagnosis of ischemia-causing coronary stenoses by noninvasive fractional flow reserve computed from coronary computed tomographic angiograms. Results from the prospective multicenter DISCOVER-FLOW (Diagnosis of Ischemia-Causing Stenoses Obtained Via Noninvasive Fractional Flow Reserve) study. J Am Coll Cardiol 2011;58:1989–97. https://doi.org/10.1016/j.jacc.2011.06.066
19. Tan SK, Yeong CH, Ng KH, Abdul Aziz YF, Sun Z. Recent update on radiation dose assessment for the state-of-the-art coronary computed tomography angiography protocols. PloS One 2016;11:e0161543. https://doi.org/10.1371/journal.pone.0161543
20. Larifla L, Armand C, Velayoudom-Cephise F-L et al. Distribution of coronary artery disease severity and risk factors in Afro-Caribbeans. Arch Cardiovasc Dis 2014;107:212–18. https://doi.org/10.1016/j.acvd.2014.03.003
21. Miller TD, Hodge DO, Christian TF, Milavetz JJ, Bailey KR, Gibbons RJ. Effects of adjustment for referral bias on the sensitivity and specificity of single photon emission computed tomography for the diagnosis of coronary artery disease. Am J Med 2002;112:290–7. https://doi.org/10.1016/S0002-9343(01)01111-1
